Pediatric Surgery Training Programs
You’re in the right place
Looking for a pediatric surgery training program? APSA can help; learn about the characteristics of the ideal candidate and view current listings from major research institutions around the country and Canada.
Association of Pediatric Surgery Training Program Directors
KuoJen Tsao, MD – President
McGovern Medical School at UTHealth,
Houston, TX
kuojen.tsao@uth.tmc.edu
Mark Mazziotti, MD – Secretary
Texas Children’s Hospital,
Baylor College of Medicine
Houston, TX
mazziott@bcm.edu
Alberta Children's Hospital/University of Calgary
Last updated: 31/10/2024
Program web page URL: https://cumming.ucalgary.ca/departments/surgery/sections/pediatric-surgery/education
The University of Calgary Pediatric Surgery Fellowship Program welcomes well-rounded candidates who wish to become experts and leaders in our field worldwide. The program will provide the clinical exposure required to be facile in the evaluation and management of the full breadth of neonatal and pediatric general surgical conditions. In accordance with the objectives of training outlined by the Royal College of Physicians and Surgeons of Canada, trainees will achieve competence as medical experts, communicators, collaborators, managers, health advocates, scholars, and professionals. Candidates will be well supported and mentored to achieve their personal and career goals.
Strengths: Faculty from a variety of training backgrounds, with expertise and leadership positions in quality/patient safety, basic sciences research, clinical/translational/outcomes research, and education. Lack of residents and Fellows in other pediatric surgical training programs provides ample opportunity to participate in ENT and Urology cases. Strong partnerships with other care providers across disciplines and specialties. The ECMO program is one-of-a-kind, where cannulation is completed on site, but the patient is then transferred for the run to be completed at Stollery Children’s Hospital.
Weaknesses: Global health experience not included in current curriculum. Pediatric cardiac surgery care exclusively at Stollery Children’s Hospital in Edmonton.
Institution Information
Alberta Children’s Hospital
Calgary, AB Canada
Number of beds: 141
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
The current Alberta Children’s Hospital (ACH) opened in 2006, and is the largest children’s hospital in the Canadian Prairies. Its catchment area includes Southern Alberta and extends to southeastern British Columbia and southwestern Saskatchewan. It is an accredited level 1 pediatric trauma centre, and also has a rescue ECLS program. ACH program development has led to the realization of specialized teams and multidisciplinary clinics which care for intestinal rehabilitation, congenital diaphragmatic hernia, esophageal atresia/tracheoesophageal atresia, oncology, and pediatric complex care patients. The general surgery service performs ~1300-1500 cases per year, and the full department performs in excess of 10,000 cases per year across the breadth of pediatric subspecialties.
The Alberta Children’s Hospital Research Institute has over 150 members, and offers many funding opportunities to support innovation and advancement of pediatric care. Alberta Children’s Hospital is much beloved and championed by the local community, as evidenced by the annual Caring for Kids Radiothon fundraiser, which in 2019 raised a record-breaking total of $6.6 million.
Faculty Information
Program Director: Andrea Lo
Program Administrator: Bibiana Silva
bibiana.silva@ahs.ca
403-955-2271
Faculty:
P. Paul Beaudry, MD, MSc, FRCSC
Mary Brindle, MD, MPH, FRCSC
Oluwatomilayo (Tito) Daodu, MD, FRCSC
Andrea Lo, MD, FRCSC
Steven Lopushinsky, MD, MSc, FRCSC
Natalie Yanchar, MD, MSc, FRCSC
Fellow Information
Number of fellows: one per year
The University of Calgary participates in the NRMP Match q2y, alternating with a nonMatch trainee.
Current fellow(s):
Robin Wigen
Catalina Ceballos
Previous 5 fellows:
Abdullah Alenazi
2024
Prince Mohammed Medical City
Al Jouf, Saudi Arabia
Brittany Hasty
2024
University of California San Francisco
Oakland, CA
William Hammond
2022
Eastern Idaho Regional Medical Center
Idaho Falls, ID
Mercedes Pilkington
2021
Pediatric Surgeon, The Hospital for Sick Children
Toronto, Ontario
Oluwatomilayo (Tito) Daodu
2020
Pediatric Surgeon, Alberta Children’s Hospital
Calgary, Alberta
Curriculum Information
Block schedule
1st year off-service blocks in NICU and PICU
Call Schedule
1st year: home call no more than q4
2nd year: home call no more than q4
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy:
1st year Fellow attends Transition to Fellowship (Boot Camp), PALS, and APSA
2nd year Fellow attends CAPS, and Transition to Practice course
Each Fellow will also attend the St. Jude’s Oncology course, and one of the Colorectal courses, once each during their training.
The above-named courses/meetings will be reimbursed by the program. Additional courses/meetings appropriate to the trainee’s clinical and academic interests are considered.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1030
Board passage rate (3 years): 100%
Fellow salary:
PGY 6 $93 674 CAD, PGY 7 $100 722 CAD, additional call stipend (current as of July 1, 2024).
Ann & Robert H. Lurie Children’s Hospital of Chicago
Last updated: December 2023
Program website: https://www.surgery.northwestern.edu/divisions/pediatric/index.html
Institution Information
Ann & Robert H. Lurie Children’s Hospital of Chicago
Chicago, IL United States
Number of beds: 360
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
In the 2020-21 U.S. News & World Report rankings of the Best Children’s Hospitals, Lurie Children’s continues to be the top hospital in Illinois, ranking in all 10 specialties. Lurie Children’s was named a level 1 pediatric surgery center by the American College of Surgeons (ACS), becoming the first children’s hospital in Illinois to earn this status.
Research at Lurie Children’s is conducted through Stanley Manne Children’s Research Institute. We focus on improving child health, transforming pediatric medicine and ensuring healthier futures. In partnership with Northwestern University Feinberg School of Medicine, our scientists work in labs, in clinics, at the patient bedside and in the community to unravel the root causes of pediatric and adolescent disease, to understand childhood injury and to find factors that precipitate health problems in childhood and over a lifetime. Our researchers work every day to develop new therapies and prevention strategies.
More than 220,000 children receive the highest-quality medical care at Lurie Children’s each year.
Faculty Information
Program Director: Seth Goldstein, MD, MPhil
Program Coordinator: Chris Peltier
cpeltier@luriechildrens.org
312-227-4734
Faculty:
Amir Alhajjat, MD
Guillermo Ares, MD
Anthony C. Chin, MD
Alexander Dzakovic, MD
Julia Grabowski, MD
Seth Goldstein, MD
Yue-Yung Hu, MD
Rashmi Kabre, MD
Monica Langer, MD
Timothy Lautz, MD
Caroline Lemoine, MD
Mehul Raval, MD
Erin E. Rowell, MD
Aimen F. Shaaban, MD
Riccardo Superina, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Courtney Harris, MD
David Grabski, MD
Previous 5 fellows:
Guillermo Ares, MD
Samantha Ahle, MD
Nathaniel Koo, MD
Elliott Pennington, MD
Chethan Sathya, MD
Curriculum Information
Block Schedule:
Program Year 1: 1 month in NICU & 1 month in PICU, rest of time spent with Pediatric Surgery
Program Year 2: Solely spent with Pediatric Surgery
Call Schedule: Split home call
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Standard courses, with opportunity to individualize as needed
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1200
Board passage rate (3 years): N/A
Fellow salary: N/A
Arkansas Children's Hospital (University of Arkansas for Medical Sciences)
Last updated: December 2024
Program website: https://medicine.uams.edu/surgery/fellowships/pediatric-surgery/
As the only free-standing tertiary children’s hospital in the state, ACH provides fellows with the broad-based clinical experiences necessary to practice pediatric surgery independently in a variety of settings. These experiences occur in both the inpatient and outpatient settings exclusively on the ACH campus in Little Rock. Furthermore, trainees achieve this goal in an educational learning environment second to none. Our faculty are close-knit and share a common commitment to the fellows’ acquisition of medical knowledge and continual lifelong learning. ACH has also been verified as both a Level 1 Children’s Surgery center and a Level 1 Children’s Trauma center by the ACS. As such, fellows will develop and actively participate in quality initiatives in a setting emphasizing teamwork.
Institution Information
Arkansas Children’s Hospital
Little Rock, AR United States
Number of beds: 336
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
ACH is the only free-standing tertiary children’s hospital in Arkansas. The ACH campus spans 36 city blocks and is currently licensed for 336 beds. ACH has the only pediatric ICU in the state with 26 beds, cardiovascular ICU with 30 beds and the only Level IV NICU that is licensed for 104 beds. ACH offers outpatient, inpatient, perioperative, full diagnostic and therapeutic services for patients from micro-preemies to select adults with pediatric medical issues. Arkansas Children’s Hospital offers the only mobile ECMO and pediatric ECMO in the state of Arkansas. ACH has a staff of approximately 505 physicians, and over 200 residents in pediatrics and pediatric surgery. Additionally, the pediatric surgical service performs approximately 2,400 cases yearly.
Faculty Information
Program Director
Deidre Wyrick, MD
Assistant Program Director (if applicable)
Lindsey Wolf, MD
Program manager and email
Jill Hare 501.364.3962
Faculty:
Jeff Burford, MD
Sid Dassinger, MD
Richard Jackson, MD
Todd Maxson, MD
Deidre Wyrick, MD
Lindsey Wolf, MD
Robert Vandewalle, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Martha-Conley Ingram, MD
Greg Keefe, MD
Previous 5 fellows:
Elise McKenna, MD PhD
2023
Assistant Professor, New York University
New York, NY
Patrick Bonasso, MD
2022
Assistant Professor of Surgery, West Virginia University
Morgantown, WV
Lori Gurien, MD MPH
2021
Assistant Professor of Surgery, Nemours Children’s Health System
Jacksonville, FL
Mikki Kollisch-Singule MD
2020
Assistant Professor of Surgery, SUNY Upstate
Syracuse, NY
Deidre Wyrick, MD
2019
Assistant Professor of Surgery, UAMS
Little Rock, AR
Curriculum Information
Call Schedule
1st year: Q4
2nd year: Q4
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: We pay for Transition to Fellowship bootcamp, Pectus course, St. Jude course, MIS course, Colorectal course, APSA meeting, AAP meeting plus any additional meetings if fellow presenting own work.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): 100%
Fellow salary: $67,287
Baylor College of Medicine
Last updated: 09/14/2021
Program website: https://www.bcm.edu/departments/surgery/divisions/pediatric-surgery/education/pediatric-surgery-residency
The Pediatric Surgery Residency Program at Baylor College of Medicine and Texas Children’s Hospital is one of the top Pediatric Surgery Residency programs in the nation. The Pediatric Surgery Residency Program has continual full accreditation by the Accreditation Council for Graduate Medical Education. The program accepts one resident per year. Applicants must have completed a five-year Accreditation Council for Graduate Medical Education (ACGME) General Surgery Residency Program and be board-eligible in general surgery.
This two-year residency is primarily at Texas Children’s Hospital, the largest children’s hospital in the nation. Residents are exposed to a broad array of surgical cases and work closely with residents in pediatric medicine in the care of sick infants and children.
The first year includes up to two months of elective time, which may be tailored to the trainee’s special interests and career goals. In addition, the resident spends one month in the neonatal intensive care unit. During the remainder of the year, he or she has senior responsibilities at Texas Children’s Hospital. The second year is spent as chief resident of the program.
The program strives to graduate residents who excel as practitioners of pediatric surgery and become top leaders in the field, whether in academics or the private sector.
Strengths
- The large clinical volume of index cases allows the fellow to focus on those cases which interest them
- Diverse faculty with variety of experience and interests
- Yearly mock oral exam course provided for current fellows and graduated fellows;
- Dedicated programs in Colorectal, Thyroid, Fetal, Surgical Oncology, and Chest Wall Deformities – none of these programs have fellows of their own to limit experience of the pediatric surgery fellow.
Weaknesses
- Strong Pedi GYN and ENT divisions may limit exposure in these areas, although electives can be arranged
- Fellows not involved in transplant cases.
Institution Information
Texas Children’s Hospital
Houston, TX United States
Number of beds: 959
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Texas Children’s Hospital consists of a Main Campus, which includes the Pavilion for Women and Legacy Tower. The Pavilion for Women houses the Fetal Program, and the Legacy Tower consists of 25 floors devoted to ICU care and has a helipad for transporting patients to our hospital. Texas Children’s also consists of a West Campus (PICU, no NICU) and a Woodlands Campus (PICU and NICU). For fiscal year 2019, the Division of Pediatric General Surgery performed 6,632 cases, with 3,993 at the Main Campus. Pediatric surgery fellows have privileges and access to operative cases at all campuses.
Faculty Information
Program Director: Mark V. Mazziotti, MD, MEd
Associate Program Director: Jed G. Nuchtern, MD and Kristy Rialon, MD
Program manager: Maelene Phillips
(713) 798-6078
Fax: (713) 798-8941
pedisurgerytraining@bcm.edu
Faculty:
Sundeep Keswani, MD — Professor and Division Chief
Swathi Balaji, PhD — Assistant Professor
Lily Cheng, MD – Assistant Professor
Alice King, MD — Assistant Professor
Louis Le, MD — Assistant Professor
Timothy C. Lee, MD — Associate Professor
Mark V. Mazziotti, MD, MEd — Professor
Allen Milewicz, MD — Associate Professor
Paul K. Minifee, MD — Associate Professor
Jed G. Nuchtern, MD — Professor
Kristy L. Rialon, MD — Assistant Professor
Ruben Rodriguez, MD, MMSC — Assistant Professor
Sohail R. Shah, MD, MSHA — Associate Professor
Yan Shi, MD – Assistant Professor
Shawn Stafford, MD — Assistant Professor
Adam Vogel, MD — Associate Professor
David Wesson, MD — Professor, retired
Sanjeev A. Vasudevan, MD — Associate Professor
Fellow Information
Number of fellows: one per year
Current fellow(s):
Ross Beckman, MD (1st year fellow)
Ekene Onwuka, MD (2nd year fellow)
Previous 5 fellows:
Lily Cheng, MD
2019-2021
Assistant Professor of Surgery
Baylor College of Medicine
Raphael Sun, MD
2018-2020
Assistant Professor of Surgery
Co-Director of Fetal Surgery
Oregon Health & Science University
Ihab Halaweish, MD
2017-2019
Assistant Professor of Surgery
Nationwide Children’s Hospital
Sara C. Fallon, MD
2016-2018
HCA Healthcare
Houston, TX
Danielle M. Hsu, MD
2015-2017
Assistant Professor of Surgery and Pediatrics
University of Texas
Curriculum Information
1st Year home and 1-2 nights in house per month
2nd Year home and 1-2 nights in house per month
Each conference is one hour per week:Fellows Conference combined with University of Texas faculty
Pathology/Radiology Conference
Mobidity/Mortality Conference
Indications Conference
Surgery Quality Improvement Conference alternating with Surgery Grand Rounds
Trauma M&M (monthly)Optional Conferences: Fetal, GI, Tumor Board
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Pays for Colorectal Course, Oncology course (St. Jude’s), APSA (first year fellow), AAP Section on Surgery (second year fellow); ECMO Course at UT; Pediatric Surgery Boot Camp (prior to fellowship).
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: 1,228
Board passage rate (3 years): 100%
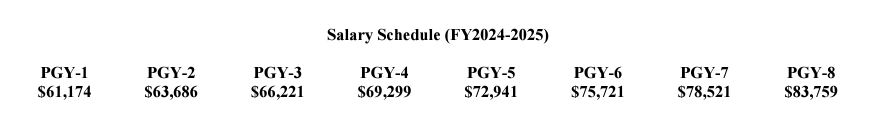
Fellow salary: (2019-2020) PGY6: $69,947; PGY7: $72,306; PGY8: $74,114
BC Children’s Hospital Pediatric Surgery, University of British Columbia, Vancouver, Canada
Last updated: January 2024
Program website: https://surgery.med.ubc.ca/divisions/pediatric-surgery/
Pediatric surgery fellows are ultimately responsible for the supervision of the pediatric surgical service, including inpatient and outpatient consultations, pre- and post-operative care, as well as operative procedures. They will learn the full breadth of pediatric surgery, and are expected to be ambassadors for our division throughout the hospital and wider community. As such, successful candidates for pediatric surgery fellowship must have a demonstrable track record of interest in the field of pediatric surgery, exemplary communication and leadership skills and a commitment to patient/family-centered care.
The pediatric surgery program at the BC Children’s Hospital is responsible for all tertiary/quaternary level surgical care for children in the province of British Columbia, with an enormous geographical catchment area and a population served approaching 5 million people. As such, we see the full spectrum of congenital, oncologic and pediatric trauma populations, with many routine pediatric procedures (onychectomy, appendectomy, etc…) performed at outside facilities. We take particular pride in servicing our northern, remote and Indigenous communities in a culturally contextualized manner. We also dedicate considerable energy and resources to ensuring a rigorous academic curriculum nested within the educational framework of both the Royal College of Canada as well as the American College of Surgeons (ACS). Our median case volumes remain well within the standards of the ACS, and electives in other surgical subspecialties as well as an international experience are available depending on individual trainee interests and career aspirations.
Institution Information
Training Site #1
BC Children’s Hospital, free-standing children’s hospital, with attached obstetrical center (BC Women’s)
4500 Oak St, Vancouver, BC V6H 3N1
Faculty Information
Program Director: Robert Baird, MD
robert.baird@cw.bc.ca
Associate Program Director:
Program manager: Shania Linggon
Shania.linggon@cw.bc.ca
Faculty:
Eric Webber MD
Erik Skarsgard MD
Sonia Butterworth MD
Hannah Piper MD (Division Head)
Shahrzad Joharifard MD
Fellow Information
Number of fellows:
One fellow per year (Matched fellows every other year)
Current fellow(s):
Moses Kasumba
Amanda Phares (Chief)
Previous 5 fellows:
AlReem Al-Hinai
2023
RBC Rainbow Babies & Childrens
Martina Mudri
2022
Victoria General Hospital, VIHA
AlGhalya AlMaawali
2021
Sultan Qaboos University
Arash Safavi
2020
Children's Hospital of Los Angeles
Anne Shikanda
2019
Norvik Hospital, Uganda
Curriculum Information
Mandatory NICU/PICU rotation in y1; electives available
12 months consecutive PSx in y2
Program Information
RRC accreditation status: Fully Accredited by the Royal College of Physicians and Surgeons of Canada in 2020 (next accreditation in 2026)
Meeting/Training Course policy:
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1000
Board passage rate (3 years): 100%
Fellow salary: https://www.carms.ca/match/r-1-main-residency-match/salary/#1511459599452-6c7d2a84-0f83
Boston Children’s Hospital Pediatric Surgery Fellowship
Last updated: January 2025
Program website: https://dme.childrenshospital.org/graduate-medical-education/trainings-programs/surgery/pediatric-surgery-fellowship/
Boston Children’s Hospital has a long and rich tradition of training the leaders in pediatric surgery. Our fellowship is the crown jewel of a Department steeped in history as the birthplace of pediatric surgery and yet dedicated to pushing our field forward as a leader in education, innovation, research and clinical care. The fellowship is a two-year clinical training program for which we have three ACGME approved positions. One resident is selected to begin training on odd years and two residents to begin training on even years through the National Resident Matching Program administered by the Electronic Residency Application Service (ERAS). The applicant must have completed a general surgical training program by the time of program matriculation and be eligible to take the qualifying examination in general surgery given by the American Board of Surgery or the Royal College of Surgeons of Canada.
Our fellowship offers exposure to a large volume of ‘bread and butter’ as well as complex cases with liberal use of minimally invasive techniques. Operative experience includes thoracic, abdominal, head and neck, urologic, oncologic, vascular, endoscopic and transplant surgery.
The program is structured to offer residents a total of 16 months of their 24 month tenure as the chief on one of our two services, working closely with our surgical faculty and their co-fellows in all aspects of patient management on the surgical floors, ICU and NICU. A staff of over 18 pediatric nurse practitioners provide the chief residents with experienced and reliable care of all surgical inpatients 24 hours per day and 7 nights per week. In addition, the residents rotate in functioning as the administrative chief resident, helping to organize the operating room schedule, large surgical resident and medical student contingent and a robust educational conference schedule. Administrative staff within the Department help the chief residents with these tasks.
A very close working relationship exists between the surgical faculty and the pediatric surgery residents. In addition to primary surgeons coordinating care of patients with the fellows, a staff surgeon is assigned as the “Surgeon of the Day” for acute consults and another staff surgeon as “Surgeon of the Week” to help care for the inpatient services and serve as sounding boards for the fellows as they make patient care decisions.
In the ICU and NICU, the chief residents collaborate with critical care and neonatology staff in their responsibility to direct the multidisciplinary care of these patients. The general surgery census averages 40-70 inpatients per day.
Institution Information
Boston Children’s Hospital
Boston, MA United States
Number of beds: 477
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Boston Children’s Hospital is ranked the number one pediatric hospital in the world by Newsweek and for over a decade has remained in the Honor Roll of Pediatric Hospitals by U.S. News and World Reports. It is home to the world’s largest pediatric research enterprise, and it is the leading recipient of pediatric research funding from the National Institutes of Health. It is the primary pediatric teaching hospital for Harvard Medical School. Boston Children’s Hospital has more than 40 clinical departments and 258 specialized clinical programs. https://www.childrenshospital.org/
Faculty Information
Program Director: Biren P Modi, MD, MPH
Associate Program Director: Brent Weil, MD, MPH; Prathima Nandivada, MD
Program manager:
Katherine Mooney, MHA
Katherine.mooney@childrens.harvard.edu
617-919-2469
Faculty:
Terry Buchmiller, MD
Catherine Chen, MD, MPH
Alex Cuenca, MD, PhD
Belinda Dickie, MD, PhD
Farokh Demehri, MD
Steven Fishman, MD
Tom Jaksic, MD, PhD
Heung Bae Kim, MD
Monica Langer, MD, MS
Craig Lillehei, MD
Arin Madenci, MD, MPH, SM, PhD
Biren Modi, MD, MPH
Somala Mohammed, MD, MPH
David Mooney, MD, MPH
Prathima Nandivada, MD
Konstantinos Papadakis, MD
Mark Puder, MD, PhD
Shawn Rangel, MD
Robert Shamberger, MD
Brent Weil, MD, MPH
Christopher Weldon, MD, PhD
Jill Zalieckas, MD, MPH
Ben Zendejas-Mummert, MD
Fellow Information
Number of fellows: 3
Current fellow(s):
Brian Fallon, MD
Mark Fleming II, MD
Eliza Lee, MD
Previous 5 fellows:
Arin Madenci, MD, MPH, SM, PhD
2024
Pediatric Surgeon, Boston Children’s Hospital; Assistant Professor of Surgery, Harvard Medical School
Boston, MA
Patrick Delaplain, MD
2024
Pediatric Surgeon, Texas Children’s Hospital; Assistant Professor, Baylor College of Medicine
Houston, TX
Woo Do, MD
2023
Pediatric Surgeon, Walter Reed National Military Medical Center
Bethesda, MD
Danielle Cameron, MD, MPH
2022
Pediatric Surgeon, Massachusetts General Hospital; Director of Pediatric Surgical Oncology, Mass General Hospital for Children; Assistant Professor of Surgery, Harvard Medical School
Boston, MA
Jamie Robinson, MD, PhD
2022
Pediatric Surgeon, Monroe Carell Jr. Children’s Hospital at Vanderbilt; Assistant Professor of Pediatric Surgery, Vanderbilt University
Nashville, TN
Hester Shieh, MD
2021
Pediatric Surgeon, John Hopkins All Children’s Hospital
St Petersburg, FL
Somala Mohammed, MD, MPH
2020
Pediatric Surgeon, Boston Children’s Hospital; Assistant Professor of Surgery, Harvard Medical School
Boston, MA
Prathima Nandivada, MD
2020,
Pediatric Surgeon, Boston Children’s Hospital; Assistant Professor of Surgery, Harvard Medical School
Boston, MA
Curriculum Information
Call Schedule
The pediatric surgery fellows take in-house call only on Fridays, as a “pre-attending” with a faculty backup. Otherwise, they take only home call, which does count toward the 80 hour work week limit. In general, the fellows take home call Q3 and work every third weekend. The pediatric surgery fellows have two weeks of vacation each year per ACGME guidelines.
Conference Schedule
The Department provides a number of didactic teaching programs: Advanced Fetal Care Conference, Didactic Lecture Series, Combined Gastroenterology/Surgery Conference, Morbidity and Mortality Conference, Oncology Radiology Conference, Professor Rounds, Combined Radiology/Surgery Conference, Surgical Grand Rounds, Trauma Conference, Vascular Anomalies Conference, and Indications Case Conference.
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Full financial support for attendance at APSA, AAP, as well as specialty courses such as MIS, Oncology and Colorectal. Other support is also available on a case by case basis based on fellow interests.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: 1,189
Board passage rate (3 years): 93.33%
Fellow salary: $140,000 per year
Brown University
Last updated: December 2024
Program Website - https://med.brown.edu/pedisurg/index.html
Overview of Fellowship
The fellowship program at Brown University was first accredited in 1995 shortly after the opening of the new Hasbro Children’s. Its previous fellows have had a growing impact on the field of pediatric surgery through their roles as Division Directors, NIH (KO8 and R01)-funded clinician scientists, fetal surgery program directors, trauma program directors and missionary pediatric surgeons. The Fellowship Program aims to train excellent clinicians who are future leaders of their field. Hasbro Children’s Hospital, in conjunction with the neighboring 75 bed NICU at Women and Infant’s Hospital, serves a diverse patient population. The setting of Providence, RI provides an energetic and culturally rich background for fellows as they complete their two years of training.
Institution Information
Training site #1:
Name: Hasbro Children’s Hospital
#beds: 85
Percentage of time at this location: 90%
Children’s hospital within an Adult hospital
Brief description of other hospital information
5000 operations/year
50,000 ER visits/year
Programs:
Fetal Surgery Program
Adolescent Bariatric Surgery Program
Vascular Anomalies Program
Multidisciplinary Bowel Rehabilitation Program
Level 1 Pediatric Trauma Center
Level 1 Burn Center
Pediatric ECMO Program
Pediatric Renal Transplant Program
Founding member of NAFNet
Training Site #2:
Name: Women and Infants Hospital
#beds: 75
Percentage of time at this location: 10%
Brief description of other hospital information
Member of NICHD, MFMU, and Neonatal Research Network
Faculty Information
Program Director:
Elizabeth Renaud, MD
Assistant Program Director (if applicable):
Julie Monteagudo, MD
Program manager and email:
Bridget Glazier
bglazier@brownhealth.org
phone 401-444-3717
fax 401-444-6681
List of Faculty and titles
Francois Luks, MD, PhD
Professor of Surgery, Pediatrics, Obstetrics & Gynecology
Division Chief, Surgeon in Chief, Hasbro Children’s Hospital
Elizabeth J. Renaud, MD
Associate Professor of Surgery and Pediatrics
Pediatric Trauma Medical Director
Julie Monteagudo, MD
Assistant Professor of Surgery and Pediatrics
Director of Pediatric ECMO
Samantha Ahle, MD, MHS
Assistant Professor of Surgery and Pediatrics
Surgical Residency Program Associate Program Director
Artur Chernoguz, MD, FACS
Assistant Professor of Surgery and Pediatrics
Carl-Christian Jackson, MD, FACS, FAAP
Associates Professor of Surgery and Pediatrics
Fellow Information
Number of fellows:
One every other year
Current fellow(s) names:
Alejandra Casar-Berazaluce, MD
List of previous 5 fellows: name, grad year, current position
Melissa Vanover, MD, 2023. Sutter Medical Foundation- Sutter Medical Group, Sacramento, CA
Inna Lobeck, MD, 2021. American Family Children’s Hospital/University of Wisconsin School of Medicine and Public Health
Julie Monteagudo, MD, 2019. Hasbro Children’s Hospital/Brown University, Providence, RI
Alexis Smith, MD, 2017. Children’s Healthcare of Atlanta at Scottish Rite Hospital, Atlanta, GA
Joseph Hartwich, MD, 2015. Inova Children’s Hospital, Fairfax, VA.
Call schedule
1st Year – Home call, Q2 with APP coverage
2nd Year – Home Call, Q2 with APP coverage
Conference Schedule
Tuesday 7 am Surgery Grand Rounds
Wednesday
7 am alternating weeks: Department of Surgery Morbidity and Mortality Conference, Pediatric Surgery M&M
7:45 am Perinatal Management Conference
8 am alternating weeks: Pediatric Surgery Conferences, Tumor Board
Friday 12 PM M.A.D.A.M Conference
Program Information
RRC accreditation status: Continued Accreditation
Initial Accreditation: June 29, 1995
Continued Accreditation: January 7, 2021
Meeting/Training Course policy
Pays for APSA meeting first year, APP meeting second year, St. Jude Course, and Fellowship Bootcamp. Will also cover any additional meeting if fellow is presenting his/her own work.
Does the program provide financial support for candidate interviews?
No
Optional information
What is the average total number of cases performed by your graduating fellows over the past five years?
Board Passage rate (last ten years)
100%
Fellow Salary
First Year: $85,473.15
Second Year: $ 93,026.85
Children’s Hospital Colorado/University of Colorado Pediatric Surgery Fellowship
Last updated: December 2024
Program website: https://medschool.cuanschutz.edu/surgery/divisions-centers-affiliates/pediatric/education/pediatric-surgery-fellowship-program
Our two-year fellowship was established in 1993. Our mission is to provide a well-rounded pediatric surgical education in all facets of our specialty. Our global objective is to prepare the graduates of our program to step into their careers prepared to meet the challenges of the profession, regardless of their ultimate career goals.
During the two-year curriculum, fellows work exclusively at the Children’s Hospital Colorado in Aurora. During the first year, the fellow rotates a month each on Neonatology, Critical Care, and Urology. The rotations provide a focused, in-depth experience in each of these subspecialty areas, which are important aspects of pediatric surgical practice. The other nine months are spent on Pediatric Surgery where the trainee will develop expertise in the diagnostic, operative, and perioperative surgical care of patients, from prenatal diagnosis through adolescence, with congenital and acquired anomalies and diseases. As Chief, the second year is designed to prepare the fellow for independent practice, to broaden his/her experience in all areas of pediatric surgery, and to provide greater depth of knowledge in neonatal surgical problems, oncology, trauma management, and surgical disorders of the chest and abdomen. The fellowship is organized to ensure that the trainee is prepared for the American Board of Surgery – Pediatric Surgery Qualifying and Certifying Examinations. Regardless of a fellow’s ultimate career goal, the faculty is absolutely committed to helping all fellows achieve their goals.
The graduates of our program have established very successful careers across the country. Our fellows are in both academic medical centers and private practice. Regardless of the area of clinical focus, the graduates of our programs have consistently provided feedback that they were more than ready to function independently upon completion of the fellowship program.
Strengths
- Large scope of Pediatric Surgery defined cases
- Large volume of colorectal cases
- Financial support for 6+ national conferences and educational courses
- Strong program support for career development
- Strong service support minimalizing the trainee’s service obligations
- Large APP support for both services
Weakness
- Fellows not involved with transplant cases
Institution Information
Children’s Hospital Colorado
Aurora, CO United States
Number of beds: 444
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Faculty Information
Program Director: David Partrick, MD
david.partrick@childrenscolorado.org
Associate Program Director: Jose Diaz-Miron, MD
Jose.diaz-miron@childrenscolorado.org
Program manager: Jaymie Donner
Jaymie.donner@childrenscolorado.org
Faculty:
Shannon Acker, MD
Andrea Bischoff, MD
Luis De la Torres, MD
S. Christopher Derderian, MD
Kristine Corkum, MD
Jose (Pepe) Diaz-Miron, MD
Ann Kulungowski, MD
Steve Moulton, MD
David Partrick, MD
Jonathan Roach, MD
Stig Somme, MD
John Wiersch, MD
Jonathan Hills-Dunlap, MD
Guy Jensen, MD
Thomas Rauth, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Alexandria Robbins, MD
Jenny Stevens, MD
Previous 5 fellows:
Andrew Trecartin
August 2023 – July 2024
Associate Professor of Surgery and Pediatrics
East Tennessee State University
Johnson City, TN 37604
Jonathan Hills-Dunlap, MD
August 2021 – July 2023
Assistant Professor of Surgery and Pediatrics
University of Colorado/Children’s Hospital
Colorado Aurora, CO
Kristine Corkum, MD
August 2020 – July 2022
Assistant Professor of Surgery and Pediatrics
University of Colorado/Children’s Hospital
Colorado Aurora, CO
Christopher Derderian, MD
August 2019-July 2021
Assistant Professor of Surgery and Pediatrics
University of Colorado/Children’s Hospital Colorado
Aurora, CO
Shannon Acker, MD
August 2017 – July 2019
Assistant Professor of Surgery and Pediatrics
University of Colorado/Children’s Hospital Colorado
Aurora, CO
Curriculum Information
Call Schedule
1st Year – In-house call, 15 calls over 13 weeks
2nd Year – In-house call, 15 calls over 13 weeks
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Pays for Transition to Fellowship bootcamp, St. Jude course, MIS course, Peña Colorectal course, PECTUS course, APSA meeting, AAP meeting plus any additional meetings if fellow presenting. Time away subject to RRC regulations governing time in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1155
Board passage rate (3 years): 100%
Fellow salary: Salary information updated annually to reflect cost of living in the Denver, Colorado at https://medschool.cuanschutz.edu/graduate-medical-education/CUGME-benefits/stipends
PGY-7: $100,483.00 PGY-6: $95,438.00
Children’s Hospital Los Angeles
Last updated: April 2025
Program website: https://www.chla.org/fellowship/pediatric-surgery-fellowship
Children's Hospital Los Angeles offers a comprehensive two-year residency (fellowship) training program in pediatric surgery. This fellowship program, designed for residents who have completed their training and are Board-eligible in general surgery, is accredited by the Residency Review Committee (RRC) of the Accreditation Council for Graduate Medical Education.
The Division of Pediatric Surgery participates in the National Intern and Resident Matching Plan and chooses one fellow each year for the program.
Our fellowship offers a great breadth of cases. Operative cases include extensive experience with neonatal surgery, anorectal malformations, pediatric surgical oncology, hepatobiliary and thoracic surgery. In the first year, junior fellows gain experience in general pediatric surgery, trauma, neonatology and intensive care of older children, pediatric otolaryngology, and urology. They gradually assume a greater role in patient management and administrative duties in the final two months of the year. In the second year, senior fellows participate in virtually all newborn surgery, tumor surgery and non-cardiothoracic surgery while on service and have administrative responsibilities for weekly conferences.
There are weekly lectures led by Pediatric Surgery faculty as well as other faculty members from other specialties such as pediatric oncology, neonatology and pediatric anesthesiology. Each weekly lecture is followed by rounds in the Newborn and Infant Critical Care Unit (NICCU), where fellows, residents and medical students review complex neonatal surgical patients and discuss challenging scenarios to simulate the pediatric surgery boards. Pediatric Surgery and NICCU faculty members lead the rounds. Attendance at outpatient clinics one half-day a week is required, and a monthly clinic devoted to long-term patient-care follow-up is mandatory throughout the two-year fellowship. Residents can attend specialty clinics such as Vascular Anomalies Clinic, Colorectal Clinic, Trauma Clinic and Aerodigestive Clinic.
At our facility, fellows will have access to the knowledge and expertise of 7 (subject to change) pediatric surgeons who have different backgrounds, teaching methods and interests. Fellows will also be mentored on becoming a successful surgeon in academic medicine.
During the fellowship, the senior fellow is expected to complete the American Board of Surgery qualifying and certification exams in general surgery. Upon completion of the fellowship program, the graduating fellow will be eligible to take the Board exam in pediatric surgery.
Institution Information
Children’s Hospital Los Angeles
Los Angeles, CA United States
Number of beds: 413
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
>17K Discharges/year
>17K surgeries/year
Children’s Hospital Los Angeles is one of the nation’s leading pediatric hospitals. True to our mission, we have been creating hope and building healthier futures since 1901. Our medical experts offer more than 350 pediatric specialty programs and services to meet the needs of our patients. Our comprehensive approach ensures that each child is cared for, regardless of circumstances, and makes care as accessible and convenient as possible. We believe every child deserves a healthier future and access to the best care possible is central to this belief. That is why we make our expertise available to children across the globe and why we train the next generation of pediatric specialists.
Our hospital has been ranked as a top health care facility for children by U.S. News & World Report magazine every year since the magazine began ranking pediatric hospitals in 1990. In U.S. News & World Report's most recent rankings, we were ranked the No. 1 hospital in California for caring for children.
The Department of Surgery brings together specialized pediatric knowledge, dedication to excellence and family-centered care in one of the country’s finest, most comprehensive pediatric surgical programs, comprising a full spectrum of surgical specialties. We perform over 15,400 surgical procedures annually for children ranging in age from newborns to adolescents, unlike practices where practice are routinely performed for adults and these approaches are simply adjusted to fit a child. Patients ranging in age from newborns to adolescents are treated in the hospital’s spacious, state-of-the-art Burtie Green Bettingen Surgery Center, which opened in 2001. Our surgeons conduct research and maintain academic affiliations with the Keck School of Medicine of the University of Southern California.
Faculty Information
Program Director: Donald J. Lucas, Jr., MD, MPH, FACS
Associate Program Director: N/A
Program manager:
Monica Del Rio
mdelrio@chla.usc.edu
(323) 361-7097
Faculty:
Dean Anselmo, MD, FACS, FAAP
Christopher Gayer, MD, PhD, FACS, FAAP
Lorraine Kelley-Quon, MD, MSHS, FACS, FAAP
Aimee Kim, MD
Donald Lucas, Jr., MD, MPH, FACS
Nam Nguyen, MD, FACS, FAAP
Arash Safavi, MD, MHSC, FRCSC, FACS, FAAP
Cathy Shin, MD, FACS< FAAP
Ryan Spurrier, MD, FACS
James Stein, MD, MSc, FACS, FAAP
Michael Zobel, MD
Fellow Information
Number of fellows: two, one per year
Current fellow(s):
Kasiemobi (Kasi) Pulliam, MD
Celia Short, MD
Previous 5 fellows:
Michael Zobel, MD
2024
Children’s Hospital Los Angeles
Los Angeles, CA
Lauren Baumann, MD, MHS
2023
Intermountain Health Primary Children’s Hospital
Salt Lake City, UT
Gillian Fell, MD, PhD
2022
Stanford Children’s Health, Lucile Packard Children’s Hospital Stanford
Palo Alto, CA
David Darcy, MD
2021
Golisano Children’s Hospital
Rochester, NY
Willieford Moses, MD
2020
UCSF Benioff Children’s Hospital
Oakland, CA
Curriculum Information
Call Schedule
1st Year – home
Q2 weekdays
Other – every other weekend
2nd Year – home
Q2 weekdays
Other – every other weekend
Conference Schedule
Weekly: Joint Service M&M Conferences, Thursday Lecture Core Series, NICU Teaching rounds
Monthly: Trauma M&M Conference, Surgical Simulation Workshops
Biannually: Surgical Grand Rounds at USC Keck School of Medicine
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Junior fellow attends the transition to the Fellowship Bootcamp, APSA conference and MIS course. Second year fellow attends the following conference/courses: AAP, Colorectal, Oncology.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: 1222
Board passage rate (3 years): 100%
Fellow salary: According to Post Graduate Year
Children’s Hospital of Michigan
Last updated: 1/11/2023
Program website: https://www.childrensdmc.org/our-services/surgery/meet-the-surgeons
We are interested in candidates who wish to a have a broad scope of experiences in the care or surgical diseases of infants and children with faculty who are committed to their education. Our strengths are in the surgical management of the patients at all levels including having the NICU and PICU surgical patients on our surgical service with our service managing all these patients. We have a robust trauma and burn program. We have an ECMO service which we run. We have a Intestinal Rehabilitation Program. Although we do some clinical research our strength is the clinical experience from the common to the rare diseases of children. https://www.childrensdmc.org/our-services/surgery/meet-the-surgeons.
Institution Information
Children’s Hospital of Michigan
Detroit, MI United States
Number of beds: 250
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
10,000 OR cases per year. Over 100,000 ER visits per year.
Faculty Information
Program Director: Scott Langenburg, MD, FACS, FAAP
Associate Program Director: Justin Klein, MD, FACS, FAAP
Program manager: Christine Klimek
Cklimek@dmc.org
313-831-3220
Faculty:
Joseph Lelli, MD — Surgeon-In-Chief
Christina Shanti, MD — Chief of General Surgery
Lydia Donoghue, MD — Trauma Medical Director
Justin Klein, MD — Burn Medical Director
Michelle Veenstra, MD — ECMO Director
Fellow Information
Number of fellows: one per year
Current fellow(s):
Andrew Nordin, MD
Christopher Marenco, MD
Previous 5 fellows:
John Wiersch, MD
Colorado Children’s Hospital
Brenna Fullerton, MD
Orlando Children’s Hospital
Paulette Abbas, MD
Texas Children’s Hospital Dallas
Iljana Gaffar, MD
Northwell Health and King’s County, New York
Curriculum Information
1st year: home call
2nd year: home call
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Yes
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): 100%
Fellow salary: $60,000/year
Children’s Hospital of Philadelphia’s Pediatric General Surgery Fellowship
Last updated: November 2024
Program website: https://www.chop.edu/pediatric-fellowships/pediatric-general-surgery-fellowship
The training program for the Louise Schnaufer Endowed Fellowship in Pediatric Surgery is two years in duration beginning August 1 of each year. All training occurs at a single site, the Main Campus of The Children’s Hospital of Philadelphia. The fellow’s primary training will take place within the Division of Pediatric General, Thoracic and Fetal Surgery. This is a “fellow-centered” clinical service that demands efficiency, ownership, and constant reflection-in-action to build proficiency. The educational program in pediatric surgery includes operating room experience, bedside clinical teaching, and an active conference routine.
Institution Information
The Children’s Hospital of Philadelphia
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Faculty Information
Program Director: Joy Collins, MD
Associate Program Director: Myron Allukian, MD
Program manager: Kelsey Murray
bockk@chop.edu
215-590-5294
Faculty:
Scott Adzick, MD – Surgeon-in-Chief
Joy Collins, MD –Program Director
Myron Allukian, MD – Associate Program Director
Michael Nance, MD – Division Chief
Gary Nace, MD – Attending Surgeon
Alan Flake, MD – Attending Surgeon
Holly Hedrick, MD – Attending Surgeon
Pablo Laje, MD – Attending Surgeon
Peter Mattei, MD – Attending Surgeon
William Peranteau, MD – Attending Surgeon
Emily Partridge, MD – Attending Surgeon
Duy Dao, MD – Attending Surgeon
Fellow Information
Number of fellows: other
Current fellow(s):
Matthew Goldshore, MD
Emily Onufer, MD
Clara Nicolás Martínez, MD
Previous 5 fellows:
Duy Dao, MD
2024
Patrick McGovern, MD
2023
John Stratigis, MD
2023
Avery Rossidis, MD
2022
Dana Schwartz, MD
2021
Program Information
RRC accreditation status: Initial accreditation
Meeting/Training Course policy: yes
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): N/A
Fellow salary: N/A
Children’s National Hospital
Last updated: September 2023
Program website: https://childrensnational.org/research-and-education/healthcare-education/residencies-and-fellowships/fellowship-programs/surgery
Our program seeks highly skilled, dedicated and motivated individuals who are committed to providing the best possible care to patients and their families. The fellows in our program will receive extensive experience and training in the surgery of congenital malformations, oncology, minimally invasive procedures, colorectal and pelvic reconstruction and complex pediatric cases. They manage patients on the pediatric surgery service along with an attending physician.
Institution Information
Children’s National Hospital
Washington, DC United States
Number of beds: 323
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Faculty Information
Program Director: Mikael Petrosyan, MD, MBA
Associate Program Director:
Program manager: Yvette Dill
ydill@childrensnational.org
202-476-2151
Faculty:
Anthony D. Sandler, MD – Surgeon-In-Chief and Senior Vice President, Division of General and Thoracic Surgery, Director, Sheikh Zayed Institute for Pediatric Surgery Innovation
Timothy D. Kane, MD – Chief, Division of General and Thoracic Surgery
Mikael Petrosyan, MD – Associate Chief, Division of General and Thoracic Surgery, Director, Surgical Residency Training Program
Marc A. Levitt, MD – Chief, Colorectal and Pelvic Reconstructive Surgery
Andrea Badillo, MD – Surgical Director, Fetal Medicine Institute
Randall S. Burd, MD – Chief, Division of Trauma and Burn Services
Arunachalam Thenappan, MD – Director, Surgical Critical Care Fellowship
Christina Feng, MD
Jeffrey R. Lukish, MD
Manuel B. Torres, MD
Kibileri Wiliams, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Mark Kovler, MD
Carolyn Gosztyla, MD
Previous 5 fellows:
Adil Shah, MD
2023
Attending Surgeon
Omaha, Nebraska
Kibileri Williams, MD
2022
Attending Surgeon
Children’s National Hospital
Rodrigo Mon, MD
2021
Attending Surgeon
Children’s Healthcare of Atlanta, Georgia
Jun Tashiro, MD
2020
Attending Surgeon
NYU Langone
Jason Sulkowski
2019
Attending Surgeon
Children’s Hospital of Richmond VCU
Curriculum Information
Call Schedule
1st year: Every other Wed and every other Saturday
2nd year: Every other Tuesday and Every other Saturday
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy:
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1500
Board passage rate (3 years): 100%
Fellow salary: N/A
Children's Hospital, University of Oklahoma
Last updated: December 2024
Program web page URL https://medicine.ouhsc.edu/academic-departments/surgery/education-programs/residency-fellowship-programs/pediatric-surgery-residency-fellowship-program
Overview of Fellowship
The University of Oklahoma offers a two-year ACGME-accredited clinical training program, accepting one fellow each year. Fellows in our pediatric surgery program can expect a challenging yet rewarding educational experience. Our graduates complete training with an average of 1,500 cases during fellowship. Board passage rates for our graduating fellows is 100 percent.
Our facility is a regional center for comprehensive, specialized pediatric services and the only fully dedicated, free-standing pediatric hospital in the state, including the only Level Four NICU in the state. More than 2,500 pediatric surgical operations are performed each year by our five full-time pediatric surgeons, and hospital admissions average more than 14,000 per year.
The teaching program emphasizes responsibility, self-directed learning and exposure to a broad spectrum of clinical material. The fellows round twice daily and supervise three general surgery residents, two nurse practitioners, and two medical students assigned to pediatric surgery. Faculty members are available for constant interaction and feedback.
Year one: Pediatric surgery training involves a closely supervised two-year period of education, gradually giving trainees more responsibility and independence. The initial six months of training will expose the resident to clinical care of all common and tertiary pediatric surgery problems. The second six months is focused on directing the trainee to become more independent in his/her patient care management; building a broad base of knowledge in both pediatric physiology and pathobiology and incorporating a collaborative clinical research project with the faculty. Constant communication between the first-year trainee, the attendings and the senior fellow is expected.
Year two: During the second year of training, the trainee is expected to perform in a more independent fashion, making important decisions regarding preoperative, intraoperative and postoperative patient management. The fellow is given additional teaching and administrative responsibilities, as well as additional independent operating room experience as his/her technical skills are developed through one-on-one teaching. Progression of responsibility toward independent performance, especially during the last six months of clinical training, is strongly promoted by faculty. Pediatric surgery attendings continually monitor and provide appropriate feedback to the pediatric surgery fellow throughout his/her clinical training both in and out of the operating room.
Institution Information
Training site #1:
Name: Oklahoma Children's Hospital at OU Medical Center
#beds: 350
Percentage of time at this location: 100%
Brief description of other hospital information: Oklahoma Children’s Hospital is the only freestanding children’s hospital in the state and the only level 1 trauma facility for children. The pediatric surgical fellowship is well-established and has been in place since 1979.
Faculty Information
Program Director: Dr. Catherine Hunter, M.D.
Assistant Program Director (if applicable): Dr. Alessandra Landmann, M.D. and Dr. Jeremy Johnson, M.D.
Program manager and email: Raven Nelson, raven-nelson@ouhsc.edu
List of Faculty and titles
- Catherine Hunter, MD- Division Chief/Fellowship Program Director
- Alex Ruiz-Elizalde, MD- Associate Professor of Surgery/Vice Clinical Surgical Service Chief
- Jeremy Johnson, MD- Associate Professor of Surgery/Trauma Medical Director, Children's Hospital/Co-Director, Third Year Surgical Clerkship
- Alessandra Landmann, MD- Assistant Professor of Surgery/Fourth Year Surgery Clerkship Director/Surgical Critical Care Fellowship Program Director
- Paul McGaha, MD- Assistant Professor of Surgery/ ECMO Pediatric Surgery Medical Director
Fellow Information
Number of fellows: 2
Current fellow(s) names:
- Robert Crum, M.D.
- Kathryn Maselli, M.D.
List of previous 5 fellows: name, grad year, current position
- Ryan Phillips, M.D. (2024) Private Practice, Savannah, GA
- Christie Buonpane, M.D. (2023) Academic Practice, Louisville, KY
- Jonathan Green, M.D. (2022) Academic Practice, U Mass, MA
- Alessandra Landmann, M.D. (2021) Academic Practice, Oklahoma City, OK
- Rodrigo Interiano, M.D. (2020) Private Practice Dallas, TX
Call schedule
Home call shared between fellows.
Conference Schedule
- Clinical Sciences/SCORE Conference (Weekly on Monday mornings)
- Morbidity & Mortality (M&M) Conference (Bi-Weekly on Friday mornings)
- Journal Club (Monthly)
- Radiology Conference (Monthly)
- Multidisciplinary Tumor Conference (Weekly)
- GI/Surgery Conference (Monthly)
Program Information
RRC accreditation status: Fully acredited
Initial Accreditation: February 01, 1978
Continued Accreditation: January 04, 2024
Meeting/Training Course policy
Fellows are supported to travel to one national meeting per year (APSA 1st year, AAP 2nd year). Fellows are also supported to attend the St. Jude’s oncology course and one complex colorectal course of their choice.
Does the program provide financial support for candidate interviews? No
Optional information
What is the average total number of cases performed by your graduating fellows over the past five years?
1500
Board Passage rate (last ten years): 100%
Fellow Salary:
CHU Sainte-Justine Pediatric Surgery Fellowship (Université de Montréal)
Last updated: 10/27/2021
Program website: https://enseignement.chusj.org/fr/Etudiants-en-stage/Fellowships/Fellowship-en-chirurgie-pediatrique https://medpostdoc.umontreal.ca/programmes/chirurgie-pediatrique/
The Pediatric Surgery Training Program at CHU Sainte-Justine is a two-year residency program accredited by the Royal College of Physicians and Surgeons of Canada. The reciprocity agreement between the Royal College and ACGME in the United States permits the trainee who successfully completed the program to be qualified for examinations in Pediatric Surgery given by the Royal College and the American Board of Surgery. The program was founded more than 60 years ago and has trained about a hundred of pediatric surgeons who are now practicing all over the world.
Since August 2020, the program has transitioned to Competency by Design, the Royal College’s model of competency-based medical education. As part of this model, the curriculum is designed to permit the progressive acquisition of the competencies of a pediatric surgeon. The fellows have frequent assessment and meaningful feedback from faculty. The first year include 2 mandatory 1- month rotations (Neonatal Intensive Care Unit (NICU), Pediatric Intensive Care Unit (PICU). During the second year, the fellow works at the level of chief resident in Pediatric Surgery and gain progressive autonomy. A learning plan is tailored toward the needs of the fellow and elective rotations in other pediatric surgical specialties, other pediatric hospital (typically the Montreal Children’s Hospital) or abroad internationally can be organized. The ultimate goal is to train a competent pediatric surgeon ready for an independent practice in an academic or non-academic position.
Institution Information
CHU Sainte-Justine
Montreal, QC Canada
Number of beds: 400 with 80 NICU and 32 PICU beds
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
The CHU Sainte-Justine is a francophone Level 1 trauma center with 12 000 traumas per year including 600 admissions in trauma. It has a 15-room surgery department where more than 10 000 surgeries are performed annually. It offers the whole breadth of highly specialized pediatric surgical services and is the training center for multiple pediatric fellowships training programs (Neonatology, Pediatric Intensive Care, and Maternal-Fetal Medicine), giving a rich opportunity for interaction with other pediatric fellows. CHU Sainte-Justine is also a kidney and liver transplant center and the fellows, depending of their interest, are welcome to be involved with the care of these patients. Since 2016, a new 7-story specialized unit building integrating clinical care and research has been added to the hospital. Specific opportunities for research include: oncology, clinical bioethics, simulation based training, and surgical education). The “Centre de simulation mère-enfant” is a simulation center located in the hospital allowing a facilitated access for interdisciplinary simulation activities.
Faculty Information
Program Director: Ann Aspirot, MD, FRCPC
Associate Program Director:
Program manager: Caroline Dufour
caroline.dufour.hsj@ssss.gouv.qc.ca
514-345-4688
Faculty:
Marianne Beaudin, MD, MPH, FRCPC
Mona Beaunoyer, MD, FRCPC
Sarah Bouchard, MD, FRCPC, FACS
Rebecca Brocks, MD, FACS
Michel Lallier, MD, FRCPC
Nelson Piché, MD, MSc, FRCPC, FACS
Dickens Saint-Vil, MD, FRCPC, FACS
Fellow Information
Number of fellows:
Alternately, one one year and two the other year for a total of three fellows
Current fellow(s):
James Saltsman
Kristen Calabro
Camille Plourde
Previous 5 fellows:
Dre Catherine K. Beaumier, 2018, Valley Children's Hospital, Merced, CA
Dre Josée Trébichavsky, 2018, CHUS, Université de Sherbrooke, Canada
Dre Danielle Leblanc, 2019, Blank Children's Hospital, Des Moines, IA
Dre Shahrzad Joharifard, 2020, BC Children's Hospital, University of British Columbia, Canada
Dr Shin Miyata, 2020, SSM Health Cardinal Glennon Children’s Hospital, St. Louis, MO, USA
Dre Maeve Trudeau, 2021, Montreal Children’s Hospital, University of Montreal, Canada
Curriculum Information
Block Schedule
| Description | Term | Center where training is given |
|---|---|---|
| General Pediatric Surgery | 21 periods | CHU Sainte-Justine |
| Pediatric Intensive Care | 1 period | CHU Sainte-Justine |
| Neonatalogy | 1 period | CHU Sainte-Justine |
1st Year
Home call Q3 for fellow-level /index cases (NICU, PICU, level 1 trauma)
5 home calls per month with Full Pediatric Surgery Coverage2nd Year
Home call Q3 for fellow-level /index cases (NICU, PICU, level 1 trauma)
5 home calls per month with Full Pediatric Surgery Coverage
Monday:
Trauma multidisciplinary meeting (weekly)
Prenatal diagnosis multidisciplinary meeting (twice a week)
Anorectal malformation multidisciplinary meeting (twice a month)
Tuesday:
GI rounds (weekly alternating between IBD and short gut)
NICU-surgery conference (every 2 months)
Wednesday:
Departmental scientific conference (monthly)
Tumor board (weekly)Protected academic half-day (9h00-12h00 weekly) including but not limited to:
Didactic courses, pedscore curriculum (weekly)
Review of interesting cases and discussion of upcoming cases (weekly)
Pathology review interesting cases (monthly)
M and M (monthly)
Journal club:
Pediatric scientific conference (weekly)
Multidisciplinary trauma simulation (monthy)
Multidisciplinary esophageal atresia meeting
Thursday:
Prenatal diagnosis multidisciplinary meeting (twice a week)
Pneumology-surgery conference
Friday:
Research conference
Special conferences:
Northeastern Rounds (three times a year)
Conference from University of Montréal (CanMEDS day and Research days)
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The Pediatric Surgery Academic Funds pays for Transition to Fellowship Bootcamp, MIS, and oncology courses. It also pays for meetings if the fellow is presenting on behalf of the division.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 800
Board passage rate (3 years): 100% passed the ABS
Fellow salary: N/A
Cincinnati Children's Hospital Pediatric Surgery Fellowship
Last updated: November 2024
Program website: https://www.cincinnatichildrens.org/education/clinical/fellowship/ped-surgery
At Cincinnati Children’s Hospital Medical Center, the Division of General and Thoracic Surgery offers a two-year residency (fellowship) in pediatric surgery. One new resident is chosen each year through the National Resident Matching Program. The applicant must have completed a general surgical training program and must be eligible to take the qualifying examination given by the American Board of Surgery. To date, more than 50 pediatric surgery fellows have been trained.
The fellowship is a two-year training program that emphasizes diverse clinical experience. In the first year, residents do a month-long rotation in neonatology, pediatric intensive care and colorectal surgery, as well as a two-week rotation in pediatric urology. The second-year chief resident’s responsibilities focus on managing the clinical care team along with the administration of the educational program. There are also two-week rotations in otolaryngology and vascular malformations along with a 4-week rotation in the fetal care center.
With faculty performing over 4100 operations annually, the pediatric surgical trainee gains extensive experience in managing a wide spectrum of common and complex pediatric surgical problems in neonates to young adults. This experience includes training in:
- Thoracic surgery
- Fetal surgery
- Abdominal surgery
- Urologic surgery
- Oncologic surgery
- Trauma surgery
- Transplant surgery
- Endoscopy
- Minimally invasive surgical techniques
The two-year curriculum combines structured rotations, didactic lectures and weekly and monthly educational conferences comprising:
- Pediatric surgery grand rounds
- Basic science lectures
- Radiology conference
- Tumor Board
- Morbidity and Mortality
- Trauma Conference
- Pathology Conference
The resident is also expected to engage in independent study and self-directed learning. He or she is given access to computerized databases, library materials and journals, and given the opportunity to participate in a variety of clinical and basic science research projects as well as Quality Improvement initiatives.
Pediatric surgery faculty members closely mentor the resident throughout training. More details can be found here.
Institution Information
Cincinnati Children’s Hospital Medical Center
Cincinnati, OH United States
Number of beds: 625
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
27k cases/year
Faculty Information
Program Director: Aaron P Garrison, MD
Associate Program Director: Director: Greg M. Tiao, MD
Program manager: Meghan Wiesner
meghan.wiesner@cchmc.org
513-803-9226
Faculty:
Alexander J. Bondoc, MD — Associate Professor, Pediatric and Transplant Surgery, Cincinnati Children’s Hospital Medical Center, Associate Professor, Surgery, UC Department of Surgery
Rebeccah L. Brown, MD, FACS, FAAP — Associate Director, Trauma Services; Director, Pediatric Trauma Fellowship; Co-Director, Chest Wall Center; Professor, UC Department of Surgery
Rebeccah Brown, MD, FACS, FAAP — Professor, Pediatric Surgery, Co-Director: Chest Wall Center, Pilonidal Center, Cincinnati Children’s Hospital Medical Center, Professor, Surgery
UC Department of Surgery
- Roshni Dasgupta, MD, MPH — Professor, Pediatric Surgery, Surgical Director Vascular Malformations Center, Director, Vascular Malformations Fellowship, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of SurgerySue Evans, MD — Assistant Professor, Surgery, Cincinnati Children’s Hospital Medical Center
Assistant Professor, Surgery, UC Department of Surgery
Richard A. Falcone Jr., MD, MPH — Chief of Staff; Professor, Pediatric Surgery, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Jason S. Frischer, MD — Professor, Pediatric Surgery; Director, Colorectal Center, Extracorporeal Membrane Oxygenation (ECMO) Program, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Laura Galganski, MD — Assistant Professor, Pediatric Surgery, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Victor F. Garcia, MD, FACS, FAAP — Professor, Pediatric Surgery, Founding Director, Trauma Services; Co-Director, Chest Wall Center, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Aaron P. Garrison, MD — Associate Professor, Pediatric Surgery; Program Director, Pediatric Surgery Fellowship, Cincinnati Children’s Hospital Medical Center, Associate Professor, Surgery
UC Department of Surgery
Juan P. Gurria, MD – Assistant Professor, Pediatric Surgery; Program Director, Surgical Critical Care Fellowship, Cincinnati Children’s Hospital Medical Center, Assistant Professor, Surgery
UC Department of Surgery
Michael A. Helmrath, MD, MS — Professor, Pediatric Surgery; Surgical Director, Intestinal Rehabilitation; Director of Surgical Research; Associate Director of Clinical Translation, CuSTOM; Co-Director, Center of Bariatric Surgery, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Meera Kotagal, MD, MPH — Assistant Professor, Pediatric Surgery; Director, Pediatric Surgery Global Health Program, International Fellowship, Cincinnati Children’s Hospital Medical Center
Assistant Professor, Surgery, UC Department of Surgery
Foong-Yen Lim MD — Associate Professor, Pediatric Surgery; Surgical Director, Cincinnati Fetal Center, Cincinnati Children’s Hospital Medical Center, Associate Professor, Surgery, UC Department of Surgery
Jonathan Merola, MD — Assistant Professor, Surgery, Cincinnati Children’s Hospital Medical Center
Assistant Professor, Surgery, UC Department of Surgery
Jose L. Peiro, MD — Associate Professor, Pediatric Surgery; Director, Endoscopic Fetal Surgery Cincinnati Fetal Center, Cincinnati Children’s Hospital Medical Center, Associate Professor, Surgery
UC Department of Surgery
Todd A. Ponsky, MD — Professor, Pediatric Surgery; Director, Clinical Growth and Transformation;
Cincinnati Children’s Hospital Medical Center, Associate Professor, Surgery, UC Department of Surgery
Nelson G. Rosen, MD — Professor, Pediatric Surgery; Associate Director, Colorectal Center; Director, Colorectal Fellowship, Cincinnati Children’s Hospital Medical Center, Professor, Surgery
UC Department of Surgery
Beth A. Rymeski, DO — Associate Professor, Pediatric Surgery, Cincinnati Children’s Hospital Medical Center, Associate Professor, Surgery, UC Department of Surgery
Gregory M. Tiao, MD — Division Director, Pediatric Surgery; Associate Program Director, Pediatric Surgery Fellowship; Surgical Director, Liver Transplantation; Frederick C. Ryckman Chair of Pediatric Surgery, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Daniel von Allmen, MD — Surgeon-in-Chief; Lester W. Martin Chair of Pediatric Surgery; Senior Vice President, Surgical Services; Director, Esophageal Center, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Paul Wales, BSc, MD, MSc, FRCSC, FACS — Professor, Pediatric Surgery; Surgical Director, Intestinal Rehabilitation, Cincinnati Children’s Hospital Medical Center, Professor, Surgery, UC Department of Surgery
Ashley Walther, MD — Assistant Professor, Pediatric Surgery, Surgical Lead, Aerodigestive and Esophageal Center, Co-Director, Center of Bariatric Surgery, Cincinnati Children’s Hospital Medical Center. Assistant Professor, Surgery, UC Department of Surgery
Fellow Information
Number of fellows: one per year
Current fellow(s):
Numa Perez, MD (Senior)
Andrew Hu, MD (Junior)
Previous 5 fellows:
Byron Hughes, MD
2024
C.S. Motts Children’s Hospital
Laura Galganski, MD
2023
Cincinnati Children’s Hospital Medical Center
Irene “Iris” Lim-Beutel, MD
2022
Children’s Mercy, Kansas City
Eric Rellinger, MD
2021
University of Kentucky Healthcare
Christina Feng, MD
2020
Children’s National Hospital
Curriculum Information
Call Schedule
1st year: In the first few months of fellowship the junior fellow will do one in house call per week.
The remainder of the year is spent alternative home call with the senior fellow.
2nd year: Home call, alternating with junior fellow – Q2
Conference Schedule
Every Wednesday:
1200 – Radiology Conference, combined Pathology/Surgery Conference, Trauma Case Review Conference
1500 – Morbidity and Mortality
1600 – Grand Rounds
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Meeting/Training Course policy: First year Fellows attend APSA and second year Fellows attend AAP.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: 1301
Board passage rate (3 years): 100%
Fellow salary: According to Post Graduate year
Cohen Children's Medical Center- Northwell Health
Last updated: 09/14/2021
Program website: https://professionals.northwell.edu/graduate-medical-education/fellowship-pediatric-general-surgery-cohen-children-medical-center
The Zucker School of Medicine at Hofstra-Northwell offers a two-year clinical fellowship training program in pediatric surgery at the Cohen Children’s Medical Center. The program offers a broad experience in all aspects of pediatric general surgery with extensive training in minimally invasive surgery, pediatric oncology, inflammatory bowel disease and neonatal surgery.
Institution Information
Cohen Children’s Medical Center
New Hyde Park, NY United States
Number of beds: 202
Percentage of time at this location: 95%
Training site type: Free standing children’s hospital
Cohen Children’s Medical Center is a major referral center for many pediatric surgical conditions including chest wall abnormalities, solid tumors, colorectal issues and complex neonatal anomalies. Cohen Children’s is the pediatric service line hub for the Northwell Health System (formerly NSLIJ) which encompasses 21 hospitals and over 42,000 births annually. In addition, Cohen Children’s is the major pediatric referral center for many other hospitals throughout Long Island, Brooklyn, and Queens and the only stand-alone ACS Accredited Level 1 pediatric trauma center in the region. The hospital is one of the leading ECMO centers in the New York-metro area. The training program features an extensive minimally invasive surgery experience, with all advanced laparoscopic and thorascopic procedures being performed by many of the faculty staff. Previous graduates of our program have been recognized for their superior minimally invasive skill sets by their future employers. Approximately 2200 ambulatory and inpatient cases are done by the pediatric general surgery service at Cohen Children’s each year.
Memorial Sloan Kettering Cancer Center
New York, NY United States
Number of beds: 50
Percentage of time at this location: 5%
Training site type: Children’s hospital within adult hospital
Faculty Information
Program Director: Samuel Soffer, MD
Associate Program Director: Aaron Lipskar, MD
Program manager: Roseanne Milano
rmilano@northwell.edu
718-470-3135
Faculty:
Stephen Dolgin, MD
Richard Glick, MD
Andrew Hong, MD
Barrie Rich, MD
Jose Prince, MD — Division Chief
Chethan Sethya, MD
Larry Bodenstein, MD
Colleen Fitzpatrick, MD
Whitney Mcbride, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Charlotte Kvasnovsky, MD
Key Nguyen, MD
Previous 5 fellows:
Naina Bagrodia,MD
2021
Cohen Children’s Medical Center/ Kings County Hospital Center
New Hyde Park, NY
Yan Shi, MD
2020
Texas Children’s Hospital
Houston, Texas
Rohini Olson, MD
2019
East Carolina Children’s Hospital
Greenville, North Carolina
Nathan Heinzerling, MD
2018
Akron Children’s Hospital
Akron, Ohio
Meade Barlow, MD
2017
Tacoma Children’s Hospital
Tacoma, Washington
Curriculum Information
1st year: home
2nd year: home
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Pays for St Jude Course, MIS course, Colorectral course, AAP surgical section, APSA
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1300
Board passage rate (3 years): 100% written, 90% oral
Fellow salary: First Year Fellow: $81,500; Second Year Fellow: $83,000
Dalhousie University, Halifax, Nova Scotia, Canada
Last Updated: October 2024
Program Name
Dalhousie University, IWK Health
Program web page URL
https://medicine.dal.ca/departments/department-sites/surgery/divisions/pediatric-surgery.html
Overview of Fellowship
Our Pediatric General and Thoracic Surgery program is a 2-year training program affiliated with the Dalhousie University Department of Surgery and accredited by the Royal College of Physicians and Surgeons of Canada. Prospective candidates have usually completed 5-year General Surgery training in the US or Canada and complete an application through the Electronic Residency Application Services (ERAS). We select a new fellow every other year through the National Resident Matching Program (NRMP). Training spans from Aug 1st to July 31st on even years, which means that we participate on the interview process and the match on odd years.
Our program seeks highly-qualified and motivated individuals whose main goal is to become a clinically strong, academically inclined surgeon capable of:
- Tackling most pediatric surgical conditions in an academic environment.
- Developing solid communication skills and a team-based work mentality.
- Demonstrating empathy and compassion towards patients and their families.
Strengths:
- Large catchment area with no competition for index cases (neonatal surgery, oncology, etc.) in the region due to the nature of the Canadian healthcare system.
- Close and collegial relationship between faculty and fellow, which provides a “junior attending” experience during the fellowship.
- Manageable case load for a single fellow with a high complex-to-simple case ratio.
- Flexibility for involvement with pediatric urology cases and other areas of pediatric surgery (ENT, cardiac) based on interest and career goals.
Weaknesses:
- Low trauma volume.
- Senior / junior fellow interaction not available since one fellow program.
- No exposure to transplant surgery
Institution Information
Training site #1:
Name: IWK Health, Halifax, NS, Canada
Number of Beds: 122 children's beds
Percentage of time at this location: 100%
Training site type: free standing children’s hospital
IWK Health is the only children’s Hospital serving the Eastern Canada Maritime provinces (Nova Scotia, New Brunswick and Prince Edward Island). It is one of the teaching hospitals associated with the 200-year old Dalhousie University and the sole tertiary referral center for pediatric surgery and level I trauma center for the entire region, a catchment area of approximately 2 million people.
Our unique geographic position and distance from other children’s hospitals offer opportunity for excellent clinical experience in index pediatric surgery cases. The IWK enjoys a full complement of pediatric surgical and medical subspecialties with the resulting exposure to the complete spectrum of pediatric conditions and opportunities for multidisciplinary coordination.
Faculty Information
Program Director
Christopher Blackmore
Christopher.blackmore@iwk.nshealth.ca
Program manager and contact info
N/A
Faculty:
Christopher Blackmore MD, MSc, FRCSC
Dafydd Davies MD, MPhil, FRCSC
Jessica Mills MD, FRCSC
Karen Milford MD, FRCSC
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Olga Bednarek
List of previous 5 fellows:
Krista Lai 2024: Pediatric Surgeon in Fresno, CA
Mackenzie Lees, 2022: Pediatric surgeon in Des Moines, IA (starting Jan 2023)
Natashia Seeman 2020: Pediatric surgeon in London, ON
Christopher Blackmore 2018: Pediatric surgeon in Halifax, NS
Victoriya Staab 2016: Pediatric surgeon in Neptune City, NJ
Curriculum Information
Block schedule:
1st year – NICU (4 weeks), PICU (4 weeks) and Pediatric Surgery Service
2nd year – Pediatric Surgery, electives available based on interest (Urology, ENT / Airway, CV surgery)
Call schedule:
1st year: Q4 home call
2nd year: Q4 home call
Conference Schedule:
Pediatric Surgery Teaching Rounds / Academic halfday
Radiology Rounds
Neonatal quality meeting
Tumor Boards
QI / M&M Rounds
Journal club
Research Rounds
Program Information
Full Accreditation by the Royal College of Physicians and Surgeons of Canada with next review planned for 2026.
Accredited since 1988.
Meeting/Training Course policy (Does program pay for courses or meetings? e.g. our program would say, “Pays for one meeting and one course per year plus any additional meetings if fellow presenting own work. Time away subject to RRC regulations governing time in training”)
Our program covers the costs for the following meetings:
- One Pediatric Surgery meeting per year (CAPS or APSA)
- Pediatric Surgery Boot Camp
- Colorectal, and MIS Courses in 1stor 2ndyear
- Oncology (St. Jude) course in 2ndyear
- AAP Job Fair 2ndyear
One Pediatric Surgery meeting per year (CAPS or APSA) plus additional meetings if presenting own work.
Pediatric Surgery Boot Camp
Colorectal, MIS, Oncology (St. Jude) courses 2nd year
AAP Job Fair 2nd year
Does the program provide financial support for candidate interviews? No
Optional information
What is the average total number of cases performed by your graduating fellows over the past five years?: 950 cases
Board Passage rate (last ten years): 100%
Fellow Salary: Updated Contract information can be found at:
https://www.maritimeresidentdoctors.ca
Starting July 30, 2024: PGY 6 – $97,968 CAD; PGY 7 – $103,870 CAD
Emory University/Children's Healthcare of Atlanta
Last updated: September 2023
Program website: http://www.surgery.emory.edu/specialties-and-programs/pediatric_surgery/pediatric-surgery-residency.html
The pediatric surgery fellowship of the Emory University School of Medicine is an ACGME approved two-year program. During the training period, fellows are responsible for the care of pre- and post-operative patients in both inpatient and outpatient clinic settings. As fellows master increasingly difficult skills and become adept at communicating with children and parents, they are assigned higher levels of responsibility in and out of the operating room. The Division of Pediatric Surgery offers a comprehensive didactic curriculum examining all major topics in pediatric surgery. Fellows participate in weekly conferences on morbidity and mortality, pediatric radiology and pediatric oncology; attend bimonthly lectures on basic science topics; and participate in a monthly pediatric surgical pathology conference and journal club. Pediatric surgery residents present a weekly pediatric surgery conference for surgical and pediatric house officers, pediatric and surgical attendings, and nurses. In addition to clinical efforts, pediatric surgery fellows are expected to participate in the division's research mission. Studies driven by pediatric surgery fellows are strongly encouraged and will ideally result in original work being presented and published on the national/international level.
Institution Information
Children's Healthcare of Atlanta, Egleston
Atlanta, GA United States
Number of beds: 340
Percentage of time at this location: 95%
Training site type: Free standing children's hospital
On average, ~6500 cases/year including Scottish Rite
Children's Healthcare of Atlanta, Scottish Rite
Atlanta, GA United States
Number of beds: 325
Percentage of time at this location: 5%
Training site type: Free standing children's hospital
Faculty Information
Program Director: Matthew S. Clifton, MD
Associate Program Director:
Program manager: Nena Buie
bbuie@emory.edu
404-727-4375
Faculty:
Hanna Alemayehu, MD
Ross Beckman, MD
Amina Bhatia, MD
Alfred Chahine, MD
Matthew Clifton, MD
Megan Durham, MD
Allison Linden, MD
Jonathan Meisel, MD
Paul Parker, MD
Matthew Santore, MD
Heather Short, MD
Alexis Smith, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Christina “Nina” Bence, MD
Megan Bouchard, MD
Previous 5 fellows:
Sarah Rinke. MD, 2023
Robert Vandewalle, MD, 2022 (Assistant Professor, Arkansas Children’s Hospital, Little Rock, AR)
Heather Short, MD, 2021 (Staff Surgeon, Children’s Healthcare of Atlanta, Atlanta, GA)
Morgan Richards, MD, 2020 (Staff Surgeon, St. Luke’s Hospital, Boise, ID)
Irving Zamora, MD, 2019 (Assistant Professor, Vanderbilt University, Nashville, TN)
Curriculum Information
Call Schedule
1st year: Q4
2nd year: Q4
Conference Schedule:
- M&M/Staff Rounds: Weekly review of morbidity and mortality and presentations of pediatric topics geared to the surgical residents.
- Weekly Radiology Conference: Review of interesting cases.
- PedSCORE/Basic Science Conference: Meets three times a month to discuss topics within pediatric surgery and includes guest lecturers from other disciplines; geared to the Fellow. Score modules used as curriculum for pediatric surgery component and are oral boards format.
- Tumor Board: Weekly multi-disciplinary discussion of current patients with malignancies.
- Neonatology lecture series: at Grady during introduction to neonatology rotation.
- Pathology/Radiology Conference: Multi-disciplinary monthly presentations of the most interesting cases from our service.
- Journal Club: Monthly review of current literature, Friday morning.
- Weekly General Surgery “Grand Rounds.”
- GI/Surgery Conference: quarterly meeting of services to discuss patients that require multi-disciplinary input/care.
- Albatross/Zebra Conference: quarterly meeting to discuss unusual or challenging cases.
- NICU/Surgery Conference: quarterly meeting of services to discuss patient care issues that cross both specialties.
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: (Does program pay for courses or meetings? e.g. our program would say, “Pays for one meeting and one course per year plus any additional meetings if fellow presenting own work. Time away subject to RRC regulations governing time in training”)
Attendance at both the American Academy of Pediatrics (senior resident) and American Pediatric Surgical Association (junior resident) is supported. Senior residents traditionally attend the Pediatric Anorectal and Colorectal Surgical Workshop, the Advanced Minimally Invasive Surgery Course, and the Pediatric Surgical Oncology Review Course.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1300-1400
Board passage rate (3 years): 100%
Fellow salary:
PGY-6: $75,110
PGY-7: $76,403
PGY-8: $78,397
Johns Hopkins All Children's Hospital
Last updated: March 2024
Program website: https://www.hopkinsmedicine.org/all-childrens-hospital/academics/education/office-of-medical-education/fellowships/pediatric-surgery-fellowship
The faculty of the Division of Pediatric Surgery at the Johns Hopkins All Children’s Hospital offer a two year, ACGME-accredited pediatric surgery clinical fellowship for BC/BE general surgeons. One fellow is selected through the National Resident Matching Program (NRMP) on a yearly basis. The fellowship provides a broad exposure to all facets of general pediatric surgery including head & neck surgery, endocrine, oncology, gastrointestinal surgery, gynecology, endoscopy, minimally invasive surgery, thoracic surgery, ECMO, trauma care, vascular anomalies, wound care, congenital diaphragmatic hernia management, and esophageal and airway treatment. Candidates choose JHACH due to the high clinical volume, diverse faculty, and mentorship. Our hospital mission focuses on clinical care, education, quality, and research. Therefore, we favor candidates with 1) a strong background in clinical general surgery, 2) significant evidence of scholarly achievement, and 3) a desire to pursue a career in academic pediatric surgery.
Strengths
- Congenital Diaphragmatic Hernia Program (only dedicated CDH unit in the nation)
- ECMO program
- Esophageal/airway reconstruction
- Minimally invasive surgery including pediatric single incision laparoscopy, and broad general, neonatal and oncologic surgical exposure
Weakness
- Johns Hopkins All Children’s Hospital does not perform kidney, liver or intestinal transplantation.
Institution Information
Johns Hopkins All Children's Hospital
St. Petersburg, FL United States
Number of beds: 259
Percentage of time at this location: 100%
Training site type: Free-standing children's hospital
Johns Hopkins All Children’s Hospital (JAHC) is a 259 bed free standing children’s hospital and which admits patients from the age of 0-21 years. It is the sponsoring institution for a pediatric residency, child neurology residency, and twelve fellowship programs. Additionally, JHACH is a participating site for three ACGME institutions, University of South Florida Morsani College of Medicine. HCA Healthcare and Bayfront Health, covering a variety of residency, fellowship, and medical student rotations. The institution is home to a regional pediatric trauma center, a congenital cardiac disease and cardiac transplant center, a pediatric oncology and bone marrow transplant center, a neuroscience institute, a maternal and neonatal diseases institute, as well as the Congenital Diaphragmatic Hernia and ECMO Program. The hospital’s divisions of radiology, pathology, critical care, pediatric hospitalist medicine, and emergency medicine are solely focused on pediatric care and operate 24 hours per day. The facility has 97 NICU beds, 28 Cardiovascular ICU beds, 22 PICU beds, 15 congenital diaphragmatic hernia/ECMO beds, 28 specialized surgery-neuroscience ward beds, 28 oncology/bone marrow transplant unit beds, and 41 general medical/surgical beds. The average daily census on the pediatric surgical service is 30 with patients distributed throughout the various units within the hospital. Johns Hopkins All Children’s Hospital is one of the teaching hospitals of the Johns Hopkins School of Medicine. Although Johns Hopkins has many affiliates around the country and the world, Johns Hopkins All Children’s is one of only six that meet the standards and criteria to be operated by Johns Hopkins Medicine.
Faculty Information
Program Director: Nicole M. Chandler, MD, FACS, FAAP
Associate Program Director: Henry Chang, MD
Program manager: Israel Marmolejos
imarmol2@jh.edu
727-767-8813
Faculty:
Nicole Chandler, MD
Henry Chang, MD
Paul Danielson, MD
Raquel Gonzalez, MD
Amanda Harrington, MD
Russel Jennings, MD
David Kays, MD
Hester Shieh, MD
J. Charles Smithers, MD
Christopher Snyder, MD
Keith Thatch, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Gabriel Ramos Gonzalez, MD
Alicia Sykes, MD
Previous 5 fellows:
Ali Mokdad
July 2023
Cook Children’s Fort Worth, TX
Lindsey Armstrong, MD
July 2022
Advent Health Orlando, FL
Heather Nolan
July 2021
Ascension, Studer Family Children’s Hospital Pensacola, FL
Katherine Gonzalez, MD
July 2020
Division of Pediatric Surgery, St. Luke’s Children’s Hospital Boise, ID
Jason O. Robertson, MD
July 2019
Assistant Professor of Surgery Case Western University, Cleveland Clinic Children’s
Cleveland, Ohio
Christopher W. Snyder, MD
July 2018
Medical Director, Pediatric Trauma Program; Assistant Professor of Surgery, Johns Hopkins University
Johns Hopkins All Children’s Hospital St. Petersburg, Florida
Varun Bhalla, MD
June 2017
Assistant Professor of Surgery University of South Carolina, Prisma Health Children’s Hospital
Columbia, South Carolina
Margaret M. McGuire, MD
June 2016
Children’s Hospital of the King’s Daughter Norfolk, VA
Curriculum Information
Call Schedule
The fellows share home call with the senior general surgery resident. Each fellow takes one in-house shift per month as surgical intensivist in the Center for Congenital Diaphragmatic Hernia Unit
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The program will support “away” courses as part of a career development plan (e.g., Surgery board prep, Oncology course, Colorectal course, MIS course, Transition to Fellowship Bootcamp). The fellow will attend one professional society meeting per year (APSA, AAP or ACS) plus any additional meetings if the fellow is presenting scholarly activity from the program. Time away is subject to RRC regulations governing time training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1327
Board passage rate (3 years): 100%
Fellow salary: PGY-6: $76,083, PGY-7: $80,605
The program provides a $1000/month housing stipend.
Johns Hopkins University
Last updated: 08/29/2024
Program website: https://www.hopkinsmedicine.org/pediatricsurgery/fellowship/
Founded in 1912 as the Harriet Lane Home for Children, the Johns Hopkins Children's Center offers one of the most comprehensive pediatric medical programs in the country, with more than 92,000 patient visits and nearly 9,000 admissions each year. It is Maryland’s largest children’s hospital with 205 beds and the only state-designated Trauma Service and American Burn Association-Accredited Burn Unit for pediatric patients. Patients from age 0-21 are admitted to the Children's Center. The facility is equipped for all aspects of general pediatric care, with a 40-bed intensive care unit (PICU), a 45-bed neonatal intensive care unit (NICU) and laboratory and radiology facilities. A pediatric medical and surgical oncology ward (14 beds), psychiatric wards and general pediatric age-determined wards complete the inpatient facility. A suite of 10 operating rooms for children's surgery and a pediatric recovery room adjacent to the PICU are utilized by pediatric general surgery, urology, orthopedics, neurosurgery, and otolaryngology services. The Johns Hopkins Outpatient Center houses the clinical facilities for outpatient visits (approx. 45,000/year). The Park Building, adjacent to the Children's Center, has a pediatric emergency room, oncology and hematology clinics, and a perfusion center.
The pediatric surgical staff at the Johns Hopkins Hospital is under the direction of David J. Hackam, MD, PhD, The Robert Garrett Professor of Pediatric Surgery and co-director of Johns Hopkins Children’s Center. There are also full-time specialty surgeons in pediatric orthopedics, urology, neurosurgery, otolaryngology, plastic and cardiovascular surgery.
Under the direction of Samuel M. Alaish, M.D., the post-doctoral training program in Pediatric Surgery at The Johns Hopkins Hospital and the University of Maryland Medical Center is unique in concept, because it utilizes the clinical population of two large university services for a broad clinical experience in pediatric surgery over the prescribed two years. Both divisions of Pediatric Surgery perform more than 3,200 operations annually and have a staff of 14 pediatric surgeons. Completion of the basic two-year program will qualify the trainee to take the examination for a “Certificate of Special Competence in Pediatric Surgery,“ which is given by the American Board of Surgery.
History
Support of pediatric surgery by the Robert Garrett Foundation began in the 1940s. These funds enabled Dr. Alfred Blalock to conduct his animal laboratory experiments on congenital heart disease and helped support Dr. Helen Taussig with her clinical evaluation of children with cyanotic congenital heart disease. These studies led to the development of the Blalock-Taussig shunt and culminated in the first clinical use of their subclavian artery-pulmonary artery anastomosis for a child with tetralogy of Fallot in November 1944. In 1964, Dr. J. Alexander Haller became the first pediatric surgeon-in-charge of The Johns Hopkins Hospital and Chief of the Division of Pediatric Surgery. Later that year, Dr. Haller finished training the first chief resident in pediatric surgery, Dr. James L. Talbert, who left to become the Chief of Pediatric Surgery at the University of Florida in Gainesville. In 1976, Dr. J. Laurence Hill was recruited to the University of Maryland with a joint appointment at Johns Hopkins Hospital in 1977. With Dr. Hill’s arrival, the first integrated training program in pediatric surgery was born. In 1991, Dr. Paul M. Colombani was appointed the pediatric surgeon-in-charge and second Garrett Professor of Pediatric Surgery. Following Dr. Colombani’s departure in 2014, Dr. David J. Hackam became the third Garrett Professor of Pediatric Surgery and Co-director of the Johns Hopkins Children’s Center. In 2015, Dr. Samuel M. Alaish became the fourth training director, following Dr. Fizan Abdullah’s move to Lurie Children’s Hospital of Chicago.
Since 1965, a long line of talented and accomplished people have graduated from our fellowship. Notable alumni include James Talbert ’65, Paul Colombani ’83, Richard Azizkhan ’85, Francisco Cigarroa ’93 and Jessica Kandel ’95 to name just a few.
Institution Information
Johns Hopkins Children’s Center
Baltimore, MD United States
Number of beds: 205
Percentage of time at this location: 87.5%
Training site type: Children's hospital within adult hospital
University of Maryland Medical Center
Baltimore, MD United States
Number of beds: 800
Percentage of time at this location: 12.5%
Training site type: Children's hospital within adult hospital
Faculty Information
Program Director: Samuel M. Alaish, MD
Associate Program Director: Mark Slidell, MD
Program manager: Katy Bender
kbuckle9@jhmi.edu
410-955-9012
Faculty:
Johns Hopkins University
David Hackam, MD, Garrett Professor of Pediatric Surgery, Co-Director and Surgeon-in-Chief, Johns Hopkins Children’s Center
Samuel Alaish, MD Associate Professor of Surgery, Associate Division Chief of Clinical Operations and Education, Director, Fellowship in Pediatric Surgery, Surgical Director, THRIVE Pediatric Intestinal Rehabilitation Program, Johns Hopkins Children’s Center
Shaun Kunisaki, MD, Professor of Surgery, Associate Division Chief of Strategy and Integration, Director, Pediatric Esophageal Surgery
Isam Nasr, MD, Assistant Professor of Surgery, Director of Pediatric Trauma Program
Alejandro Garcia, MD, Associate Professor of Surgery, Director of ECMO Program
Erica I. Hodgman, MD, Assistant Professor of Surgery, Director, Burn Program
Daniel Rhee, M., Associate Professor of Surgery, Director, Pediatric Surgical Oncology
Clint Cappiello, MD Assistant Professor of Surgery, Director, Pediatric Surgery Residency Education
Mark Slidell, Associate Professor of Surgery, Associate Program Director
University of Maryland
Kimberly M. Lumpkins, MD, Surgeon-in-Chief, Associate Professor of Surgery, University of Maryland Hospital for Children
Eric D. Strauch, MD, Associate Professor of Surgery, University of Maryland
James T. Moore, MD, Assistant Professor of Surgery, University of Maryland
Helena M. Crowley, MD, Assistant Professor of Surgery, University of Mar
Brian Englum, M.D. Assistant Professor of Surgery, University of Maryland
Fellow Information
Number of fellows: one per year
Current fellow(s):
Stephen Niemiec, M.D., Senior fellow
Richard Guyer, M.D., Ph.D., Junior fellow
Previous 5 fellows:
2020
Felipe Pedroso, MD
Miami Children’s Hospital, Miami, FL
2021
Yue Julia Chen, MD
Dell Children’s Medical Center, Austin, TX
2022
Mitchell Ryan Ladd, MD, PhD
Assistant Professor of Surgery, Wake Forest Baptist Medical Center, Winston-Salem, NC
2023
R. Ellen Jones, MD
Cook Children’s Medical Center, Dallas, TX
2024
Mollie Freedman-Weiss, MD
Assistant Professor of Surgery, Weill Cornell Medical Center, New York, NY
Curriculum Information
Block Schedule
First Year of Training Program, Senior Resident in Pediatric Surgery
The first year of the training program is designed to expose the resident to general pediatric surgery and a number of surgical and pediatric subspecialties. The first two months are spent at Johns Hopkins Hospital with an August rotation in the pediatric intensive care unit and a September rotation in the neonatal intensive care unit. The next three months are spent on the General Pediatric Surgery service at Johns Hopkins. The following three months are spent as the Chief Resident in pediatric surgery at the University of Maryland Hospital under the supervision of Dr. Lumpkins and staff. Patients admitted to the pediatric surgical service are evaluated and treated under the Chief Resident’s direction. Care of surgical patients in the pediatric and neonatal intensive care units is the responsibility of the surgical housestaff under the supervision of this Chief Resident in pediatric surgery. At the University of Maryland, the Chief Resident is responsible for housestaff and student teaching on rounds and in the operating room. He/she organizes the weekly pediatric surgery conference and professors walk rounds as well as presentation of patients at the weekly General Surgical Morbidity and Mortality Conference, monthly Pathology Conference and monthly Radiology Conference.
The pediatric surgery faculty at the University of Maryland have active clinical and laboratory research projects, and the Chief Resident is encouraged to participate in ongoing research or guided to begin an independent project.
During the last four months, the first-year fellow returns to The Johns Hopkins Hospital on General Pediatric Surgery and works with the senior fellow in the clinical care of patients both inside and outside of the OR.
Second year of Training Program, Chief Resident in Pediatric Surgery
The second year of the two-year program is a diverse clinical year as Chief Resident. The responsibility of the Chief Resident is to supervise and coordinate pre-operative and post-operative care of all children with surgical conditions in the Johns Hopkins Children's Center. The Chief Resident renders direct surgical care to patients with problems in general pediatric, gynecologic, and all non-cardiac thoracic surgery. The Chief Resident coordinates patient care in the statewide regional pediatric trauma center and thus supervises the initial neurosurgical, orthopedic, plastic surgical and critical care for more than 1000 severely injured children each year. He/she provides surgical consultation services for all divisions of the Children's Center and is thus involved in the general management of patients on the medical and surgical subspecialty services. He/she is the consultant for most surgical problems in the pediatric emergency room and outpatient clinics, particularly in the comprehensive child care clinic where more than 18,000 children are seen annually.
The overall management of surgical patients in the pediatric ICU and neonatal ICU is the primary responsibility of the Chief Resident and pediatric surgical housestaff working with the attending pediatric surgeons, staff intensives and neonatologists who attend in these units.
Trauma and Burn patients in the pediatric intensive care unit (PICU) remain on the pediatric surgery service and are cared for by an integrated housestaff. The responsibility for moment-to-moment ventilator adjustment and respiratory support is delegated to the pediatric intensive care residents, but the overall responsibility for the writing of medication orders and patient management, including cardiorespiratory support, remains with the pediatric surgery housestaff. The physician of record is the Staff Pediatric Surgeon. Neonatal surgical patients are managed in a combined medical and surgical newborn intensive care unit (NICU), which is supervised by full-time neonatologists. Direct patient management is rendered by the pediatric surgical service working with the pediatric housestaff assigned to a particular surgical patient in the NICU.
Both the Chief Resident and Senior Resident share teaching responsibilities with the full-time surgical staff. Housestaff and student teaching on afternoon ward rounds, as well as weekly formal discussions for students, are the responsibilities of the residents in pediatric surgery.
Call Schedule
Fellows share home call at Johns Hopkins. While at the University of Maryland, the junior fellow takes only home call for the University of Maryland. Fellows receive 1 day off each week. Rarely, a fellow may take in-house call at Johns Hopkins to accommodate the schedule.
Conference Schedule
Weekly
General Pediatric Surgery (GPS) Core Curriculum, Morbidity and Mortality Conference, Halsted Surgery Grand Rounds, Fetal Conference, Goals of Care Multidisciplinary Rounds, Pediatric Grand Rounds, Pediatric Nutrition Rounds and Hackam/Alaish/Nasr Combined Lab Meeting, Tumor Board
Biweekly
GPS Clinical Research Conference
Monthly
GPS/Neonatology Conference, Trauma M and M, Trauma QI, Burn M and M, Burn QI, THRIVE Pediatric Intestinal Rehabilitation Multidisciplinary Conference and CDH Multidisciplinary Workshop Conference
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The fellows have a travel budget to be used to attend meetings of their choice over the two years. Meetings have included the Lurie Children’s MIS course, the St. Jude Pediatric Surgical Oncology course, APSA’s Annual Meeting, the AAP Section on Surgery Meeting and a colorectal course (highly encouraged). Should a fellow have a paper on a program, additional funds will be allotted to pay for travel. We have used other funds in the past to pay for the fellow to attend the Transition to Fellowship and the Transition to Practice Courses.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1342
Board passage rate (10 years): 95%
Fellow salary: The 2023-2024 academic year annual compensation levels are as follows: PGY 6 (Year 1 Fellow) $89,458; PGY 7 (Year 2 Fellow) $92,536
Le Bonheur Children’s Hospital Pediatric Surgery Fellowship - University of Tennessee Health Science Center
Last updated: September 2023
Program website: http://uthsc.edu/surgery/pediatric-surgery/index.php
The Pediatric Surgery fellowship program at the University of Tennessee Health Science Center in conjunction with Le Bonheur Children’s Hospital seeks diverse candidates who have completed an ACGME‐accredited (or its equivalent) general surgery training program and is interested in advancing their knowledge and training in the surgical management of infants and children. The goals of the program are to teach fellows the skills necessary to consistently deliver excellent and state‐of‐the‐art patient care, to appraise and assimilate new scientific evidence, to grow professionally with constant self‐evaluation and life‐long learning, and to participate in the process of research and discovery to advance patient care for the future. The faculty provides training in an environment that is sensitive to cultural diversity and seeks to be responsive to health care disparities. At the completion of this education, fellows will function as successful independent pediatric surgeons and can excel both in academic and private practice settings.
Institution Information
Training Site #1:
Le Bonheur Children's Hospital
Memphis, TN United States
Number of beds: 255
Percentage of time at this location: 83.3%
Training site type: Free standing children's hospital
Le Bonheur Children’s Hospital offers top‐tier pediatric training programs in a patient‐ and family‐centered environment. Named a “Best Children’s Hospital” by U.S. News & World Report for nine consecutive years, our 255‐bed state‐of‐the‐art facility has more than 750 medical staff and 45 pediatric specialties. Le Bonheur is designated as a Level 1 pediatric trauma center by the American College of Surgeons. The only Level 1 pediatric trauma center in the state and one of only 33 in the Country. It is also a Magnet‐designated hospital, a distinction given by the American Nurses Credentialing (ANCC), which is the ultimate credential for high‐quality care, nursing excellence and innovations in professional nursing practice. Our academic affiliation with the University of Tennessee Health Science Center (UTHSC) in Memphis, along with our premier academic partner, St. Jude Children’s Research Hospital, delivers a transformational education experience for our fellows. Because of our strong commitment to quality improvement, patient safety and transparency in health care, we participate in Children’s Hospitals Solutions for Patient Safety and many other collaboratives and registries. In 2017, we were named a Leapfrog Top Hospital, which is widely regarded as the most competitive designation for quality and patient safety among hospitals. More information is available at www.lebonheur.org.
Training Site #2:
St. Jude Children's Research Hospital
Memphis, TN United States
Number of beds: 78
Percentage of time at this location: 12.5%
Training site type: Free standing children's hospital
Integrally associated with Le Bonheur is St. Jude Children’s Research Hospital. Founded in 1962 by the late entertainer Danny Thomas, this unique institution is a world‐renowned institution in the clinical care and research of children’s cancer. In 1996 St. Jude opened its state‐of‐the‐art surgical complex and established a Department of Surgery. Since then our surgeons have been an integral part of the diagnosis and treatment team that includes oncologists, radiation therapists, pathologists, radiologists, hematologists, and basic scientists. The inpatient unit has 73 beds for acute medical and surgical care.
There are 3 state‐of‐the‐art operating rooms, a 6 bed recovery area, and an 8 bed Intensive Care Unit on the 3rd floor of the patient care center. Over 1,800 cases are performed in the operating room complex each year. A dedicated pediatric surgical nursing staff and 11 pediatric anesthesiologists staff the operating room complex. Children referred to St. Jude receive complete diagnostic testing and are assured that all of the necessary biological studies are performed to properly diagnose and manage childhood tumors. More information is available at www.stjude.org.
Training site #3: Sheldon B. Korones Newborn Center at Regional One Health, Memphis, TN United States
Number of beds: 65 (NICU)
Percentage at this hospital: 4.2%
Training site type: Free standing children's hospital
The Newborn Center is a 65 bed level III NICU with about 1350 admissions a year and over 3000 deliveries. A significant number of high risk neonates are delivered at Regional One as this is the regional referral center for West Tennessee. The NICU is staffed by attending neonatologists, fellows, Pediatric/Med‐Peds residents and NNPs. Over 100 staff RNs and 12 respiratory therapists cover the inpatient services. The center is also supported by social workers, nutritionists, pharmacists, speech and occupational therapists and research nurses. Our NICU rotation allows our fellows to participate in high risk deliveries, resuscitation, stabilization, and management of premature and complex neonates. The collaborative work of our maternal fetal medicine specialists and pediatric subspecialists through the Le Bonheur Fetal Center allows our fellows to participate in prenatal evaluation and management.
Faculty Information
Program Director: Ying Weatherall, MD
Associate Program Director: Tim Jancelewicz, MD, MA, MS
Program manager: Shannae Staten
sstaten@uthsc.edu
901-287-6300
Faculty:
James W. Eubanks, III, MD
Professor of Surgery and Pediatrics
University of Tennessee Health Science Center
Chief, Division of Pediatric Surgery
Surgeon in Chief, Le Bonheur Children’s Hospital
Alexander Feliz, MD
Associate Professor of Surgery and Pediatrics
Program Director, General Surgery Residency
University of Tennessee Health Science Center
Program Director, Pediatric Surgical Critical Care Fellowship
Director, Center for Health Equity
Le Bonheur Children’s Hospital
Tim Jancelewicz, MD, MA, MS
Associate Professor of Surgery and Pediatrics
Associate Program Director, Pediatric Surgery Fellowship
University of Tennessee Health Science Center
Surgical Director, ECMO and CDH
Pediatric Surgical Director, Fetal Center
Le Bonheur Children’s Hospital
Rachel Landisch, MD
Associate Professor, Department of Surgery and Pediatrics
University of Tennessee Health Science Center
Le Bonheur Children’s Hospital
Ying Z. Weatherall, MD
Associate Professor of Surgery and Pediatrics
Program Director, Pediatric Surgery Fellowship
University of Tennessee Health Science Center
Director, Adolescent Bariatric Surgery Program
Surgical Director, Healthy Lifestyle Clinic
Director, Burn Task Force
Le Bonheur Children’s Hospital
Regan Williams, MD, MS
Associate Professor of Surgery and Pediatrics
Associate Program Director, General Surgery Residency
University of Tennessee Health Science Center
Director, Trauma Services
Le Bonheur Children’s Hospital
Fellow Information
Number of fellows: one per year
Current fellow(s):
Akshita ‘Jade’ Kumar, MD
Brian Hosfield, MD
Previous 5 fellows:
Cory McLaughlin, MD
August 2021-July 2023
Assistant Professor, Pediatric Surgery
Children’s Hospital Colorado, Colorado Springs
Sara Mansfield, MD
Aug 2020-July 2022
Pediatric Surgeon, Nationwide Children’s Hospital
Columbus, OH
Daniel Lodwick, MD
Aug 2019-July 2021
Pediatric Surgeon, Department of Pediatric Surgery, Cook Children’s Medical Center
Fort Worth, TX
Erica Hodgeman, MD
Aug 2018-July 2020
Assistant Director, Pediatric Burn Program, Assistant Professor of Surgery, Johns Hopkins Children’s Center
Baltimore, MD
Alpin Malkan, MD
Aug 2017‐July 2019
Pediatric Surgeon, Children’s Hospital of Saint Francis
Tulsa, OK
Donald Lucas, Jr., MD, MPH
Aug 2016‐July 2018
Chief, Division of Pediatric Surgery, Department of General Surgery, Naval Medical Center San Diego; Assistant Professor of Surgery, Uniformed Services University of the Health Sciences
San Diego, CA
Curriculum Information
Block Schedule
Click Here
Call Schedule
1st year: home call, approximately Q3
2nd year: home call, approximately Q3
Conference Schedule
Click Here
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Fellows are provided funds to attend the following:
- Transition to Fellowship Bootcamp
- APSA meeting
- AAP meeting
- MIS course
- Colorectal Course
- Jude Oncology course
- Any additional meetings if fellow is presenting their own work
*Time away subject to ACGME RRC and ABS regulations governing time required in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1254.2 cases
Board passage rate (3 years):
Qualifying exam – 100%; Certifying exam – 67% first time
Fellow salary: PGY-6: $67,980: PGY-7: $70,464
Loma Linda University Children’s Hospital
Last updated: 10/22/2022
Program website: https://lluh.org/health-professionals/gme/resident-fellow/pediatric-surgery-fellowship
The program is designed for well-rounded individuals able to function independently and interested in whole patient and family care.
Strengths
- Our one-Fellow program gives immediate exposure to index cases and a two-year supervised experience of primary management of all ages of pediatric surgery patients
Weaknesses
- Working to improve access to ENT and Urology cases
Institution Information
Loma Linda University Children’s Hospital
Loma Linda, CA United States
Number of beds: 254
Percentage of time at this location: 100%
Training site type: Children's hospital within adult hospital
- 15,574 Admissions
- 6,876 Operations
- 84 bed Level IV NICU
- 25 bed PICU
- 16 bed CTICU
Loma Linda University Children's Hospital is scheduled to become a free-standing children's hospital in 2020-2021.
Faculty Information
Program Director: Edward Tagge, MD
Associate Program Director:
Program manager: Tinesha Charles
909-558-4619
tcharles@llu.edu
Faculty:
Donald Moores, MD – Chief of Pediatric Surgery
Edward Tagge, MD – Professor of Surgery
Faraz Khan, MD – Assistant Professor of Surgery
Andrei Radulescu, MD – Assistant Professor of Surgery
Ali Mejjadam, MD
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Steven Raymond, MD
Previous 5 fellows:
Shannon Longshore, MD – 2013 Assistant Professor of Surgery
Erin Perrone, MD – 2015 Assistant Professor of Surgery
Arul Thirumoothi, MD – 2017 Assistant Professor of Surgery
Victoria Pepper, MD – 2019 Assistant Professor of Surgery
Laura Goodman, MD – 2021
Curriculum Information
Call Schedule
1st Year - home call
2nd Year - home call
General Surgery Morbidity and Mortality Conference
Journal Club (1st Thursday)
Pathology conference/case presentation (alternate) (2nd Thursday)
Resident lectures (3rd Thursday)
Pediatric surgery morbidity and mortality conference (4th Thursday)
Core Lecture (every Thursday)
Radiology conference (every Thursday)
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Our program pays for the following:
- Nationwide Colorectal Course
- Fellow Yr 1 APSA
- Fellow Yr 2 AAP
- St. Jude Oncology course
- Conference if fellow is presenting own work
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): Qualifying exam – 100% (4 out of 4); Certifying exam – 67% first time (3 out of 4) & 100% second time (3 out 4)
Fellow salary: PGY6: $71,893 PGY7: $77,165
Mayo Clinic Arizona/Phoenix Children’s Hospital Pediatric Surgery Fellowship - Mayo Clinic Arizona/Phoenix Children’s Hospital
Last updated: October 2023
Program website: http://phoenixchildrens.org/graduate-medical-education/fellowship-programs/pediatric-surgery-fellowship
The Pediatric Surgery Fellowship is a robust training program for individuals interested in pursuing a career in pediatric surgery. The fellowship is supported by the graduate medical education infrastructure at both the Mayo Clinic in Arizona (program sponsor) and Phoenix Children's (clinical site). Phoenix Children’s and the Mayo Clinic in Arizona are committed to the medical education of pediatric surgeons, providing an environment of academic enrichment, research and a comprehensive educational experience for clinical pediatric surgery fellowship training. Full-time pediatric surgeons serve as faculty with a diverse background including advanced MIS, trauma/critical care, oncology and neonatal surgery. In addition, the fellowship and faculty actively participate in research within the institution as well as serving as the primary investigator in multi-institutional research projects. Fellows finishing the program will be competitive for any potential employment opportunities that they pursue.
Strengths
- The program has an experienced faculty with nationally recognized expertise.
- The program is fellowship focused with high value assigned to surgical training.
- General Surgery and advanced practice providers afford significant leadership opportunities and strong support to fellows.
- Trauma exposure is limited by the use of a fully-staffed Trauma Service.
- In-house General Surgery residents take first calls.
Weaknesses
- Surgery is a very busy service with a high census and case volume and a large faculty.
- Call is q2 from home (and in-house moonlighting is available).
Institution Information
Training Site #1:
Phoenix Children’s
1919 E. Thomas Road
Phoenix, Arizona 85016
Number of beds: 433
Percentage of time at this location: 95%
Training site type: Free standing children's hospital
With a medical staff of nearly 1,000 specialists, Phoenix Children’s is one of the largest pediatric healthcare systems in the country, and the most comprehensive children's care facility in the state. The hospital provides inpatient, outpatient, trauma and emergency care across more than 75 subspecialties. Last year the hospital had more than 13,000 discharges and more than 23,000 surgical cases.
St. Joseph’s Hospital and Medical Center
Phoenix, AZ United States
Number of beds: 595
Percentage of time at this location: 5%
Training site type: Children's hospital within adult hospital
St. Joseph’s Hospital and Medical Center, which is located less than three miles away from Phoenix Children’s Hospital, is a nationally recognized center for quality tertiary care, medical education and research. It includes the internationally renowned Barrow Neurological Institute, the Norton Thoracic Institute, Center for Women's Health, University of Arizona Cancer Center at St. Joseph’s, and a Level I Trauma Center verified by the American College of Surgeons. The hospital is also a respected center for orthopedics, internal medicine, primary care and many other medical services.
Training Site #2
Name and Location:
St. Joseph’s Hospital and Medical Center
350 W. Thomas Road
Phoenix, Arizona 85013
Number of Beds: 595
Percentage of Time at this Location: 5%
Training Site Type: Adult Hospital
St. Joseph’s Hospital and Medical Center, which is located less than three miles away from Phoenix Children’s Hospital, is a nationally recognized center for quality tertiary care, medical education and research. It includes the internationally renowned Barrow Neurological Institute, the Norton Thoracic Institute, Center for Women's Health, University of Arizona Cancer Center at St. Joseph’s, and a Level I Trauma Center verified by the American College of Surgeons. The hospital is also a respected center for orthopedics, internal medicine, primary care and many other medical services.
Faculty Information
Program Director: David M. Notrica, MD
Associate Program Director: Mark S. Molitor, Jr, MD
Program manager:
Amy Bailey
abailey4@phoenixchildrens.com
(602) 933-7209
Faculty:
Bae, Jae-O, MD
Egan, J Craig, MD
Garvey, Erin M, MD
Hansen, Eric, MD
Harris, Jamie C, MD
Jamshidi, Ramin, MD
Lee, Justin, MD
McMahon, Lisa E, MD
Molitor, Mark S, MD
Notrica, David M, MD
Ostlie, Daniel J, MD
Padilla, Benjamin, MD
Rowe, Dorothy H, MD
van Leeuwen, Kathleen D, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Anthony Ferrantella, MD
James Prieto, MD
Previous 5 fellows:
2023 Zens, Tiffany MD , Clinical Instructor, University of Michigan General Surgery, Ann Arbor, Michigan
2022 Velazco, Cristine, MD, Surgeon, Orlando Health Arnold Palmer Hospital—Pediatric Surgery, Orlando, Florida
2021 Gurria Juarez, Juan, MD, Surgeon, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio
2020 Schall, Kathy, MD, Surgeon, Boys Town National Research Hospital, Omaha, Nebraska
2019 Alhajjat, Amir, MD, Surgeon, Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, Illinois
Curriculum Information
Block schedule (enter text or provide document to APSA)
| Fellow | Block 1 | Block 2 | Block 3 | Block 4 | Block 5 | Block 6 | Block 7 | Block 8 | Block 9 | Block 10 | Block 11 | Block 12 |
| Year | Aug | Sep | Oct | Nov | Dec | Jan | Feb | Mar | Apr | May | Jun | Jul |
| 2 | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg |
| 1 | Ped Surg | NICU | Ped Surg | PICU | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Ped Surg | Uro | Ped Surg | Ped Surg |
| Pedsurg |
Call Schedule
Fellows are on service Monday through Friday and alternate on the weekends. Fellows only take call from home.
Conference Schedule
Every Tuesday morning
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The program pays for Transition to Fellowship Boot Camp, Advanced Pectus course, MIS course, Colorectal course, and APSA meeting.
Financial support for candidate interviews: None
Average total number of cases performed by graduating fellows over the past 5 years: 833
Board passage rate (3 years): 75%
Fellow salary:
PL-6 $79,216
PL-7 $83,238
PL-8 $87,125
McMaster Children’s Hospital Pediatric Surgery Fellowship - McMaster Children’s Hospital
Last updated: September 2023
Program website: https://surgery.mcmaster.ca/divisions/pediatric-surgery
The Division of Pediatric Surgery at McMaster Children's Hospital is committed to quality patient care, education and research. As a group of 5 active clinical pediatric surgeons, we are dedicated to supporting and mentoring our fellows to achieve their professional goals. The program will provide the clinical exposure required to be competent in the evaluation and management of the full breadth of neonatal and pediatric general surgical conditions in accordance with the objectives of training outlined by the Royal College of Physicians and Surgeons of Canada.
We seek candidates who are passionate about their career in pediatric surgery and dedicated to the pursuit of developing knowledge and skills in this domain. Trainees in the McMaster program benefit from a dedicated academic half-day with organized teaching seminars and quarterly evaluations.
Strengths
- Rich and diversified case volumes
- Strong program and career support
- Transition to practice program offered in last six months of training
- Research infrastructure and support available for trainees to achieve academic success
- Global health initiative available to pediatric surgery residents for education and research
- Flexible program that meets Training requirements and individual career objectives
Weaknesses
- Non-ECLS centre
- Penetrating trauma volume low
Institution Information
McMaster Children’s Hospital at Hamilton Health Sciences
Hamilton, ON Canada
Number of beds: 165
Percentage of time at this location: 100%
Training site type: Free Standing Women and Children’s Hospital
McMaster Children’s Hospital sees 210,000 visits per year, with 11, 363 admissions. It houses the largest neonatal intensive care unit in Canada and has its own dedicated surgical ward as well as a level 1 pediatric trauma center. It is the second largest children’s hospital in Ontario, Canada. Excluding the NICU and PICU consults, the surgery service averages 1,552 admissions per year and 52,000 emergency department visits. The average case logs for our graduating fellows is 1100 cases (this number has changes over the COVID pandemic but has still exceeded 800).
Faculty Information
Program Director: Lisa VanHouwelingen, MD, MPH, FRCSC
Associate Program Director:
Program manager: Carol Dow
cdow@mcmaster.ca
Faculty:
Karen Bailey, MD, MHM, FRCSC
Peter Fitzgerald, MD, MA, FRCSC
Helene Flageole, MD, MSc, FRCSC, FACS
Michael Livingston, MD, MSc, FRCSC
Lisa VanHouwelingen, MD, MPH, FRCSC
Mark Walton, MD, FRCSC
Fellow Information
Number of fellows: One every year
At McMaster we have an Ontario Ministry of Health funded fellowship position every other year. Both fellows are taught the same curriculum and with the same expectations. This program is a two-fellow program.
Current fellow(s):
Fahd Alsaleh (2021-2024)
Nadia Safa (2023-2024)
Hanan Alansari (2023-2026)
Previous 5 fellows:
Dr. Nathalie Carey July 2021 - June 2023 McMaster University
Dr. Luai Jamal July 2020 - June 2022 Consultant Pediatric Surgeon, Assistant Professor of Surgery, King Abdulaziz University Hospital, Jeddah, KSA
Dr. Gilgamesh Eamer July 2019- June 2021 Assistant Professor Children’s Hospital Ottawa
Dr. Noora Al-Shahwani July 2018- June2020 Assistant Professor Weill Cornell Medicine - Qatar
Dr. Michael Livingston July 2017- June 2019 Assistant Professor McMaster Children’s Hospital
Curriculum Information
Block schedule:
1st Year: 10 months of Pediatric General Surgery, 1 month of NICU, 1 month of PICU
2nd year: 6 months Core Pediatric General Surgery, 6 Months of Transition to Practice
Call schedule:
1st Year – Q4
2nd Year – Q4
- Wherever Possible call will be home call. However, given increasing shortages of human resources, there are times when call may be in house and less than Q4.
Conference Schedule:
1st Year: Fellowship boot camp, APSA or CAPS, Colorectal Course, PALS
2nd year: MIS course (when offered), Oncology, APSA or CAPS
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Fellowship program provides 3000$ yearly to the fellows to help compensate for costs associated with courses (PALS/TRIK), educational conferences (fellowship boot camp, MIS course, oncology) and meetings (APSA, CAPS).
Financial support for candidate interviews: No
What is the average total number of cases performed by your graduating fellows over the past five years? 1000
Board passage rate (10 years): 100%
Fellow salary: https://myparo.ca/your-contract/
PGY 6 – 88, 452.95$
PGY 7 – 91, 848.99$
PGY 8 – 96,908.04$
Please note that this fellowship position is compensated by the Ontario Ministry of Health financially supporting all landed immigrants and Canadian citizens. All non-Canadian citizen’s wishing to participate in our fellowship program will need to provide their own external funding.
Medical College of Wisconsin and Affiliated Hospitals
Last updated: September 2023
Program website: https://www.mcw.edu/departments/surgery/education/fellowship-programs/pediatric-surgery-fellowship
The Pediatric Surgery Fellowship of The Medical College of Wisconsin at the freestanding Children’s Hospital of Wisconsin is a two-year clinical training program approved in 2002 by the ACGME. It was last reviewed in August, 2012 with ACGME continued accreditation through 2023. The curriculum includes comprehensive coverage of the scientific principles that are the basis for the practice of pediatric surgery. These are combined with structured operative and perioperative management of infants, children, and adolescents with problems managed in the contemporary practice of general and thoracic pediatric surgery. The clinical experience encompasses newborns, congenital anomalies, pediatric trauma, burns, critical care, surgical oncology, GI diseases, and the entire spectrum of abdominal, non-cardiac thoracic, urologic, and other clinical problems that fall within the scope of practice for pediatric surgery in the United States.
Institution Information
Children's Hospital of Wisconsin
Milwaukee, WI United States
Number of beds: 298
Percentage of time at this location: 100%
Training site type: Free standing children's hospital
Faculty Information
Program Director: Casey M. Calkins, MD
Associate Program Director: Dave R. Lal, MD
Program manager: Teresa Hauser
thauser@childrenswi.org
414-266-6557
Faculty:
John Aiken, MD
Casey Calkins, MD
Brian Craig, MD
John Densmore, MD
Katy Flynn-O’Brien, MD, MPH
David Gourlay, MD
Dave Lal, MD, MPH
Caroline Maloney, MD, PhD
Jose Salazar Osuna, MD, PhD
Jack Schneider, MD
Amy Wagner, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Senior – Alexander Peters, MD
Junior – Abby Larson, MD
Previous 5 fellows:
Caroline Maolney, MD
2023
Ali Mejaddam, MD
2022
Jose Salazar Osuna, MD, PhD
2021
Shannon Koehler, MD, PhD
2019
Veronica Sullins, MD
2018
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy:
Weekly educational conferences 2-3 hours/week, support for national meeting attendance and other educational conferences (fellow boot camp, colorectal, oncology, etc). More details on website.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1400
Board passage rate (3 years): 100%
Fellow salary: $75,710
Montreal Children’s Hospital (McGill University)
Last updated: November 2023
Program website: http://www.medicine.mcgill.ca/pediatricsurgery/fellowships_gensurgery.htm
The pediatric surgery training program is based at the Montreal Children's Hospital [MCH] of the McGill University Health Centre. It is a two-year residency training program provided to candidates who have completed their training in general surgery at a Royal College of Surgeons of Canada or ACGME-accredited program. All academic faculty involved in the training program are board-certified pediatric surgeons passionate about surgical education.
The scope of training involves a comprehensive program with exposure to pediatric general and non-cardiac, thoracic surgery (with a particular focus on neonatal and congenital malformation surgery), as well as head and neck, gynecological/genitourinary surgery, trauma, oncologic and colorectal surgery. Patients' ages range from the premature to the older adolescent (<18 years). Successful completion of training allows the candidate to sit for the pediatric surgery examinations of the Royal College of Surgeons and the American Board of Surgery. The training objectives can be found on the Royal College of Surgeons of Canada website. As per Royal College's requirement, the program transitioned to a competency-based model of surgical education using “entrustable professional acts” (EPAs). The first year of training consists of 10 months of pediatric general and thoracic surgery and mandatory rotations in Neonatal Intensive Care Units (NICU) and Pediatric Intensive Care Units (PICU), which are one month each. The second year of training consists of 12 months of clinical pediatric general and thoracic surgery at the chief resident level. Elective rotations in Pediatric Urology (1 month) or Pediatric Surgery at Hôpital Ste-Justine (1 month) can be organized during the second year.
Overview/History of Institution:
The Montreal Children’s Hospital (MCH) was founded in 1903 by Dr. Alexander Mackenzie Forbes as a 10-bed unit primarily treating children with orthopedic issues. The establishment of McGill University affiliation in 1920 led to the vision of training surgeons specialized in the care of children. The hospital moved to Tupper Street in 1956 under the leadership of Dr. David Murphy (1953-1974), its first Surgeon-in-Chief, where it remained for nearly 60 years. Dr. Harvey Beardmore (program director 1974-1981) spearheaded efforts to recognize pediatric surgery as a distinct specialty of the American Board of Surgery. Thus, the MCH became one of the “original 5” pediatric surgery training programs in North America under the directorship of Dr. Herbert Owen (1974-1981). Dr. Frank Guttman (1981-1996) took over both the Division and Program Directorships and was succeeded in this role by Dr. Jean-Martin Laberge in 1996. In 2008, after 14 years of unprecedented growth, the Division and Program Directorships were split into two distinct entities under Dr. Sherif Emil and Dr. Pramod Puligandla, respectively.
On May 24, 2015, the MCH underwent its most significant transformation as it moved from a free-standing children’s hospital to a “hospital within a super-hospital” at the McGill University Health Centre Glen Site on Decarie Boulevard. The Division currently consists of 8 board-certified pediatric surgeons with varying interests and expertise, including pediatric critical care. The Division has many interdisciplinary clinics (e.g. EATEF, CDH, chest wall anomalies) and will launch a colorectal center of excellence (COCOE) in September 2024. In addition, Division members dedicate significant personal and academic time to global surgery and indigenous health. The program also has a close working relationship with the Shriner’s Hospital for Children, located immediately adjacent to the MCH, the only Shriner’s hospital outside of the USA. As of 2023, the MCH has trained 60 surgeons from North America and worldwide.
Institution Information
Montreal Children’s Hospital
Montreal, QC Canada
Number of beds: 156, with 52 NICU and 18 PICU beds
Percentage of time at this location: 100%
Training site type: Free-standing children's hospital
Faculty Information
Program Director: Hussein Wissanji, MD, MPH
Program manager: Alessia Umana, Program Coordinator
alessia.umana@muhc.mcgill.ca
Faculty, Harvey E. Beardmore Division of Pediatric Surgery:
Sherif Emil, MD, CM
Mirella & Lino Saputo Foundation Chair in Pediatric Surgical Education and Patient and Family-Centred Care
Professor of Pediatric Surgery, Surgery, and Pediatrics Associate Chair for Education & Departmental Citizenship Department of Pediatric Surgery
McGill University Faculty of Medicine
Director: Harvey E. Beardmore Division of Pediatric Surgery
The Montreal Children's Hospital
McGill University Health Centre
Jean-Martin Laberge, MD
Professor of Surgery and Paediatric Surgery
Department of Pediatric Surgery
McGill University Faculty of Medicine
Pediatric Surgeon, Harvey E. Beardmore Division of Pediatric Surgery
The Montreal Children's Hospital
McGill University Health Centre
Dan Poenaru, MD, MHPE, PhD
Professor of Surgery and Pediatric Surgery
FRQS Clinical Research Scholar
McGill University Faculty of Medicine
Pediatric Surgeon, Harvey E. Beardmore Division of Pediatric Surgery
The Montreal Children’s Hospital
McGill University Health Centre
Pramod S. Puligandla, MD, MSc
Professor of Pediatric Surgery, Pediatrics and Surgery
McGill University Faculty of Medicine
Department of Pediatric Surgery
Pediatric Surgeon, Harvey E. Beardmore Division of Pediatric Surgery
Pediatric Intensivist, Division of Pediatric Critical Care
The Montreal Children’s Hospital
McGill University Health Centre
Kenneth S. Shaw, MD, CM
Assistant Professor of Surgery and Pediatric Surgery
Medical Director, Pediatric and Adolescent Trauma Program
Department of Pediatric Surgery
McGill University Faculty of Medicine
Pediatric Surgeon, Harvey E. Beardmore Division of Pediatric Surgery
The Montreal Children’s Hospital
McGill University Health Centre
Etienne St-Louis, MD CM, PhD, FRCSC (Start date summer 2024)
Assistant Professor of Pediatric Surgery
Department of Pediatric Surgery
McGill University Faculty of Medicine
Pediatric Surgeon, Harvey E. Beardmore Division of Pediatric Surgery
The Montreal Children’s Hospital
McGill University Health Centre
Maeve O'Neill Trudeau, MD CM, MPH, FRCSC
Assistant Professor of Pediatric Surgery
Department of Pediatric Surgery
McGill University Faculty of Medicine
Pediatric Surgeon, Harvey E. Beardmore Division of Pediatric Surgery
The Montreal Children’s Hospital
McGill University Health Centre
Hussein Wissanji, MD, MPH, FRCSC
Assistant Professor of Surgery and Pediatric Surgery
Program Director, Pediatric Surgery Fellowship
Director, Colorectal Center of Excellence (COCOE)
Department of Pediatric Surgery
McGill University Faculty of Medicine
Pediatric Surgeon, Harvey E. Beardmore Division of Pediatric Surgery
The Montreal Children’s Hospital
McGill University Health Centre
Fellow Information
Number of fellows: one per year
Current fellow(s):
Carolina Pinzon-Guzman, MD, PhD (senior fellow)
Samantha Knight, MD (junior fellow)
Previous five fellows:
Etienne St-Louis, MD, CM, PhD
2023
Current position: Bariatric Surgery subspecialization - Centre Hospitalier de l’Université de Montréal, Quebec, Canada, followed by staff Pediatric Surgeon at Montreal Children’s Hospital, McGill University, Quebec, Canada
Yasmine Yousef, MD, CM, PhD
2022
Current Position: Fetal surgery specialization, Hôpital Necker Enfants malades AP-HP, followed by staff Pediatric Surgeon at Joe Di Maggio Hospital, Hollywood, Florida
Amanda Hall, MD, PhD
2021
Pediatric Surgeon, Assistant Professor – University of Saskatchewan, Saskatoon, SK
Eileen Duggan, MD, MPH
2019
Pediatric Surgeon, Assistant Professor - University of Louisville School of Medicine
Louisville, KY
Hussein Wissanji, MD, MPH
2018
Pediatric Surgeon, Assistant Professor - McGill University, Montreal, Canada
Curriculum Information
Call Schedule
1st Year - home call Q2
Fellows are not called for appendicitis or abdominal pain consults, as these are managed by the staff on call with the junior resident. Fellows will receive calls from the PICU/NICU or significant trauma activations.
2nd Year - home call Q2
Fellows are not called for appendicitis or abdominal pain consults, as these are managed by the staff on call with the junior resident. Fellows will receive calls from the PICU/NICU or significant trauma activations.
Conference Schedule
- Tuesday
- NICU-Surgery Rounds – weekly
- Journal club
- GI/Surgery Rounds – weekly
- Case conference/review of common patients
- Wednesday – Academic Half Day
- Senior Teaching – SCORE (07h00-08h00, 12h00-13h30)
- Surgery-Radiology-Pathology (SRP) – 08h00-09h00
- Resident’s clinic (09h00-12h00)
- PICU Teaching (PM) – open invitation (ECLS wet labs, special topics, inter-disciplinary rounds)
- Thursday
- Departmental M+M grand rounds – every other month
- Trauma rounds – 3rdweek of block
- Pediatric Surgical Grand Rounds – 1stweek
- Tumor Board – weekly
- Friday
- Fetal Diagnosis and Therapy Group (every week)
- NICU-Surgery Rounds – weekly
Special Conferences:
- Northeastern Rounds
- Three times a year with CHEO, HSJ, Quebec, Kingston, +/-London, +/- Toronto
- Guttman Day – June every year
- Bass Rounds
- Eight times a year with Canadian Pediatric Surgery training programs
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Fellows' travel and lodging are covered for most post-graduate courses:
- Transition to Pediatric Surgery Fellowship Course
- MIS course
- Jude Oncology Course
- AAP Resident Retreat
- Colorectal Course
Vacation and time away are recorded and confirmed with “time away” regulations set by the RRC
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past five years: 900
Board passage rate (3 years): 100%
Fellow salary: N/A
Nationwide Children’s Hospital Pediatric Surgery Fellowship - Ohio State University/Nationwide Children's Hospital
Last updated: December 2024
Program web page URL https://www.nationwidechildrens.org/for-medical-professionals/education-and-training/fellowship-programs/pediatric-surgery-fellowship
Overview of Fellowship
The Nationwide Children’s Hospital Pediatric Surgery Fellowship program seeks candidates from a diverse background who are eager to pursue a career in pediatric surgery. The goal of the program is to provide the mentoring and training needed to develop expertise in the diagnostic, operative and perioperative care for children with congenital and acquired anomalies and diseases, be they developmental, inflammatory, neoplastic or traumatic. The scope of the training is broad, with a curriculum that encompasses surgical problems in utero, infancy, childhood, adolescence and young adulthood. The educational component prepares our trainees to function independently as board-certified subspecialists and provide them with skills necessary for delivery of surgical care in the tertiary setting, including team management, continuous performance improvement, application of new technology and participation in research. Upon completion, the fellow will have acquired the knowledge, skills, and an enthusiasm for life-long learning, teaching and practice of the pediatric surgery subspecialty. Candidates choose the NCH program due to the pediatric focus, high clinical volume and diverse faculty. The faculty have varied backgrounds and expertise and are at different stages in their careers.
Strengths
- Large volume of colorectal cases, alternate coverage of esophageal foreign bodies (airway FB by ENT)
- Alternate coverage of emergency GYN cases with pediatric adolescent GYN
- ENT rotation
- Specialist fellows help cover cases and calls, strong program support for career development of all trainees
Weakness
- Fellows not involved with transplant cases, (however, fellows responsible for all non-transplant HPB cases)
Institution Information
Training site #1:
Name Nationwide Children’s Hospital
Columbus, OH United States
#beds 673
Percentage of time at this location: 100%
Brief description of other hospital information Named to the Top 10 Honor Roll on U.S. News & World Report’s 2023-24 list of “Best Children’s Hospitals,” Nationwide Children’s Hospital is one of America’s largest not-for-profit freestanding pediatric health care systems providing wellness, preventive, diagnostic, treatment and rehabilitative care for infants, children and adolescents, as well as adult patients with congenital disease. Nationwide Children’s has a staff of more than 13,000 providing state-of-the-art pediatric care during more than 1.6 million patient visits annually. As home to the Department of Pediatrics of The Ohio State University College of Medicine, Nationwide Children’s physicians train the next generation of pediatricians and pediatric specialists. The Abigail Wexner Research Institute at Nationwide Children’s Hospital is one of the Top 10 National Institutes of Health-funded freestanding pediatric research facilities. More information is available at NationwideChildrens.org.
Faculty Information
Program Director – Benedict C. Nwomeh, MD, MPH
Assistant Program Director (if applicable) – Karen A. Diefenbach, MD and Ihab Halaweish, MD
Program manager and email – Mindy Osborne – mindy.osborne@nationwidechildrens.org
List of Faculty and titles
Benedict C. Nwomeh, MD, MPH
Brian D. Kenney, MD, MPH
Christopher K. Breuer, MD
Cory N. Criss, MD
Dana Schwartz, MD
Gail E. Besner, MD
Ihab Halaweish, MD
Jaimie Nathan, MD
James Geiger, MD
Jennifer H. Aldrink, MD
Karen A. Diefenbach, MD
Kyle Van Arendonk, MD
Marc P. Michalsky, MD
Marcus Jarboe, MD
Matthew Ralls, MD
Oluyinka O Olutoye, MD, PhD
Rajan K. Thakkar, MD
Renata B. Fabia, MD
Richard J. Wood, MD
Sara Mansfield, MD
Sara K. Rasmussen, MD
Steven Bruch, MD
Fellow Information
Number of fellows: One per year
Current fellow(s) names:
Steven Scoville, MD
Jack Vernamonti, MD
List of previous 5 fellows: name, grad year, current position
Liese Pruitt, MD; July 2023 – Colorectal Fellow/Faculty, Nemours Children’s
Joseph Drews, MD; July 2022 – Faculty, WV University
Jamie Golden, MD; July 2021 – Faculty, King’s Daughters
Dani Gonzalez, MD; July 2020 – Faculty, Dell Children’s
Afif Kulaylat, MD; July 2019 – Faculty, Penn State Children’s
Program Information
RRC accreditation status: Continued Accreditation
Continued Accreditation: Yes
Meeting/Training Course policy Pays for Transition to Fellowship bootcamp, general surgery board prep, St. Jude course, MIS course, Colorectal course, APSA meeting, AAP meeting plus any additional meetings if fellow presenting own work. Time away subject to RRC regulations governing time in training.
Does the program provide financial support for candidate interviews? Yes
Optional information
What is the average total number of cases performed by your graduating fellows over the past five years?
1300
Board Passage rate (last ten years) 100%
Fellow Salary
PGY-8 = $85,717.69; PGY-9 = $89,963.73; PGY-10 = $93,566.40
NewYork-Presbyterian Pediatric Surgery Fellowship Program(Columbia Campus) - NewYork-Presbyterian/Columbia
Last updated: December 2024
Program website: https://columbiasurgery.org/education-training/pediatric-surgery-fellowship
The NewYork-Presbyterian/Columbia Pediatric Surgery Fellowship Program is a two-year program designed to provide a broad intensive education in all aspects of pediatric general surgery. The education is focused on, but not limited to, pediatric surgical oncology, congenital and acquired conditions of the newborn, non-cardiac thoracic surgery, and all aspects of pre- and post-operative care of infants and children. Multidisciplinary programs in Trauma, ECMO, Congenital Diaphragmatic Hernia, Oncology, Thyroid disease, Obesity and Esophageal Atresia provide focused education in these areas. The integrated program in prenatal pediatrics provides the fellow exposure to diagnosis, treatment, and counseling of the fetal patient/family as well. The goal of our training program is to graduate surgeons who can independently evaluate and treat the full scope of pediatric surgical diseases, manage the consequences of treatment, and know when to seek appropriate consultation and advice.
Institution Information
NYP Morgan Stanley Children’s Hospital
New York, NY United States
Number of beds: 284
Percentage of time at this location: 90%
Training site type: Free standing children's hospital
Memorial Sloan Kettering Cancer Center
New York, NY United States
Percentage of time at this location: 5%
Training site type: Children's hospital within adult hospital
Faculty Information
Program Director: William Middlesworth, MD, Professor of Surgery
Associate Program Director: Erica Fallon MD,
Program manager: Yesenia Suarez
ys466@cumc.columbia.edu
212-342-8585
Fax: 212-342-2138
Melissa Molina
Pediatric Surgery NewYork Presbyterian (Columbia Campus)
Phone number: 212-342-8585
Fax Number: 212-342-2138
Faculty:
Jennifer DeFazio, MD: Assistant Professor of Surgery
Vincent Duron, MD: Assistant Professor of Surgery
Erica Fallon, MD: Assistant Professor of Surgery
Jeffrey Zitsman, MD: Professor of Surgery
Fellow Information
Number of fellows: other
Current fellow(s):
Roxanne Massoumi, MD
Claire Gerall, MD
Previous 5 fellows:
Matthew S Alexander
2023
Pediatric Surgeon Unity Point Health
Meredith A Baker
2022
Pediatric Surgeon at MaineHealth
Sandra K Kabagambe
2021
Assistant Professor Pediatric Surgery at UVA Health
Cornelia Griggs
2020
Pediatric Surgeon at Massachusetts General Hospital
Jennifer Defazio, MD
2019
Assistant Professor in Surgery NewYork-Presbyterian Columbia University Irving Medical Center
Curriculum Information
Block Schedule
PGY6
| Block | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| Site | Site 1 | Site 1 | Site 2 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 |
| Rotation Name | GPS | GPS | MSKCC | GPS | GPS | GPS | GPS | GPS | GPS | PICU | NICU | GPS |
| %Outpatient | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 0% | 0% | 10% |
| %Research | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% |
PGY7
| Block | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| Site | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 | Site 1 |
| Rotation Name | GPS | GPS | GPS | Urology | GPS | GPS | GPS | GPS | GPS | GPS | GPS | GPS |
| %Outpatient | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% |
| %Research | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% |
(GPS) General Pediatric Surgery (both in-patient and outpatient Fellows manage a weekly clinic as part of their curriculum) Site 1
(MSKCC) Pediatric Surgical Oncology (both in-patient and outpatient) Site 2
(Urology) Pediatric Urology (both in-patient and outpatient) Site 1
(NICU) NICU (Nutritional Management/ Ventilator Management) Site 1
(PICU) PICU (Nutritional Management/ Ventilator Management) Site 1
NOTE: Vacation is coordinated amongst the 2 Pediatric Surgery Fellows based on coverage. Pediatric Surgery Fellows are allowed 4weeks every academic year.
Call Schedule
1st Year – home call only
2nd Year – home call only
Conference Schedule
Weekly: Chairman's Conference, Radiology, Morbidity and Mortality, Pediatric Solid Tumor Conference, Journal club/Resident topic Presentations
Monthly/Quarterly: Pathology, Trauma Simulation, Surgical Skills simulation, Joint Neonatlogy/Surgery Conference
Full academic year conference schedule example below.
| SCORE topics | TOPIC | TOPIC | |
| 6-Jul | Aerodigestive tract foreign bodies | 4-Jan | Morbid obesity |
| 13-Jul | Gastroesophageal reflux/antireflux procedure | 11-Jan | FELLOW INTERVIEWS |
| 20-Jul | Branchial cleft anomaly | 18-Jan | Ovarian torsion, cysts and tumors |
| 27-Jul | Congenital diaphragmatic hernia | 25-Jan | Intestinal Failure |
| 3-Aug | Hepatic infections:Hepatitis,abscess,cysts | 1-Feb | FELLOW INTERVIEWS |
| 10-Aug | Anorectal malformations | 8-Feb | Pneumothorax |
| 17-Aug | ECMO/Tumor Board | 15-Feb | FELLOW INTERVIEWS |
| 24-Aug | Lunch | 22-Feb | ECMO Fellows Keystone Talks |
| 31-Aug | Bronchoscopy | ||
| 1-Mar | TRAUMA: Cspine w NS | ||
| 7-Sep | TRAUMA | 8-Mar | FELLOW INTERVIEWS |
| 14-Sep | Cystic diseases of the Lung | 15-Mar | Rhabdomyosarcoma |
| 21-Sep | Malignant liver tumors * | 22-Mar | TRAUMA: Burn/Inhalation Injury* |
| 28-Sep | Peritoneal Dialysis and its complications | 29-Mar | Keith Oldham visiting professor |
| 5-Oct | Empyema # | 5-Apr | Undescended testicle # |
| 12-Oct | Esophageal atresia/TEF | 12-Apr | Thyroid nodules |
| 19-Oct | Inflammatory bowel disease | 19-Apr | TRAUMA:Penetrating Chest trauma |
| 26-Oct | TRAUMA | 26-Apr | Trauma:Initial assessment,resuscitation |
| 2-Nov | Neuroblastoma | 3-May | APSA |
| 9-Nov | Gastroschisis | 10-May | Thoracic trauma |
| 16-Nov | TRAUMA | 17-May | Duodenal atresia, stenosis, webs |
| 23-Nov | THANKSGIVING | 24-May | Wilms,renal cell ca,hemihypertrophy |
| 30-Nov | w/NICU? | 31-May | TRAUMA: Blunt Abdominal Injury/Panc |
| 7-Dec | Omphalocele | 7-Jun | |
| 14-Dec | Hypertrophic pyloric stenosis * | 14-Jun | |
| 21-Dec | Lung physiology, pathophysiology, ventilators | 21-Jun | Ovary and Adnexa* |
| 28-Dec | Esophagoscopy | 28-Jun |
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Program pays for all required conference and conferences at which the fellow is presenting.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): N/A
Fellow salary: NewYork Presbyterian Hospital Graduate Medical Education Graduate Staff Salary Analysis: Graduate Staff Level 2019-2020; Graduate Staff Level 6: $90,209; Graduate Staff Level 7: $92,925
Nicklaus Children's Hospital Pediatric Surgery Program - Nicklaus Children's Hospital
Last updated: 02/07/2020
The Department of Pediatric Surgery offers a two-year ACGME-Accredited fellowship training program in pediatric surgery to Board Eligible or Certified general surgeons who are looking to gain experience in the surgical care of children. The mission of the program is to provide comprehensive training in an environment that emphasizes diverse clinical experience and excellence. The Department of Pediatric Surgery responds to the surgical needs of a very busy emergency department with 100,000 visits a year. The surgical team is an integral part of the Nicklaus Children's Hospital solid tumor program which is a Children's Oncology Group (COG) affiliate. We serve a busy neonatal intensive care unit and treat a broad spectrum of tertiary cases and a full array of common surgical problems in children ranging from the newborn period to age 21. The training program includes integration of didactic, clinical and operative instruction. Clinical education encompasses both inpatient and outpatient bedside teaching. The Training Program follows the ACGME guidelines for Fellowship in Pediatric Surgery and includes conferences in Radiology, Surgical Pathology, Trauma, Tumor Board, GI, Endocrinology, as well as Vascular Malformations Multidisciplinary Rounds, Core Curriculum, Journal Club and a bi-monthly Mortality and Morbidity Conference. The pediatric surgical fellow has the opportunity to become proficient in a broad range of surgical skills during the training program.
Strengths
- The program provides wide spectrum of complex cases and programmatic opportunities including fetal care, oncology, colorectal, endocrine and vascular malformations/ anomalies.
- Diverse patient population and very active global health office
- Training is concentrated in one site, with the opportunity for national or international electives.
- Strong Faculty Commitment to the program and comprehensive didactics
- Advance minimally invasive approach to neonatal anomalies and one of the busiest pediatric robotic programs in the country
- We have a strong support team composed of ARNPs, PAs and rotating residents from four different general surgery programs.
Weaknesses
- No exposure to Transplant cases
- Lack of basic science research (at this time)
Institution Information
Nicklaus Children’s Hospital
Coral Terrace, FL United States
Number of beds: 309
Percentage of time at this location: 100%
Training site type: Free standing children's hospital
Founded in 1950 by Variety Clubs International, Nicklaus Children's Hospital is South Florida's only licensed specialty hospital exclusively for children, with nearly 800 attending physicians and more than 475 pediatric subspecialists. The 309-bed hospital, known as Miami Children's Hospital from 1983 through 2014, is renowned for excellence in all aspects of pediatric medicine, with many programs routinely ranked among the nation's best by U.S. News & World Report since 2008. The hospital is also home to the largest pediatric teaching program in the southeastern United States and has been designated an American Nurses Credentialing Center (ANCC) Magnet facility, the nursing profession's most prestigious institutional honor. The Nicklaus Children's Hospital network includes more than a dozen outpatient centers extending from Palm Beach County to southern Miami-Dade County, offering a range of pediatric healthcare services, including urgent care, rehabilitation services and subspecialty physician appointments for children of all ages, including up to age 21. More information available at https://www.nicklauschildrens.org/about-us.
Faculty Information
Program Director: Fuad Alkhoury, M.D.
Associate Program Director: Cathy Anne Burnweit, MD
Program manager: Ana Otero, C-TAGME
Ana.otero@nicklaushealth.org
786-624-2891
Faculty:
Leopoldo Malvezzi, MD
Juan L Calisto, MD
Shahab Ahmad Shaffiey, MD, MSc
Fellow Information
Number of fellows: one per year
Current fellow(s):
John Tackett, MD
Randi Lassiter, MD
Previous 5 fellows:
Kyle Glithero, MD
2019
Maimonides Medical Center
Brooklyn, NY
Carmelle Romain, MD
2018
University of Chicago Medical Center/ NorthShore University Health System
Chicago, IL
Lynn Model, MD
2017
Maimonides Medical Center
Brooklyn, NY
Gavin Falk, MD
2016
Kalispell Regional Medical Center
Kalispell, MT
Tara Loux, MD
2015
St Joseph's Children's Hospital
Tampa, FL
Curriculum Information
1st year: alternates between Q2 and Q3
2nd year: alternates between Q2 and Q3
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: no, unless fellows are presenting
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1200
Board passage rate (3 years): 90%
Fellow salary: PGY 6: $75,857.60, PGY 8: $82,409.60, PGY 9: $84,864.00
Oregon Health and Science University
Last updated: December 2024
Program website: https://www.ohsu.edu/school-of-medicine/surgery/pediatric-surgery-fellowship-department-surgery
The Pediatric Surgery Fellowship Program in the OHSU School of Medicine is an ACGME-accredited two-year training program. Our fellows rotate between two primary sites, Doernbecher Children's Hospital and Legacy Emanuel Randall Children's Hospital, which have the only two Level 1 pediatric trauma centers, Level IV NICUs, and Level 1 Children’s Surgery Verification (CSV) centers in Oregon. The pediatric surgery faculty at Doernbecher Children's Hospital and Randall Children's Hospital collaborate both clinically and academically. The two hospitals are five miles apart, which allows the teams at both sites to meet together for weekly clinical/educational meetings. The service encourages progressive responsibility for patient management and offers a diverse experience in clinical pediatric surgery. This broad experience includes exposure to advanced minimally-invasive surgery, chest wall reconstruction, fetal surgery, surgical oncology, ECMO, quality improvement projects, and outcomes research. Fellows typically complete 1,000 – 1,200 cases during their fellowship and exceed all required case minimums. The fellowship training includes mandatory and elective rotations in the NICU, PICU, Anesthesia, Urology, and ENT.
Institution Information
Training Site #1: Doernbecher Children’s Hospital – Portland, Oregon
Number of beds: 154
Percentage of time at this location: 50%
Training site type: Children’s hospital within adult hospital
Doernbecher Children's Hospital is an academic teaching children's hospital associated with Oregon Health & Science University located in Portland, Oregon. Established in 1926, it is the first full-service children's hospital in the Pacific Northwest, and provides full-spectrum pediatric care.
Training Site #2: Legacy Emanuel Hospital
Number of beds: 165
Percentage of time at this location: 50%
Training site type: Children’s hospital within adult hospital
Randall Children's Hospital offers a variety of pediatric services including burns, oncology, dentistry, ENT, emergency medicine, eye care, orthopedics, surgical, a neonatal ICU, audiology, urgent care, sleep disorders, rheumatology, and radiology, amongst other
Faculty Information
Program Director: Mubeen Jafri, MD, FACS, FAAP
Associate Program Director: Constance Lee, MD and Lucas McDuffie, MD
Program manager: Kate Manelis
manelis@ohsu.edu
Faculty:
Kenneth Azarow, MD, FACS, FAAP, Chair of Department of Surgery
Benjamin Carr, MD, Assistant Professor
Elizabeth Fialkowski, MD, FACS, FAAP, Associate Professor
Cynthia Gingalewski, MD, Randall Children’s Hospital Medical Director
Mubeen Jafri, MD, FACS, FAAP, Professor
Sanjay Krishnaswami, MD, FACS, FAAP, Professor and Doernbecher Surgeon-in-Chief
Constance Lee, MD, Assistant Professor
Lucas McDuffie, MD, Assistant Professor
Raphael Sun, MD, FACS, FAAP, Assistant Professor
Andrew Zigman, MD, Affiliate Professor (Kaiser Permanente)
Fellow Information
Number of fellows: one per year
Current fellow(s):
Danny Labuz, MD (2nd year)
Maria Tecos, MD (1st year)
Previous 5 fellows:
Devin Halleran, 2024, Pediatric Surgeon, UPMC Children’s Hospital, Pittsburgh, PA
Mike Arnold, 2023, Pediatric Surgeon, Golisano Children’s Hospital of SW Florida, Fort Meyers, FL
Wesley Barry, 2022, Pediatric Surgeon, Providence, Anchorage, AK
Colin Gause, 2021, Pediatric Surgeon, Providence St Vincent, Portland, OR
Stephanie Polites, 2020, Pediatric Surgeon, Mayo Clinic, Rochester, MN
Curriculum Information
Block Schedule
2023 Block Diagram
Call Schedule
1st year: Q2
2nd year: Q2
Block Schedule
Click here to view the block schedule.
Conference Schedule
Educational Conference Monthly Schedule
Program Information
RRC accreditation status: Continued Accreditation
Initial Accreditation: 6/22/2006
Meeting/Training Course policy: OHSU pays for conference registration, airfare and hotel for three conferences for our senior fellow and for two conferences for our junior fellow.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1266
Board Passage rate (last ten years): 90% passage of QE and 100% CE on first attempt since 2014
Fellow salary: 2025-2026
$94,177 PGY 6
$97,698 PGY 7
Rady/UCSD - The University of California, San Diego, Rady Children’s Hospital
Last updated: 10/02/2024
Program website: https://www.rchsd.org/programs-services/pediatric-surgery/fellowship/
Overview
We seek trainees interested in learning to manage the full spectrum of general pediatric surgical conditions in any practice setting whilst employing their humanity and individuality to enhance our profession.
Strengths
- Large case volume and complexity
- Diverse faculty, 9 faculty members
- Free standing USNWR Top Ten children'shospital with many nationally ranked subspecialties supported by accompanying fellowships offering a wide array of specialty trainee programs.
- Pediatric Surgical critical care fellowship
Institution Information
Rady Children's Hospital
San Diego, CA United States
Number of beds: 524
Percentage of time at this location: 100%
Training site type: Free standing children's hospital
- 90% of pediatric care in San Diego. -99% of complex care.
- Provides care to c >225,000 children yearly.
- Yearly c >20,000 admissions.
- Yearly c 250,000 outpatient visits.
- Yearly c 900 trauma patients.
- Yearly c 100,000 emergency care visits and c 50,000 urgent care visits. (c 400/day)
- Yearly c >20,000 surgeries.
- Yearly c 300 newly diagnosed cancer patients.
- Pediatric Surgery volume: 3500 – 4300 cases/year.
- Genomics Institute has sequenced >1000 patient/family genomes.
Faculty Information
Program Director: Karen Kling, MD, FACS
Associate Program Director: Timothy Fairbanks, MD, FACS
Program manager:
Janelle Lagler
nlagler@rchsd.org email is best
858 966 1700 X224292
Faculty:
Stephen Bickler, MD, DTM - Professor
Timothy Fairbanks, MD, MBA - Associate Professor
Gerry Gollin, MD - Professor
Romeo Ignacio, MD, CPT USN - Professor
Benjamin Keller, MD - Assistant Professor
Karen Kling, MD - Professor
David Lazar, MD - Associate Professor
Hariharan Thangarajah, MD, MS - Associate Professor
Kyle Thompson, MD - Assistant Professor
Fellow Information
Number of fellows: one per year
Current fellow(s):
Keon Young Park, MD phD
Megan Birkhold, MD
Previous 5 fellows:
Tim Tirrell, MD PhD
2024
Assistant Professor, Stanford University
Amanda Harrington, MD Mph
2023
Assistant Professor, Johns Hopkins All Children's Hospital
Shunpei Okochi, MD
2022
Assistant Professor and Director of ECMO and Pediatric Surgical Critical Care
Mount Sinai Hospital Health
Jonathan Halbach, DO LCDR
2021
Chief, Naval Hospital, Edward Herbert School of Medicine, Uniformed Services University
Portsmouth, VA
Benjamin Keller, MD
2020
Assistant Professor and Program Director Pediatric Surgical Critical Care
Rady Children's Hospital University of California, San Diego School of Medicine
Bhargava Mullapudi, MD
2018
Associate Professor and Director of Pediatric Transplantation
University of Missouri-Kansas City School of Medicine.
Katherine Davenport, MD
2015
Associate Professor and Director of Pediatric Trauma
Children's Hospital of The King's Daughters
Curriculum Information
Call Schedule
1st year: q 4 call
2nd year: q 4 call
Conference Schedule
Click here to view the conference schedule.
Program Information
RRC accreditation status: Continued Accreditation
Initial accreditation: 2015
Continued accreditation: Yes
Meeting/Training Course policy: APSA, AAP, boot camp, ECMO course, 2 other courses during the fellowship
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1200-1300
Board passage rate (3 years): 100%
Fellow salary: https://meded.ucsd.edu/index.cfm/gme/house_officer
book funds, meal stipend, housing stipend, fellow offices and call room with computers, clinical workroom embedded in patient care area
Riley Hospital for Children at IU Health/Indiana University School of Medicine
Last updated: September 2023
Program website: https://medicine.iu.edu/departments/surgery/education-programs/fellowship/pediatric-surgery/
It is the Mission of the Riley Hospital for Children/Indiana University School of Medicine, Pediatric Surgery program to:
- Advance the health of children through quality surgical care
- Advance pediatric surgical care through basic science and clinical outcomes research
- Advance delivery of pediatric surgical care through quality education of its trainees
The Aims of the Pediatric Surgery Fellowship Program at Indiana University School of Medicine are to:
- Provide post-graduate, board-eligible general surgeons the training to become competent surgeons in the delivery of specialized, high-quality pediatric surgical care.
- Provide a collegial environment that allows collaborative work with professionals across the disciplines of pediatric medicine, while emphasizing the importance of interprofessional collaboration and teamwork in patient care.
- Provide a supportive learning environment that fosters trainee development of self-directed, lifelong learning
Strengths
- Collegial training environment
- Diverse faculty perspective and surgical technique utilized in training fellows
- High volume center at the only academic training center in the state
- Significant supportive resources, including General and Trauma nurse practitioner support
- Level 1 Trauma center
- ELSO designated Platinum level ECMO center with robust ECMO training for fellows
- Contemporary hospital and operating room technology and facilities
- Diverse educational experience, including frequent multinational teleconferences with peer hospitals in Kenya
- Fetal diagnosis and therapeutic center
- Potential fellow elective rotation in Kenya
- Excellent history of graduates attaining desirable job post-fellowship
- Graduate jobs range from private practice to surgeon scientists and academic centers
Weakness
- Surplus of index cases, leaving some covered by senior residents instead of fellows
Institution Information
Riley Hospital for Children at IU Health
Indianapolis, IN United States
Number of beds: 325
Percentage of time at this location: 100%
Training site type: Free standing children's hospital
Annual Emergency Department Visits >47,000
Annual Hospital Operative Volume >19,000
2018 Division of Pediatric Surgery Volume >3,000
Centers of Care:
- Colorectal/Motility
- Maternal/Fetal Medicine
- Chest Wall
- Intestinal Rehabilitation
- Biliary Atresia
- ECMO Center of Excellence
Faculty Information
Program Director: Brian Gray, MD
Associate Program Director: Alan Ladd, MD MBA
Program manager: Stacy Faletic
(o) 317-944-7611
(f) 317-944-9740
sfaletic@iupui.edu
Faculty:
- Cartland Burns, MD, Children’s Surgical Verification Director
Megan Coughlin, MD
Barrett Cromeens, DO, PhD
Brian Gray, MD, Program Director, ECMO Director
Britney Grayson, MD, PhD, BethanyKids, Kijabe, Kenya
Alan Ladd, MD, Division Chief, Associate Program Director
Matthew Landman, MD, MPH, Trauma Director
Troy Markel, MD, Research Director
Jacob Olson, MD
Frederick Rescorla, MD, Former Division Chief
Fellow Information
Number of fellows: one per year
Current fellow(s):
Sarah Tracy MD
Residency – Beth Israel Deaconess Medical Center
Benjamin Many MD
Residency - Northwestern University
Previous 5 fellows:
Amanda Jensen, MD, MS, 2023 - Transplant Surgery Fellow, Stanford University
Eric Groh, MD, 2022 – Pediatric Surgeon, Pediatric Surgeons of West Michigan, Grand Rapids
Barrett Cromeens, DO, PhD, 2021 – Assistant Professor of Surgery at Indiana University
Lucas McDuffie, MD, 2020 – Assistant Professor, Oregon Health Sciences University
Britney Grayson, MD, PhD, 2019 – Assistant Professor of Surgery at Indiana University; BethanyKids, Kijabe, Kenya
Curriculum Information
Call Schedule
1st Year – In-House Q4
2nd Year - In-House Q4
Conference Schedule
Monday - ECMO M&M or education monthy
Tuesday – Neonatology-Surgery conference monthly, Resident teaching conference weekly
Wednesday – M&M*, Department of Surgery Grand Rounds, and/or invited lecturer* (2 AM hours weekly); tumor board weekly
Thursday – Fellow SCORE conference*, Multi-disciplinary fetal conference, or journal club* (1 AM hour weekly); GI-Surgery-Radiology conference* monthly
Friday – Trauma Multi-disciplinary conference monthly, multinational case conference with 2 partner hospitals in Kenya monthly, operative case review conference* monthly
*fellow led conferences
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Pays for one meeting and one course per year plus any additional meetings if fellow is presenting own work. Time away subject to RRC regulations governing time in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1719
Board passage rate (10 years): 100%
Fellow salary: PGY level salary commensurate with University/School of Medicine Policy
Sidney Kimmel Medical College at Thomas Jefferson University/duPont Hospital for Children
Last updated: 01/12/2022
Program website: https://www.nemours.org/education/gme/fellowships/surgery.html
This fellowship will help you prepare for certification by the American Board of Surgery, and is accredited by the Accreditation Council for Graduate Medical Education (ACGME). The Pediatric Surgery Fellowship aims to:
- Train a well-rounded, empathetic, safe pediatric surgeon who is confident managing all aspects of the surgical care of children.
- Steward our fellow in quality improvement projects and methodology, and provide research opportunities.
- Provide a rigorous didactic curriculum for our fellow utilizing 360 degree feedback.
- Cultivate opportunities for our fellow to educate residents and students.
- Encourage our fellow to collaborate across specialties.
- Develop our fellow’s presentation skills during M&M conferences and multi-disciplinary educational meetings.
The program features the full participation of all nine of the Pediatric Surgery Division’s full-time faculty members. Each of these physicians have unique backgrounds and interests and will contribute greatly to your education. Your training will include a rigorous operating room and outpatient clinic experience, as well as bedside evaluation of children. You will be expected to be the leader of the Pediatric Surgery team and have ample opportunities for teaching rotating residents and medical students. You will also play a role in the organization of formal teaching conferences, which are held weekly. Formal rotations will be spent on Pediatric Urology and Neonatology during the first 12 months, with opportunities to spend time with Pediatric ENT. The last year will be spent entirely on the Pediatric Surgical Service.
The majority of your inpatient consultative time will take place at Nemours/Alfred I. duPont Hospital for Children (AIDHC), a freestanding children’s hospital in Wilmington, DE located on the verdant 300-acre Nemours Estate. The hospital is nationally ranked by U.S. News & World Report in four pediatric specialties, including Pediatric GI Surgery. The Hospital has been expanded in the last decade, and now includes 260 beds and state of the art PICU, level IV NICU, and OR facilities. There are more than 14,000 surgical procedures performed each year in our operating rooms (over 1,500 by the Division of Pediatric General Surgery), and there are 60,000 annual visits to our Emergency Department (ED).
Nemours/Alfed I. duPont Hospital for Children is accredited by the American College of Surgeons as the only Level One Pediatric Trauma Center in Delaware, with nearly 1,000 trauma patient visits per year. AIDHC is in the process of seeking Level 1 American College of Surgeons Children’s Surgery Verification (CSV) status. Additionally, the Advanced Delivery Program (ADP) offers onsite delivery of newborns with a wide spectrum of congenital anomalies who require immediate NICU and pediatric surgical care. We also offer the only regional mobile Extracorporeal Membrane Oxygenation (ECMO) program with the ability to both cannulate at regional hospitals and transport patients on ECMO.
- Program self-reported strengths
-
- Large attending staff with diverse training backgrounds and interests
- Program can adapt to the needs and interests of the current fellow
- Exposure to complex hepatobiliary surgery and liver transplant (optional)
- ECMO experience (we are a high volume ECMO center and the only regional center that performs ECMO transport)
- Intestinal failure program
- Pediatric surgical specialty programs including minimally invasive bariatric surgery, chest wall deformities, and endocrine surgery
- Level IV NICU (only one in state of DE) with high volume and wide range of neonatal surgical disease
- Advanced Delivery Program – onsite delivery program
- Emphasis on exposure to prenatal consultation
- Opportunity for meaningful fellow involvement in QI projects
- Program self-reported weaknesses
-
- Single fellow program (this can be considered a weakness or strength depending on how you look at it)
Institution Information
Nemours / A.I. duPont Hospital for Children
Wilmington, DE United States
Number of beds: 260
Percentage of time at this location: 100%
Training site type: Free standing children's hospital
The Nemours/Alfred I. duPont Hospital for Children is a multispecialty, tertiary care teaching institution located on a 300-acre estate in the scenic Brandywine Valley in Wilmington, Del. Among the hospital’s amenities for all staff are: free parking, park-like setting, gym/fitness center, on-site child care center for children of staff, massage therapy. More information is available at https://www.nemours.org/
Faculty Information
Program Director: Loren Berman, MD, MHS
Associate Program Director: Matthew Boelig, MD
Program manager: Nina Tarabicos-Dowd, BS
Nina.Tarabicos@nemours.org
(302) 651-5159
Faculty:
Loren Berman, MD – PD
Matthew Boelig, MD – APD
Brian Duffy, MD
Stephen Dunn, MD – Chair, Department of Surgery
Erika Lindholm, MD
Charles Paidas, MD – Chief, Division of Pediatric General Surgery
Kirk Reichard, MD
Erin Teeple, MD
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Mubina Isani, MD
Previous 5 fellows:
Allison Linden, MD, MPH (Graduated 2020)
Assistant Professor of Surgery – Emory University School of Medicine
Pediatric Surgeon - Division of Pediatric Surgery
Children’s Healthcare of Atlanta
Atlanta, GA
Michael Phillips, MD (Graduated 2018)
Assistant Professor of Surgery – University of North Carolina School of Medicine
Pediatric Surgeon - Division of Pediatric Surgery
North Carolina Children’s Hospital
Chapel Hill, NC
Erin Teeple, MD (Graduated 2016)
Assistant Professor of Surgery – Sidney Kimmel Medical College, Thomas Jefferson University
Pediatric Surgeon – Division of General Surgery
Nemours/AI duPont Hospital for Children
Wilmington, DE
Curriculum Information
Call schedule:
1st Year - in-house/home and
Q2
Q3
Q4
Other: Fellow takes home call every Tuesday and Wednesday evenings and every other weekend; when on call, Fellow takes calls for new NICU/PICU consults and will respond as appropriate; when on call, Fellow will come in for index type cases and additional cases at his/her discretion
2nd Year - in-house/home and
Q2
Q3
Q4
Other: Fellow takes home call every Tuesday and Wednesday evenings and every other weekend; when on call, Fellow takes calls for new NICU/PICU consults and will respond as appropriate; when on call, Fellow will come in for index type cases and additional cases at his/her discretion
Conference Schedule: Conferences are held every Wednesday AM and include:
- Mock Oral Exams (every other week, two faculty examiners per session)
- Patient Review with NICU and PICU (weekly, led by fellow)
- Core Curriculum Lectures (weekly, delivered by faculty and residents)
- Pediatric Surgery Division Morbidity and Mortality (every other week, led by fellow)
- Monthly Multidisciplinary Conferences (led by fellow): Surgery-Pathology, Surgery-Radiology
- Journal Club (Monthly, led by faculty and fellow)
- Enterprise Wide Interesting Case/Topic Conference - Nemours Delaware, Jacksonville, Orlando (led by faculty)
- Trauma Case and Peer Review (every other week, led by faculty)
Other Conferences for Fellow involvement:
- Weekly Tumor Board
- Weekly Fetal Management Conference
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Pays for Transition to Fellowship boot camp, MIS course, Colorectal course, APSA meeting, AAP meeting plus any additional meetings if fellow presenting own work. Time away subject to RRC regulations governing time in training.
Financial support for candidate interviews: No – all interviews currently conducted remotely via Zoom
Average total number of cases performed by graduating fellows over the past 5 years: 1268
Board passage rate (3 years): Qualifying Exam - 100%; Certifying exam - 67% first pass
Fellow salary: PGY 6 $74,419, PGY 7 $77,078
St. Christopher's Hospital for Children
Last updated: January 2025
Program website: https://towerhealth.org/academic-affairs/pediatric-fellowships/pediatric-surgery-fellowship
The Pediatric Surgery Fellowship Program at St. Christopher’s Hospital for Children encompasses the broad educational curriculum and clinical training required in the field of Pediatric Surgery. The two-year clinical program provides exposure to an expansive variety of surgical procedures in children, including a high volume of neonatal and minimally invasive surgical cases. Our fellow receives extensive experience in the management of complex congenital malformations as well as routine pediatric surgical conditions. These include abdominal/retroperitoneal and non-cardiac thoracic surgical problems, tumors, infections, head and neck masses, endoscopy, and urologic procedures. The program includes a significant exposure in the Neonatal and Pediatric Intensive Care Units (NICU and PICU), with a one-month rotation in each unit. St. Christopher’s is a designated Level I Pediatric Trauma Center and has an active ECMO program. Fellows attend office hours in the surgery clinic in order to master skills and knowledge required to care for outpatients including preoperative evaluation and postoperative care. A unique opportunity to spend some time at the Shriner’s Hospital for Children exists with the ability to learn exposure techniques for spinal surgeries, adds a significant thoracic and diaphragm experience. Fellows lead a team that manages all patients on the Pediatric Surgery Service (including in the NICU, PICU, and medical-surgical units) with supervision by attending surgeons dedicated to mentorship and evidence-based optimal care. Scholarly activity and education are highly valued, with a broad curriculum covering the full scope of pediatric surgery.
Institution Information
Training Site #1:
St. Christopher’s Hospital for Children
Philadelphia, PA United States
Number of beds: 189
Percentage of time at this location: 95%
Training site type: Free standing children’s hospital
Training Site #2:
Shriner’s Hospital for Children, Philadelphia PA
Number of beds: NA
Percentage of time at this location: ~5%
Training site type: Sub-Specialty Children’s Hospital
Opportunity to learn exposure techniques for complex spinal surgeries.
Faculty Information
Program Director: Alana Beres MD
alana.beres@towerhealth.org
Program manager: Kimberly Abrams
kimberly.abrams@towerhealth.org
215-427-8812
Faculty:
Alana Beres MD- Fellowship Program Director, Interim Division Chief,
Director of Resident and Medical Student Education, Surgical Director of Regional Fetal Evaluation Center, Research fellowship director
Sean Ciullo MD- Trauma Medical Director
Alexander Chalphin MD- ECMO director, associate program director
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Cressida Mahung (Howard University)- clinical fellow
Carly Chappell- Research fellow
Previous 5 fellows:
Michael LaQuaglia MD
2024
St. Peter’s Children’s Hospital, NJ
Christopher Pennell MD
2022
Mercy St. Louis MO
Erika B Lindholm, MD
2020
Cooper University Health Care
Camden NJ
Teerin Meckmongkol, MD, PhD
2018
Nemours Children’s Hospital
Orlando, FL
Sean Ciullo, MD
2017
St. Christopher’s Hospital for Children
Curriculum Information
Call Schedule
1st year: Q4/Q5 in house
2nd year: Q4/Q5 in house
Conference Schedule
Weekly Thursday 8 am -11 am. M&M/Journal Club/SRP(8-9), SCORE (9-10), mock orals 10-11)
Quarterly NICU/Surgery conference
Monthly GI/Surgery conference
Monthly Tumor Board
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Colorectal course, Oncology course (or Pectus course), APSA in first year, AAP in second year
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1137
Board passage rate (3 years): 100% over last 10 years
Fellow salary:
PGY-6: 74,494$
PGY-7: 76,842$
PGY-8: 79,719$
Stanford University Pediatric General Surgery Fellowship - Stanford University
Last updated: December 2023
Program website: http://pediatricsurgery.stanford.edu/education/PedSurgFellowship.html
The Division of Pediatric General Surgery offers a 2-year, single-fellow ACGME accredited fellowship program. The objectives of Stanford’s postgraduate training in Pediatric Surgery are to develop Pediatric Surgeons who can, with an increasing level of autonomy, assume complete responsibility for the preoperative, operative, and postoperative management of the problems relegated to their area of special expertise and who can interact appropriately with allied colleagues involved in the care of pediatric patients. Additionally, it is expected that the fellow will develop the sensitivity required to deal not only with pediatric patients, but also with their families. Interwoven with these objectives will be those of an ethical and academic nature that will reflect the conscience of modern Pediatric Surgery and that will help advance the field through innovation, research, and discovery.
Strengths
- Broad spectrum of minimal access surgery
- Endoscopic treatment of achalasia
- Accredited bariatric surgery program
- Chest wall deformities
- Surgical oncology
- Inflammatory bowel disease
- Fetal diagnosis counseling and treatment
- Short bowel and intestinal rehabilitation
- Bowel management program
- Level 1 Accredited Trauma Center
Weakness
- Hepatoblastomas go to the transplant team, but our fellow is welcome to scrub in if interested.
- Airway foreign bodies go to ENT, but our fellow is welcome to retrieve them with their team
Institution Information
Lucile Packard Children’s Hospital
Stanford, CA United States
Number of beds: 361
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Stanford Children’s Health, with Lucile Packard Children’s Hospital Stanford at its core, offers comprehensive clinical services, from treatments for rare and complex conditions to primary care. We provide care in more than 150 medical specialties. Our exceptional care extends far beyond the hospital walls. Today, our Stanford physicians and health care teams offer comprehensive clinical services at more than 60 locations. We’ve expanded our clinical programs to regional centers and have brought our specialists and subspecialists inside more than a dozen top hospitals across the western United States—and we have Stanford Children’s Health primary care providers in dozens of locations across the Bay Area. We provide fertility services, normal and complex obstetrical care, multidisciplinary fetal care and perinatal genetics, and neonatology services all in one place. As global leaders in obstetrical and neonatal care, our physician-scientists have advanced their field in the United States for more than half a century. Together, our network offers a full spectrum of premiere pediatric and obstetrical care close to where our patients and their families live. For more information, please visit our website https://www.stanfordchildrens.org/en/default.page
Faculty Information
Program Director: James Dunn, MD, PhD
Associate Program Director:
Program manager and contact info:
Samrawit Gebregziabher
Phone: 650-723-6439
Email: samrawit@stanford.edu
Faculty:
- Stephanie Chao, Assistant Professor of Surgery.
- Bill Chiu, Assistant Professor of Surgery.
- James Dunn, Professor of Surgery, Division Chief.
- Julie Fuchs, Clinical Associate Professor of Surgery.
- Gary Hartman, Clinical Professor of Surgery.
- Jeong Hyun, Assistant Professor of Surgery.
- Thomas Hui, Clinical Associate Professor of Surgery.
- Faraz Khan, Clinical Associate Professor of Surgery.
- Dennis Lund, Professor of Surgery, Chief Medical Officer.
- Claudia Mueller, Associate Professor of Surgery.
- David Powell, Clinical Associate Professor of Surgery.
- Janey Pratt, Clinical Professor of Surgery.
- Wendy Su, Clinical Associate Professor of Surgery.
- Karl Sylvester, Professor of Surgery.
- James Wall, Associate Professor of Surgery.
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Marisa Schwab, MD
Previous 5 fellows:
Aaron Cunningham, MD
2023
Assistant Professor of Surgery
Shawn Jenkins Childrens Hospital
Medical University of South Carolina
Rachel Landisch, MD
2021
Assistant Professor of Surgery
Le Bonheur Children’s Hospital
University of Tennessee Health Science Center, Memphis, TN
Enrico Danzer, MD
2019
Assistant Professor of Surgery
Memorial Sloan Kettering Cancer Center
Weill Cornell Medical College, New York, NY
Chad Thorson, MD
2017
Associate Professor of Surgery
Program Director General Surgery Program
Stephanie Chao, MD
2015
Assistant Professor of Surgery, Stanford University
Stanford, CA
Curriculum Information
Block schedule:
1 month of NICU rotation
1 month of PICU rotation
22 months Pediatric Surgery
Call schedule
1st Year - in-house/home and Q4
Other: every other weekend
2nd Year - in-house/home and Q4
Other: every other weekend
Explain
Conference Schedule
| Conference | Time |
| Surgery Grand Rounds Li Ka Shing |
Tuesdays 7-8 am |
| Tumor Board LPCH Board Room |
Tuesday 8-9 am |
| Core Lecture Series Alway Conference Room |
Monday 7:30-8:30 am |
| Pediatric Surgery Division Meeting Alway Conference Room |
Wednesday 8:40-9:15 am |
| Morbidity/Mortality Review Alway Conference Room |
Wednesdays 9:15-10 am |
| Surgery/GI Case Review Alway Conference Room |
1st Wednesday
7:30-8:30 am |
| Pediatric Surgery Journal Club Alway Conference Room |
2nd Wednesday
7:30-8:30 am |
| Surgery/Pathology/Radiology Case Review Radiology Reading Room |
3rd Wednesday
7:30-8:30 am |
| Surgery/NICU/Radiology Case Review
Radiology Reading Room |
4th Wednesday
7:30 – 8:30 am |
| Multidisciplinary Bariatric Review Board Alway Conference Room |
1st Thursday
12-1 pm |
| Perinatal/NICU Conference LPCH Auditorium |
Fridays 12-1 pm |
| Fetal Case Conference Radiology Conference Rm |
Every Other Friday 7-8 am |
| Pediatric (Trauma) Quality Improvement Meeting Radiology Conference Room |
5th Wednesdays
7:30 – 8:30 am |
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Pays for Pediatric Surgery Transition to Fellowship Courses, general surgery board preparation, MIS course, ECMO course, ATLS course, APSA member registration and conference payments, AAP meetings. Time away abides by ACGME regulations.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (7 years): 100%
Fellow salary: Based on PGY year and fellow receives a housing stipend.
University at Buffalo
Last updated: December 2024
Program Name and location:
University at Buffalo Pediatric Surgery Fellowship
Program website: http://medicine.buffalo.edu/departments/surgery/education/fellowship/pediatric-surgery.html
Overview of Fellowship:
The Pediatric Surgery Fellowship Program offered through the University at Buffalo is an ACGME-accredited two-year program. Our one-fellow program provides a focused experience and opportunity to participate in most cases, including advanced MIS exposure. The fellow is fully immersed in inpatient and outpatient care during the program and is both a team leader and educator from day one.
We seek candidates who a motivated, self-learners who are interested in MIS innovation, able to run a service well as single fellow, and have a big-picture view of pediatric surgical care delivery.
Strengths
- Advanced MIS exposure
- Diverse faculty
- Teaching conferences
- New hospital
- Single-fellow program
- No night call
- Ample APP support
Weaknesses
- Single fellow program
- Lack of depth in hepatibiliary
- Inconsistent PICU/NICU/pediatric specialty support
Institution Information
Training Site #1:
John R. Oishei Children’s Hospital
Buffalo, NY United States
Number of beds: 180
Percentage of time at this location: 95%
Training site type: Free standing children’s hospital
John R. Oishei Children’s Hospital has 45,000 annual ED visits, 20,000 annual cases and is the only free-standing children’s hospital in the area and one of two level 1 pediatric trauma centers in New York State. Multidisciplinary surgery programs include: thyroid tumor board, intestinal rehab, obesity/weight wellness, vascular anomalies, chest wall deformities, and bowel management.
Training Site #2:
Memorial Sloan Kettering Cancer Center
New York, NY United States
Percentage of time at this location: 5%
Training site type: Children’s hospital within adult hospital
Our fellow completes a 1-month pediatric oncology rotation within the first year of the program.
Faculty Information
Program Director: Kaveh Vali, MD
Associate Program Director: Ben Ham, MD
Program manager and contact info:
Sydney Rojek
Training Program Administrator
slrojek@buffalo.edu
Faculty:
Kaveh Vali, MD — Program Director, Clinical Assistant Professor
Ben Ham, MD — Associate Program Director, Assistant Professor
Carroll Mac Harmon, MD, PhD — Chief of Pediatric Surgery and Surgeon in Chief
Andrew Nordin, MD – Clinical Assistant Professor, Trauma Medical Director
Peter Kim, MD- Vice Chair Research and Innovation Department of Surgery Professor of Surgery
Fellow Information
Number of fellows: Once fellow, every other year (Start Dates; Aug 2026, Aug 2028, Aug 2030 etc.)
Current fellow(s):
Hector Osei, MD
Previous 5 fellows:
Maria Chulkov, MD
2024
Pediatric Surgeon, Carilion Roanoke Memorial Hospital
Roanoke, VA
Ruchi Amin, MD
2022
Pediatric Surgeon, Broward Health Coral Springs
Fort Lauderdale, FL
Ben Ham, MD
2020
Faculty, University at Buffalo
Buffalo, NY
Anthony Savo, MD
2018
locum tenens
Ben Tabak, MD
2017
Pediatric Surgeon, Tripler Army Base
Honolulu, Hawaii
Curriculum Information
Block Schedule
The fellow is on the Pediatric Surgery service at Oishei Children’s Hospital for majority of the program, but has the opportunity to complete 1-month rotations in the hospital’s NICU and PICU, as well as a 1-month rotation at Memorial Sloan Kettering Cancer Center for exposure to pediatric oncology cases.
Call Schedule
1st year: no in house call; home call and comes in at discretion of attending *
2nd year: no in house call; home call and comes in at discretion of attending *
*(no direct calls from anybody else)
Conference Schedule Elaborate conference schedule consisting of but not limited to:
tumor board, mock trauma, morbidity and mortality conference, case conference, neosurgery conference, pediatric GI conference, aerodigestive conference, multidisciplinary thyroid conference, journal club, trauma conferences, NSQIP conference, fetal care conference, ED/Peds Surg conference, PICU/Peds Surg conference, skills sessions, surgery/pathology/radiology conference, and pediatric surgery grand rounds
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Program pays for AAP, APSA, Colorectal Course, St Jude Oncology update, Chicago MIS course.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: Around 1500
Board passage rate (3 years): 100%
Fellow salary:PGY-6: $68,192
PGY-7: $68,359
Plus estimated ~$3,000 in benefits each AY
University of Alabama at Birmingham/Children’s of Alabama
Last updated: September 2023
Program website: https://www.uab.edu/medicine/surgery/pediatric/education/pediatric-surgery-fellowship
The University of Alabama at Birmingham Division of Pediatric Surgery at Children’s Hospital of Alabama sponsors an ACGME-accredited Pediatric Surgery Fellowship with one resident admitted yearly for the two-year program. Our program seeks candidates from varied backgrounds with strong surgical skills, eager to develop expertise in pediatric surgery. Our goal is to train pediatric surgeons who will be outstanding and compassionate clinicians capable of independently managing pediatric general surgical patients from infancy to young adulthood. The training program provides a broad exposure to all aspects of pediatric surgery and allows for graded autonomy. The faculty members have diverse backgrounds, are at various stages of their careers, and get along quite well. Candidates choose Children’s of Alabama for the large clinical volume, graded fellow autonomy, NICU coverage, and advanced minimally invasive experience.
Strengths
- Minimally-invasive surgery experience including single-site laparoscopy,
- Primary coverage of NICU patients
- Primary coverage of non-cardiac ECMO service
- Alternate coverage of airway and esophageal foreign bodies
- Coverage of all urgent and emergent GYN cases
- Overseas opportunity
Weaknesses
- Fellows not involved with transplant cases
- Lack of dedicated time for research
Institution Information
Children’s Hospital of Alabama
Birmingham, AL United States
Number of beds: 332 beds plus 48 surgical NICU bassinets
Percentage of time at this location: 96%
Training site type: Free standing children’s hospital
UAB Women’s and Infants Center
Birmingham, AL United States
Number of beds: 120-bed Level IV NICU/CCN
Percentage of time at this location: 4%
Training site type: Children’s hospital within adult hospital
Faculty Information
Program Director: Scott Anderson
Associate Program Director:
Program manager: Diane Rosato
Diane.Rosato@childrensal.org
Faculty:
Mike Chen, MD, MBA
Elizabeth Beierle, MD
Scott Anderson, MD
Robert Russell, MD, MPH
Vincent Mortellaro, MD
Chinwendu Onwubiko, MD, PhD
Eric Sparks, MD
Laura Stafman, MD, PhD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Joseph Esparaz, MD, MPH
Ryan Pickens, MD
Previous 5 fellows:
Adele Williams, MD
2023
Children’s Hospital of New Orleans
New Orleans, LA
Natalie O’Neill
2022
Children’s Hospital of The King’s Daughters
Norfolk, VA
Alicia Waters, MD
2021
St. Joseph’s Children’s Hospital
Tampa, FL
Stewart Carter, MD
2020
Assistant Professor of Surgery, University of Louisville
Norton Children’s Hospital
Louisville, KY
Jerry Chen, MD
2019
The Permanente Medical Group, Roseville Women and Children’s Center
Roseville, CA
Curriculum Information
Call Schedule
1st year: Q4
2nd year: Q4
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Pays for transition to fellowship bootcamp, colorectal course, St. Jude course, APSA meeting, AAP meeting, plus any additional meetings if fellow presenting own work or has specific clinical interest. Time away subject to RRC regulations governing time in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1500
Board passage rate (3 years): 100%
Fellow salary: https://www.uab.edu/medicine/home/residents-fellows/current/resident-physician-salary-benefits
University of California Irvine Program
Last Updated: September 2023
Program Name: University of California Irvine Program
Program Website: https://www.choc.org/careers/residency-training-programs/pediatric-surgery-fellowship/
Description of type of candidate program seeks:
The UCI/CHOC Pediatric Surgery fellowship program is committed to recruiting and training talented individuals whose backgrounds reflect California’s rich diversity. Our goal is to build an inclusive educational framework to produce future pediatric surgeons who will improve the communities which they will serve, while striving for excellence in research, teaching, and service. Our fellowship training program will provide a comprehensive educational experience, producing pediatrics surgeons who are academically, clinically, and professionally prepared to meet the demands of the ever-changing landscape of medicine.
Program self-reported strengths:
The UC Irvine-CHOC Children’s Hospital Pediatric Surgery Fellowship is based at CHOC Children’s Hospital (CHOC). CHOC and UCI function as one entity for care of children in our county. CHOC is a tertiary care freestanding children’s hospital, serving a diverse population based in Orange County, the sixth most populous county in the nation. CHOC and UCI possess faculty who represent a vast array of different subspecialties and areas of interest, cultivating an environment of inquiry with ample opportunities for scholarly activity to satisfy the variety of interests which the fellows will have. The fellows will be given the opportunities to strengthen their skills, knowledge, and confidence in the areas of quality improvement, patient safety, population health, innovation, translational and biomedical research. Faculty are dedicated to the UCI School of Medicine’s mission of “Discover. Teach. Heal.” and will guide the fellows through the infrastructure of our robust research and scholarship environment. There is strong institutional support with provision of administrative assistants, research coordinators and statisticians.
There are 10 pediatric surgeons that serve as the faculty for the fellowship. The CHOC pediatric general and thoracic surgery service also includes 3 Nurse Practitioners (NPs) that cover the service 7 days a week, in addition there are 2 NPs that cover the Trauma Service and 1 NP that covers the Colorectal Program. Two general surgery junior residents also rotate on our service.
CHOC’s main hospital is a 334-bed facility. CHOC has numerous medical and surgical inpatient units as well as an oncology ward. The inpatient pediatric critical care units provide care for both infants and older children, including a level IV neonatology intensive care unit with several subspecialty areas, including a Surgical NICU (total number of NICU beds = 92). The pediatric intensive care unit has 30 beds and the cardiovascular intensive care unit has 12 beds. CHOC’s ECMO program is currently designated as a Platinum Center of Excellence by the Extracorporeal Life Support Organization. Labor and delivery services are present at the adjacent/connected St. Joseph Hospital of Orange with an annual average of 6,000 deliveries. In addition, high risk perinatal deliveries occur at UC Irvine Medical Center and neonates with complex surgical needs are transferred to CHOC. In 2018, CHOC and UCI partnered to improve pre- and peri-natal care to families in Orange County. In 2021, CHOC and UCI opened The Fetal Care Center of Southern California, which provides accurate diagnosis, prenatal counseling and peri-natal planning to optimize outcomes for expectant mothers who are carrying a fetus with a complex congenital anomaly. CHOC and UCI are presently designing a special delivery unit and a fetal surgery suite that is projected to open in 2024. The CHOC Emergency Department is a 22,000 square foot, full-service 24/7 emergency department and an ACS-verified level 2 pediatric trauma center, in the process to be verified as a level 1 in the latter part of 2021.
CHOC currently has nine main operating suites, three minor procedure rooms, a dedicated cardiac surgery operating room, an interventional radiology suite, and a planned expansion to add two more operating rooms. All the main operating rooms are equipped with state-of-the art equipment for minimally invasive surgery. Outpatient pediatric surgery clinics consist of 4 patient exam rooms. The clinic is located on the same campus at CHOC.
Program self-reported weaknesses:
Our program was approved by the ACGME in 2021. Therefore, we are a new program and do not yet have a track record of having our graduates going on to have successful careers. Another self-reported potential drawback may be that our program is a single fellow program. Although this a self-reported weakness, we believe that this provides our trainee the correct amount of autonomy and ability choose cases without having to sacrifice on the educational value.
Institution Information
Training Site #1:
Children’s Hospital of Orange County
Number of beds: 334
Percentage of time at this location: 99%
Training site type: Free standing children’s hospital
Faculty Information
Program Director:
Yigit S. Guner, MD, MS
Associate Clinical Professor of Surgery
UC Irvine School of Medicine
yguner@hs.uci.edu
Associate Program Director:
Peter T. Yu, MD, MPH
Associate Clinical Professor of Surgery
UC Irvine School of Medicine
yup@choc.org
Program manager:
Cesar Plascencia
Cesar.Plascencia@choc.org
Phone: 714-509-8866
Faculty:
Saeed Awan, MD
John German, MD - Emeritus
David Gibbs, MD
Laura Goodman, MD, MPH
Maryam Gholizadeh, MD
Mustafa Kabeer, MD
Troy Reyna, MD
Vinh Lam, MD
Peter Yu, MD
Donald Shaul, MD
Joanne Starr, MD
Heidi Stephanie, MD
Kevin Huoh, MD
Irfan Ahmad, MD
Juliette Hunt, MD
Hira Ahmad, MD
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Amy Lawrence, MD,
Previous 5 fellows:
Yangyang Yu, MD, MS
Program Information
RRC accreditation status: Yes
Meeting/Training Course policy: 1 course per year and 1 meeting per year (APSA or AAP)
Financial support for candidate interviews: N/A
Average total number of cases performed by graduating fellows over the past 5 years: 1133
Board passage rate (3 years): N/A
Fellow salary: 96,334.60
University of California San Francisco Pediatric Surgery Fellowship - UCSF Benioff Children's Hospitals
Last updated: 9/12/2023
Program website: https://pedsurg.ucsf.edu/education-training/pediatric-surgery-fellowship.aspx
This fellowship takes place between the two participating sites – UCSF Benioff Children’s Hospital San Francisco (BCHSF) and UCSF Benioff Children’s Hospital Oakland (BCH Oakland) – with the fellow rotating between campuses on an every three month basis. The two campuses are near each other – just 11.5 miles apart. Attending surgeons at both sites are faculty in the UCSF Department of Surgery and regularly interact via weekly web-based joint clinical meetings. The two hospitals have complementary strengths that are critical to the education of a fellow. Combined, the two institutions have a strong commitment to the underserved with a diverse patient population as well as a diverse mix of cases available to the pediatric surgery trainee.
The faculty at BCHSF have long been leaders in complex areas of pediatric surgery such as neonatal surgery, minimally invasive surgery, fetal care, and surgical oncology. The Division of Pediatric Surgery also has a rich history of scholarship in clinical and translational research as well as basic science research. In clinical research, BCHSF has innovated particularly in the areas of fetal surgery and minimally invasive surgery. Thus, in addition to the rich clinical volume, the pediatric surgery fellow is encouraged to participate in the long-standing tradition of clinical research.
The faculty at BCH Oakland have long been leaders in pediatric trauma care and are busy clinical surgeons with specific interests in chest wall deformities, inflammatory bowel disease, oncology, neonatal surgery, and surgical critical care. BCH Oakland faculty have research interests in trauma and surgical innovation. BCH Oakland is a high-volume full-service freestanding children’s hospital with a broad range of elective and emergency pediatric surgical cases, a Level 4 NICU, an ECMO program, and an oncology program. The Oakland campus is an American College of Surgeons verified Level 1 pediatric trauma center and is one of the busiest pediatric trauma centers in California.
The first year of fellowship will include rotations in the NICU, PICU, Urology and a rotation of the fellow’s choice from those allowed by the ACGME. The second year will concentrate solely on general pediatric surgery.
Strengths
- Large case volume including niche experience with airway and esophageal foreign bodies (BCH Oakland)
- GYN cases (BCH Oakland) and open fetal surgery cases (BCHSF) that are all primarily managed by pediatric surgery faculty.
Weaknesses
- One fellow with two clinical sites – mitigated by a list of index cases that permit the fellow to travel to the alternate site to maximize experience.
- Relatively new fellowship program that incorporates changes to curriculum and experience based on fellow feedback.
Institution Information
Training Site #1:
UCSF Benioff Children’s Hospital San Francisco
San Francisco, CA United States
Number of beds: 183
Percentage of time at this location: 50%
Training site type: Children’s hospital within an adult hospital
UCSF Benioff Children’s Hospital San Francisco is recognized throughout the world as a leader in health care, known for innovation, technology and compassionate care. For more than a century, we have offered the highest quality medical treatment.
UCSF BCHSF is one of the top children’s hospitals in the nation, according to a ranking by U.S. News & World Report. Our expertise covers virtually all pediatric conditions, including cancer, heart disease, neurological disorders, organ transplants and orthopedics as well as the care of critically ill newborns.
Our new, state-of-the-art, 183-bed UCSF Benioff Children’s Hospital San Francisco offers emergency care and specialty outpatient services, including a 50-bed Neonatal Intensive Care Nursery. Our doctors were the first in the world to successfully perform surgery on a baby still in the womb. The Fetal Treatment Center is intricately connected with the UCSF Division of Pediatric Surgery at UCSF Benioff Children’s Hospital which is dedicated to providing expert surgical care for fetuses, infants, children, and adolescents with congenital and acquired conditions. Our pediatric surgeons remain committed to the ongoing development of new surgical techniques for treating diseases in children-particularly minimally invasive approaches to replace more invasive open procedures that require large incisions.
Additional tailored fellow outpatient clinical experiences include the L.I.F.E. (Long-Term Infant-to-Adult Follow-Up and Evaluation Program) clinic for long-term multidisciplinary follow-up care for children surviving and thriving with congenital anomalies, the UCSF Birthmarks and Vascular Anomalies Center for highly specialized multidisciplinary care for all types of vascular birthmarks and anomalies, from the most common to the rare and complex, colorectal anomalies clinic, and chest wall anomalies clinic.
Training Site #2:
UCSF Benioff Children’s Hospital Oakland
Oakland, CA United States
Number of beds: 190
Percentage of time at this location: 50%
Training site type: Free standing children’s hospital
UCSF Benioff Children’s Hospital Oakland has been delivering exceptional medical care to children from all regions of California for nearly 100 years. UCSF BCH Oakland is one of the top children’s hospitals in the nation, according to a ranking by U.S. News & World Report. Our expertise covers virtually all pediatric conditions spanning 30 pediatric medical subspecialties with programs dedicated to oncology, bone marrow transplant, congenital heart disease, complex neonatal care, ECMO, inflammatory bowel disease, and pediatric trauma care.
Our freestanding 190-bed UCSF Benioff Children’s Hospital Oakland offers emergency care and comprehensive inpatient services – including a 44-bed Neonatal Intensive Care Nursery and a 24-bed Pediatric Intensive Care Unit. Over 10,000 children are admitted and over 8,000 Operating Room cases are performed annually. Our Level 1 pediatric trauma center is one of the busiest in the state with over 1,000 major trauma admissions annually. The UCSF pediatric surgery faculty in Oakland maintain a broad and high-volume general pediatric surgical practice that encompasses common childhood problems from hernias, pilonidal disease, vascular access, emergency general surgery, aerodigestive foreign bodies, GYN emergencies, and trauma; to complex neonatal and pediatric problems including congenital anomalies, tumors, chest wall deformities, complex gastrointestinal surgery, anorectal malformations, and neonatal surgical emergencies
Faculty Information
Program Director: Hanmin Lee, MD
Associate Program Director: Aaron Jensen, MD-APD and site director, Oakland
Lan Vu, MD-APD and site director, SF
Program manager: Julie Link
415-476-6493
julie.link@ucsf.edu
Faculty:
James Betts, MD
Sarah Cairo, MD, MPH
Michael Harrison, MD emeritus
Olajire Idowu, MD
Aaron Jensen, MD, MEd, MS
Sunghoon Kim, MD
Hanmin Lee, MD
Tippi MacKenzie, MD (Research)
Willieford Moses, MD
Christopher Newton, MD
Amar Nijagal, MD
Doruk Ozgediz, MD, MSc
Lan Vu, MD, MAS
Fellow Information
Number of fellows: one per year
Current fellow(s):
Gabriella Grisotti, MD,PhD
Previous 5 fellows:
Maria Carmen Mora, MD
Graduated July 31, 2023
Assistant Professor-University of Texas Medical Branch at Galveston
Chinwendu Onwubiko, MD, PhD
Graduated July 31, 2021
Assistant Professor-University of Alabama Birmingham
Curriculum Information
Block Diagram: Click Here
BCHSF: Home call on every Tuesday night, Home call every other weekend (Friday 6pm to Monday 6am)
Support for in house surgical resident who takes primary call for all service questions and consults
BCH Oakland:
- Home call Mon-Thurs for index cases only (come in 1-2 nights per month on average)
- In-house call Friday nights
- Post-call every Saturday, off every Sunday
Conference Schedule:
Tuesdays
6:45-7:45 a.m. Fellow Education Conference (both sites)
10:00-10:30 a.m. Mission Bay Clinic Meeting (SF only)
10:30-11:30 a.m. Pediatric Surgery-BCHSF/BCH Oakland/Kaiser (both sites)
12-1:30 p.m. Tumor Board-Mission Bay Benioff Children's Hospital A1601A (SF only)
1:00-2:00 p.m. Fetal Diagnosis Conference C3810A/B (SF only)
Wednesdays
7:00‐8:00 a.m. Trauma Conference (OAK only-4th Weds)
8:00‐9:00 a.m. Trauma Advisory Conference (OAK only-4th Weds)
11:30 a.m.-12:30 p.m. Ped Surg Grand Rounds (1st Weds-both sites)
11:30 a.m.-12:30 p.m. Combined M&M (2nd Weds-both sites)
11:30 a.m.-12:30 p.m. Clinical Issues and Collaborations (3rd Weds-both sites)
11:30 a.m.-12:30 p.m. Journal Club (4th Weds-both sites)
Program Information
RRC accreditation status: Continued Accreditation without Outcomes
Meeting/Training Course policy: Pays for Transition to Fellowship bootcamp, St. Jude oncology course, MIS course, Colorectal course, APSA meeting, AAP meeting plus any additional meetings if fellow presenting own work. Time away subject to RRC regulations governing time in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1100 cases per two-year fellowship
Board passage rate (3 years): N/A
Fellow salary: PGY-6 $102,572.00; PGY-7 $105,443.00 (Housing stipend is included in salary rather than as a separate payment)
University of Chicago Comer Children’s Hospital
Last updated: November 2024
Program website: https://surgery.uchicago.edu/education/pediatrics-surgery-fellowship
This two-year fellowship is an ACGME-accredited program that consists of extensive clinical and surgical training in pediatric surgery, including trauma, ECMO, oncology, congenital abnormalities, minimally invasive surgery, subspecialty and critical care services. Applicants must have completed training in general surgery and be eligible to take the qualifying examination in general surgery given by the American Board of Surgery or the Royal College of Surgeons of Canada. Interested applicants should apply to the program via the Electronic Residency Application Services (ERAS). One fellow is selected every other year through the National Resident Matching Program (NRMP). The program start date is August 1, and the end date is July 31 of the second year.
Institution Information
The University of Chicago Comer Children’s Hospital
Chicago, IL United States
Number of beds: 172
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Welcome to the University of Chicago Section of Pediatric Surgery. We are proud to be a part of one of America’s premier universities and to share with you our rich surgical history matched only by our ongoing commitment to excellence in patient care, research and teaching. The Pediatric Surgical Subspecialty group at the University of Chicago performs more than 4,000 operations each year for a variety of childhood diseases. The clinical faculty offers world-renowned expertise in all aspects of pediatric surgical care with complete, well-balanced programs in General Surgery, Otolaryngology, Neurosurgery, Plastic Surgery, Orthopedics and Urology. The hallmark of the Pediatric General Surgery program is an AGCME-accredited, two-year fellowship training program in Pediatric General Surgery. The program has a broad clinical emphasis with clinical programs in minimally invasive surgery (MIS), Vascular Anomalies, Colorectal Reconstruction, Aerodigestive Disease, Chest Wall Deformities, Median Arcuate Ligament Syndrome (MALS), Hyperthermic Intra-Peritoneal Chemotherapy (HIPEC), Level 1 Pediatric Trauma Center, and Extracorporeal Membrane Oxygenation (ECMO). In addition to these unique programs, the general surgery group performs traditional pediatric surgical procedures ranging in complexity from high index neonatal surgery to routine hernia surgery. Our fellows receive a broad-based training from faculty that are deeply invested in the education of future pediatric surgeons. The Otolaryngology group provides a vast range of complex services from endoscopic sinus surgery and cochlear implantation to traditional myringotomy tubes for otitis media. There is ongoing seminal research in allergic rhinitis supported by NIH funding. The Neurosurgery group supports all aspects of pediatric surgery including neuro-oncology, neurovascular surgery, functional neurosurgery, epilepsy and minimally invasive surgery, allowing unprecedented access to innovative treatments. There is ongoing research in hydrocephalus physiology supported by NIH funding. The Orthopedics group performs a wide range of procedures ranging in complexity from complicated scoliosis surgery to routine fracture care. The Urology group has a renowned national expert in bladder reconstruction and complex congenital urological anomalies who performs a wide range of minimally invasive procedures including robotic surgery ranging from innovative/complicated urological reconstruction to traditional hypospadias repair. Along with our clinical and research activities, we emphasize a rich and vibrant academic environment for the education of medical students, residents, and fellows. We seek to create an environment that will foster the development and growth of our future medical leaders.
Faculty Information
Program Director:
Manish Raiji, MD
mraiji@bsd.uchicago.edu
(773) 702-6175
Associate Program Director:
Grace Mak, MD
gmak@bsd.uchicago.edu
(773) 702-6175
Program manager:
Selena Gonzalez
Sgonzalez5@bsd.uchicago.edu
(773) 641-7478
Faculty:
Grace Mak, MD – Professor; Chief, Section of Pediatric General Surgery; Surgeon-in-Chief, Comer Children’s Hospital
Jessica Kandel, MD — Mary Campau Ryerson Professor of Surgery
Thomas Lee, MD — Professor
Marion Henry, MD, MPH – Professor
Brian Jones, MD — Associate Professor
Deborah Loeff, MD — Associate Professor
Manish Raiji, MD, MA — Associate Professor
Bethany Slater, MD, MBA – Associate Professor
Charlotte Kvasnovsky, MD – Assistant Professor
Carmelle Romain, MD — Assistant Professor
Baddr Shakhsheer, MD – Assistant Professor
Fellow Information
Number of fellows: One every year
Current fellow(s):
Laura Rausch, MD
Vanderbilt University Hospital
Previous 5 fellows:
Saunders Lin, MD
2024
Assistant Professor, La Bonheur Children’s Hospital
Memphis, TN
Frances Okolo, MD
2022
Assistant Professor, East Carolina University Health
Greenville, NC
Marielena Bachier-Rodriguez, MD
2021
Assistant Professor, University of Chicago
Chicago, IL
Minna Wieck, MD
2020
Assistant Professor , University of California at Davis
Sacramento, CA
Lindsay Talbot, MD
2018
Assistant Professor, St Judes Children’s Hospital
Memphis, TN
Curriculum Information
Call Schedule
1st year: In-house every other Saturday, Home call one night
2nd year: Home call — once per week and every other weekend
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Each fellow will have the opportunity to attend the following courses/conferences:
- American Pediatric Surgical Association (APSA)
- Pediatric Colorectal Course (Pena) in Colorado
- Course for Advanced Minimally Invasive Surgery (Northwestern) as well as an additional course of the fellow’s choosing
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1100
Board passage rate (3 years): 100%
Fellow salary: N/A
University of Connecticut Pediatric Surgery Fellowship At Connecticut Children’s
Last updated: September 2023
Program website: https://www.connecticutchildrens.org/
We strive to train dedicated, clinically excellent pediatric surgeons. We enjoy working with self-motivated surgeons that share our love for children. Our strength is our diverse faculty that truly enjoys training our future pediatric surgeons.
The Pediatric Surgery Fellowship Program sponsored by the University of Connecticut is a two-year program that provides the fellow with experience in clinical and operative settings. Our program takes one fellow every 2 years. It is a competency-based program, which emphasizes learning through hands-on experience. The goal of the program is to produce graduates that are autonomous, enthusiastic and dedicated to the field.
Connecticut Children’s Medical Center is a nationally recognized, 187-bed not-for-profit free standing children’s hospital in Hartford, Connecticut. Connecticut Children’s fosters a patient-and family-centered environment with a focus on research, education, and advocacy. Connecticut Children’s serves as the primary pediatric teaching hospital for the UConn School of Medicine, has a teaching partnership with the Frank H. Netter MD School of Medicine at Quinnipiac University and is a research partner of The Jackson Laboratory. The hospital has a 32-bed neonatal intensive care unit located at Connecticut Children’s and 40-bed neonatal intensive care unit located at the UConn Health Center in Farmington, CT, an 18-bed pediatric intensive care unit, 97 medical/surgical beds, 8 operating rooms, an ambulatory surgery center in Farmington with 4 rooms and a 24-hour pediatric emergency department. Connecticut Children’s welcomes, cares for and protects all children who walk through our doors. We are an institution of acceptance and compassion regardless of nationality or immigration status.
Institution Information
Connecticut Children’s
Hartford, CT United States
Number of beds: 187
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Connecticut Children’s is the only hospital in Connecticut dedicated exclusively to the care of children and ranked one of the best children’s hospitals in the nation and a Magnet® designated hospital. Connecticut Children’s provides more than 30 pediatric specialties along with community-based programs to uniquely care for the physical, social, and emotional needs of children. Our team of pediatric experts and care coordinators bring access to breakthrough research, advanced treatments for both rare and common diseases, and innovative health and safety programs to every child. Connecticut Children’s is a not-for-profit organization with a mission to improve access to healthcare for all children through convenient locations, care alliances and partnerships.
Faculty Information
Program Director: Christine Finck, MD
Associate Program Director: Richard Weiss, MD
Program Manager: Marianne Custer, BS, C-TAGME
mcuster@connecticutchildrens.org
860.837.6260
Fellowship Program Coordinator: Allison Williams, BA
Awilliams05@connecticutchildrens.org
860.837.6262
Faculty:
Christine Finck, MD, FACS — Surgeon-in-Chief, Division Head
Richard Weiss, MD, FACS — Medical Director, Pediatric Surgery Division
Brendan Campbell, MD, MPH, FACS — Medical Director Pediatric Trauma Program; Chief Surgical Quality Officer
James Healy, MD, MHS — Pediatric Surgeon
J. Leslie Knod, MD — Pediatric Surgeon
Christine Rader, MD, FACS — Surgical Director, Extracorporeal Membrane Oxygenation Program
Donald W. Hight, MD — emeritus
Michael Bourque, MD — emeritus
Katerina Dukleska, MD — Pediatric Surgeon
Jacob Campbell, DO — Pediatric Surgeon
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Danielle Dougherty
Previous 5 fellows:
Jacob Campbell, DO
2023
Pediatric Surgeon at Connecticut Children’s Medical Center
Katerina Dukleska, MD
2021
Pediatric Surgeon at Connecticut Children’s Medical Center
James Healy, MD
2019
Pediatric Surgeon at Connecticut Children’s Medical Center
Yue-Yung Hu, MD
2017
Pediatric Surgeon at Ann and Robert H. Lurie Children’s Hospital, Chicago
Anthony Tsai, MD
2015
Pediatric Surgeon at Penn State Hershey Medical Center
Kimberly Ruscher, MD, MPH
2013
Pediatric Surgeon at Sacred Heart Medical Center, Oregon
Curriculum Information
Block Schedule
Our Pediatric Surgery Fellowship experience is designed to produce a competent and superb pediatric surgeon.
The rotations are designed to provide outstanding didactic teaching and operative experience. The curriculum is set in a longitudinal fashion that involves exposure to the clinics, to the operating room, to the emergency room and trauma bays, and through quality improvement projects. Twenty-two months are spent working with key faculty from the department of pediatric surgery, one month is spent focusing pediatric care in our Pediatric ICU, and one month is spent focusing on neonatal care in our Neonatal ICU.
Block Schedule
In first year, fellow will rotate on pediatric surgery, NICU, and PICU.
In the second year, the fellow will rotate on pediatric surgery.
Weekly Schedule Template
Mondays: Inpatient rounds, Operating Room
Tuesdays: Fellow Clinic in am; Clinic in pm
Wednesdays: Inpatient rounds in am; OR, Administrative time in pm
Thursdays: Inpatient rounds, Operating room
Fridays: Inpatient rounds; Operating room
Sign-out of patients in the afternoon usually occur at 4pm
Research: Fellows will be required to participate in one quality improvement project during their two-year fellowship training program.
Call Schedule
1st Year – typically from home and q 2
Occasional in house call required
2nd Year – typically from home and q 2
Conference Schedule
Below is a list of our conferences at which fellows are expected to attend and participate. We expect attendance at all weekly conferences, tumor board meetings, Tuesday education session, and grand rounds meetings unless the fellow is on vacation or unless emergent clinical duties preclude attendance.
Surgery/Pathology/Radiology Conference- Quarterly, 7-8 am, Connecticut Children’s
Members of the above departments (including fellows) attend. This meeting correlates and discusses specific cases with Radiological differential diagnoses and Pathological confirmation in a teaching setting.
Morbidity and Mortality Conference occurs monthly.
Pre-Op Conference: Pre-Op patients are discussed weekly at Tuesday conference.
Pediatrics Grand Rounds- Weekly, Tuesdays, 8-9 am, Virtual
This conference is attended by the Connecticut Children’s Medical Center Medical Staff, House Staff, Advance Practice RNs, Community Pediatricians, Physician Assistants, Fellows and Fellows. Topics change as to inform attendees of new developments in various areas of health care for children.
Tuesday education conference: Tuesday, 9:00-11:00 am, Connecticut Children’s
The attendings, fellows, fellows, and medical students will attend this meeting. The fellow is responsible for organizing and leading this conference. A list of topics will be given at the beginning of the year and will follow the PedScore format. In addition, topics will be supplemented with journal club. Attending surgical faculty are available to help coordinate topics. Once a month Surgical and Trauma M&M cases are reviewed.
Pediatric Solid Tumor Board Meeting- Weekly-Check with Joanne – 2 or 3 out of the 4 Tuesdays, Tuesdays, Noon-1 pm, Connecticut Children’s This conference is attended by a multi- disciplinary group of physicians and nurses in the care of cancer patients.
Surgical Quality Conference- Quarterly, Thursdays, 7-8 am, Connecticut Children’s
A multi-disciplinary group of physicians involved in the care of surgical patients are invited to participate. Typically, two or three cases are presented by the attending surgeon. The patient’s history, physical examination, radiographic studies, operative intervention and post-operative course are reviewed in a peer reviewed setting.
PICU Conference - Quarterly
There is a PICU quarterly conference where interesting cases are discussed.
Annual Cooke Lecture- Visiting Professor in pediatric surgery gives grand rounds followed by division presentation of cases to visiting professor. The fellow is expected to participate.
Annual Tsvok Lecture – Visiting professor gives grand rounds on pediatric trauma. Fellow is expected to participate.
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Fellows are provided $2,000 at the beginning of their training for the purchase of education-related materials and annually they receive $2,000 to fund conference travel. In addition to those conference funds fellows who are presenting will receive another $2,000 for presenting funds. Time away subject to RRC regulations governing time in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: Approximately 1100 cases
Board passage rate (3 years): Qualifying exam- 100%; certifying exam 100% first pass
Fellow salary: 2023-2024 PGY6: $78,263.00
University of Florida
Last updated: November 2024
Program website: https://pediatric.surgery.med.ufl.edu/education/
We are in the match every other year as a single resident program allowing maximal exposure to index cases. The intensive two-year training program includes all aspects of pediatric surgery. In the first year, residents spend up to 2 months on electives which include neonatology and pediatric critical care. The second year is spent entirely on the pediatric surgery service. Further opportunities in pediatric congenital heart surgery and pediatric urology may be made available as desired by the resident. The organized didactic component of the residency includes a weekly case conference and a subject conference, which is based on the required contents from the American Board of Surgery, and the SCORE curriculum. Additionally, there is a monthly NICU/surgery journal club and twice-monthly divisional morbidity and mortality conference. Multi-disciplinary conferences that the pediatric surgery residents attend are pathology, tumor board, ECMO M&M, and PICU case conferences.
Strengths
- Broad range of exposure to complex cases, with wide referral base throughout North Central Florida, the Panhandle, and southern Georgia.
- Specialty programs (IBD, intestinal failure, ECMO, burns) allow for exposure to niche practices and guidance to develop these programs after training.
- Pediatric surgeons at UF get the majority of airway and esophageal foreign bodies, and acute testicular cases.
- Adolescent gynecology cases are also performed by the pediatric surgeons.
- Rigorous teaching environment that focuses on the fellow, with opportunities for the fellow to begin their career development.
Weaknesses
- Pediatric transplant is rebuilding, is within the transplant division of the UF Department of Surgery.
- Single-fellow program.
Institution Information
Shands Children’s Hospital at the University of Florida
Gainesville, FL
Number of beds: 210
Percentage of time at this location: 100%
Training site type: Children’s hospital within adult hospital
pediatric surgery: 1860 cases/year
Faculty Information
Program Director: Janice Taylor, MD, MEd
Associate Program Director: Steven Raymond, MD
Program manager: Michelle DiGiacomo
michelle.digiacomo@surgery.ufl.edu
(352) 594-5119
Faculty: Shawn Larson, MD – Interim Chief
Ana Do, MD
Steven Raymond, MD
Janice Taylor, MD, MEd
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Heather Liebe, MD
Previous 5 fellows:
Russell Hawkins, MD
2024
Assistant Professor, UT-Southwestern
Dallas TX
Faidah Badru, MD
2022
Assistant Professor, West Virginia University
Charleston WV
Kevin Johnson, MD
2020
Assistant Professor, Vanderbilt University
Nashville, TN
Faraz Khan, MBBS
2018
Associate Professor, Stanford University
Palo Alto, CA
Daniel Solomon, MD
2016
Assistant Professor, Yale University
New Haven, CT
Curriculum Information
Call schedule:
1st Year - Q3 home call
2nd Year - Q3 home call
Conference Schedule:
Example week:
Monday AM case conference
Wednesday AM pediatric surgery subject conference or division M&M
Thursday AM pediatric surgery subject conference
Friday AM departmental M&M and grand rounds
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: St. Jude course, MIS course, colorectal course, APSA & AAP annual meetings, other meetings if fellow has presentation accepted. Time away subject to RRC regulations governing time in training
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1400
Board passage rate (3 years): 100%
Fellow salary: https://financeadmin.med.ufl.edu/com-hr/benefits/housestaff-benefits/housestaff-stipends/
University of Iowa/ Stead Family Children's Hospital
Last updated: September 2023
Program website: https://gme.medicine.uiowa.edu/pediatric-surgery-fellowship
At the University of Iowa Pediatric Surgery Fellowship program, we look forward to training diverse candidates who are enthusiastic about developing expertise in the pre-operative, operative, and post-operative management of infants and children. As the only quaternary referral center in the state and region, we see an impressive range of operative pathology and care for highly complex patients. Our faculty have varied clinical backgrounds, are at different stages in their careers, and prioritize fellow education. Our didactic training component prepares fellows to become competent pediatric surgeons, dedicated teachers, and life-long learners. Our clinical team includes surgical residents, nurse practitioners, and clinical nurse specialists who are collegial, collaborative, and committed to assuring prioritization of fellow education. Our fellowship offers a diverse and complex case load given our status as the only quaternary referral center in the state, collaborative relationships with NICU and PICU providers, a clinical team that prioritizes fellow education, and career counseling/coaching integrated into training program. We are unable to offer exposure to transplantation. Upon completion of the two-year program, fellows are qualified for certification in Pediatric Surgery by the American Board of Surgery.
Strengths
- Diverse and complex case load given our status as the only quaternary referral center in the state, collaborative relationships with NICU and PICU providers, clinical team that prioritizes fellow education.
- Career counseling, coaching and leadership training are integrated into training program.
- We train one fellow at a time, which requires the pediatric surgery trainee to lead for clinical team starting on day one. It also requires the pediatric surgical trainee to be prepared to perform complex pediatric surgical procedures starting on day one.
Weaknesses
- No operative transplantation exposure.
- There are no other pediatric surgical fellows on service.
Institution Information
University of Iowa Stead Family Children’s Hospital
Iowa City, IA United States
Number of beds: 190
Percentage of time at this location: 100%
Training site type: Free standing children's hospital which opened in December 2016.
The University of Iowa Stead Family Children’s Hospital is Iowa’s only nationally ranked children’s hospital featuring additional “Only” designations such as the only Level 4 NICU, only Level 1 Trauma Center for pediatrics, and only pediatric surgery team. We cared for nearly 84,000 patients last year from every one of Iowa’s 99 counties, 45 states, and 20 countries.
More information is available at https://uichildrens.org/
Faculty Information
Program Director: Joel Shilyansky, MD
Associate Program Director: Erica Carlisle, MD
Program manager: Cate Unruh, MEd
cate-unruh@uiowa.edu
319-467-5302
Faculty:
Erica Carlisle, MD
Graeme Pitcher, MBBCh
Julia Shelton, MD, MPH
Joel Shilyansky, MD
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Alexis Bowder, MD,MPH (Aug 2023-Aug 2025
Previous 5 fellows:
Lindel Dewberry, MD (Aug 2021 – July 2023)
Assistant Professor in the Department of Surgery
University of Kentucky
Lexington, KY
Benjamin Farber, MD (Aug 2019 – July 2021)
Assistant Professor in the Department of Surgery
The Children’s Hospital at Montefiore
Bronx, NY
Sarah K. Walker, MD (July 2017 – June 2019)
Assistant Professor in the Department of Surgery
Texas Tech University, El Paso
El Paso, Texas
Curriculum Information
Call Schedule
1st year: Home – Q3
2nd year: Home – Q3
Conference Schedule
Click Here
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: UIHC pays for Transition to Fellowship bootcamp, general surgery board prep, St. Jude course, MIS course, Colorectal course, APSA meeting, AAP meeting plus any additional meetings if fellow presenting own work. Time away subject to RRC regulations governing time in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1057
Board passage rate (3 years): 100%
Fellow salary: PGY-6 $76,500; PGY-7 $79,400
University of Louisville
Last updated: 10/18/2023
Program website: https://louisville.edu/medicine/departments/surgery/fellowships/pediatric-surgery
Recruitment Brochure:
Overview of Fellowship:
The Pediatric Surgery Fellowship Training Program at the University of Louisville / Norton Children’s Hospital is a “one fellow” program, accepting one fellow every other year. The program focuses on the clinical education of the fellow, with ample opportunity for experience of a wide variety of cases. The program offers excellent exposure to neonatal pathology, supported by one of the largest neonatal intensive care units in the country. While formal rotations in other surgical disciplines are not part of the formal curriculum, ample opportunity to care for patients with cardiac, urological, orthopedic, and otolaryngologic issues is available due to a limited number of fellows of other surgical specialties in the hospital.
Program self-reported strengths:
Large case volume, high faculty to fellow ratio, single-fellow program, extensive neonatal experience. The program includes ECMO, burn and trauma responsibilities.
Program self-reported weaknesses:
Very busy clinical program, rotations available in Cardiac Surgery, Urology, and other surgical subspecialties but not part of the formal required curriculum. No transplant experience as part of the fellowship training.
Institution Information
Norton Children’s Hospital
Louisville, KY United States
Number of beds: 300
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Norton Children’s is a leader in caring for children throughout Louisville, Southern Indiana, the Commonwealth of Kentucky and beyond. As the region’s only full-service, free-standing pediatric hospital, Norton Children’s Hospital, along with its predecessor hospitals, has cared for children for more than a century without regard to their families’ ability to pay. The 300-bed hospital is Louisville’s only Level I Pediatric Trauma Center and serves as the primary pediatric teaching facility for the University of Louisville School of Medicine.
The Norton Children’s system offers comprehensive inpatient and outpatient pediatric care, including a full range of services for congenital and acquired heart disease, cancer care, neurosciences, spine and orthopedic care, and neonatal care.
This is a busy clinical program with extensive operative and patient care experience. Fellows typically complete 1400-1800 operative cases during their fellowship, and exceed all “required” case minimums. The Pediatric Surgery Service typically performs 3000-4000 total cases per year.
Faculty Information
Program Director: Tiffany Wright, MD
Associate Program Director: Cynthia Downard, MD, MMSc
Program manager: Lisa Pantoja, BS
lisa.pantoja@louisville.edu
502-629-8630
Faculty:
Mary E. Fallat, M.D.
Professor of Surgery
University of Louisville
Surgical Quality Officer Norton Children’s Hospital
Sheldon J. Bond, MD
Professor of Surgery
University of Louisville
David Foley, MD
Professor of Surgery
University of Louisville
Trauma Medical Director Norton Children’s Hospital
Cynthia Downard, MD, MMSc
Professor of Surgery
Associate Program Director Pediatric Surgery
University of Louisville
Tiffany Wright, MD
Associate Professor of Surgery
Program Director Pediatric Surgery
University of Louisville
Director Surgical Critical Care Norton Children’s Hospital
Stewart Carter, MD
Assistant Professor of Surgery
University of Louisville
Christie Buonpane, MD
Assistant Professor of Surgery
University of Louisville
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Jonathan Vacek, MD
Previous 5 fellows:
Julia Shelton, MD, MPH
2013-2015
Program Director- General Surgery
University of Iowa
Iowa City, IA
Tiffany Wright, MD
2015-2017
Associate Professor
University of Louisville
Louisville, KY
Andrea Doud, MD
2017-2019
Assistant Professor
University of Kentucky
Lexington, KY
Kevin Riggle, MD
2019-2021
Gundersen Health System
University of Wisconsin
LaCrosse, WI
Heron Baumgarten, MD
2021-2023
Private Practice
Western Surgical Group
Reno, NV
Curriculum Information
Block Schedule
First year: one month PICU rotation, one month NICU rotation, remainder General Pediatric Surgery
Second year: General Pediatric Surgery
Call Schedule
1st year: The fellow alternates call from home with the PGY4 resident. In house call responsibilities average one night per week.
2nd year: The fellow alternates call from home with the PGY4 resident. In house call responsibilities average one night per week.
Conference Schedule
| Day/Time | Conference | Day/Time | Conference | |
| Every Monday 700 | M&M Conference (PGY2)
Weekly Case Preview(PGY2) |
1st Tuesday 1200
1st Tuesday 1300 |
Radiology Conference (Fellow)
Research Meeting (Beth McClure –Research Nurse) |
|
| 2nd Tuesday 1200 | General Tumor Board | |||
| 2nd Tuesday 1300 | SCORE Curriculum (Fellow) | |||
| 3rd Tuesday 1200 | PICU Journal Club (PICU Leader) | |||
| 3rd Tuesday 1300 | SCORE Curriculum(Fellow) | |||
| 4th Tuesday 1200 | Surgical Tumor Board | |||
| 4th Tuesday 1300 | SCORE Curriculum (Fellow) | |||
| 5th Tuesday 1200 | Faculty Retreat |
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The program supports attendance at the AAP Transition to Practice Program, APSA, the St Jude Oncology Review Course, an MIS Course, an Anorectal Course, the Pediatric Surgery Capstone Course, and other educational opportunities as deemed appropriate.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: Fellows complete 1400-1800 operative cases during their fellowship.
Board passage rate (3 years): 100%
Fellow salary: PGY-6 - $70,834; PGY-7 - $73,781
University of Michigan CS Mott Children's Hospital
Last updated: December 2024
Program website: https://medicine.umich.edu/dept/surgery/surgical-specialties/pediatric-surgery/training
At Michigan Pediatric Surgery Fellowship Programs, we’re looking for leaders and innovators who want to change the way pediatric surgery is practiced and delivered. Whatever your future goals are as a surgeon, we’ll give you the training and resources to get there. We offer fellowship programs in pediatric surgery, pediatric surgical critical care, medical innovation in pediatrics, fetal diagnosis and treatment, and clinical research in pediatric surgery. Your training ground is the University of Michigan’s high-volume academic medical center, Michigan Medicine, home to C.S. Mott Children’s Hospital, a modern 12-story facility featuring a dedicated pediatric emergency and trauma care center, as well as an operating suite featuring the latest technologies, including intra-operative MRI capability.
Here’s why training at Michigan will prepare you to lead in the profession:
- Training across the spectrum of specialties: Our physicians are internationally recognized experts in a broad range of pediatric surgery specialties, with core strengths in oncology, minimally invasive surgery including interventional radiology, critical care including ECMO, and neonatal surgery. You’ll benefit from working with an adept and caring faculty whose diverse experiences and areas of interest will spark and complement your own.
- Meaningful and immediate feedback: Faculty in the section provide frequent and timely feedback to fellows through in-person assessment as well as a novel smartphone-delivered survey. You’ll learn more, faster, through this ongoing feedback loop, building your autonomy as a surgeon as your training progresses.
- Extensive research opportunities: With more than $2 million in annual external sponsorship for Pediatric Surgery primary investigators, as well as longstanding partnerships across institutions, our research network is vast. Fellows will have their pick of opportunities to participate in research, from basic science to health services.
- Foundational knowledge in engaged settings: Fellows integrate quickly into the clinical rhythms of the department by participating in weekly conferences, including a pediatric tumor board, a multi-site patient management conference, a radiology/pathology conference, a PedScore lecture series, Pediatric Surgery Grand Rounds, morbidity/mortality conference, and multidisciplinary conferences in vascular anomalies, inflammatory bowel disease, neonatology, ECMO, and fetal management. You’ll learn clinical decision-making from physicians across multiple disciplines, and gain experience by presenting your own cases and receiving feedback.
- Research Education: We offer training for research in the field of pediatric surgery, giving our trainees time to develop advanced investigative skills and explore research projects. Our faculty work with trainees pursuing research throughout the University of Michigan, from fellows in our specialized Pediatric Surgery Research Fellowship to undergraduates in the Undergraduate Research Opportunity Program (UROP). Throughout your time at Michigan, you’ll form friendships with peers and mentors that will invigorate your career trajectory now and into the future.
Institution Information
University of Michigan CS Mott Children's Hospital
Ann Arbor, MI United States
Number of beds: 302
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
U.S. News & World Report ranked Michigan Medicine C.S. Mott Children’s Hospital among the nation’s best children’s hospitals. U-M the only children’s hospital ranked in all ten categories, but Michigan is also ranked higher than every other children’s hospital in the state in every category evaluated. In 2017, University of Michigan C.S. Mott Children’s Hospital received verification as a Level 1 Children’s Surgery Center by the American College of Surgeons. The ACS Children’s Surgery Verification Quality Improvement Program was developed to improve the quality of children’s surgical care by creating a system that helps match each child’s individual surgical needs with the best care environment. With this designation, Michigan became one of the first level 1 children’s surgical centers in the nation. At Michigan Pediatric Surgery, we’re proud of the well-rounded enterprise we’ve built — performing nearly 2,500 operations a year in our fast-growing specialty practice; advancing pediatric surgery knowledge and practice through NIH-funded research; and offering collegial and unique fellowship training experiences. We’re motivated by providing the very best care to our patients while improving the health of children everywhere as we help create the future of pediatric surgery.
Faculty Information
Program Director: Samir Gadepalli, MS, MD, MBA
Associate Program Director:
Joe Church, MD
Byron Hughes, MD
Program manager: Megan Conard
conardme@med.umich.edu
Faculty:
Erika A. Newman, MD – Section Chief
Meghan Arnold, MD
Joseph Church, MD
Peter Ehrlich, MD
Samir Gadepalli, MD
Ronald B. Hirschl, MD
Byron D. Hughes, MD
George B. Mychaliska, MD
Erin E. Perrone, MD
Robin T. Petroze, MD
K. Elizabeth Speck, MD
Arul S. Thirumoorthi, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Abigail Engwall-Gill, MD
Brittany Johnson, MD
Previous 5 fellows:
Aaron Beckwith, MD
2024
Dell Children’s Medical Center
Austin, Tx
Aimee Kim, MD
2023
Assistant Professor of Surgery, Children’s Hospital
Los Angeles, CA
Cory Criss, MD
2022
General Pediatric Surgery, Nationwide Children’s
Columbus, OH
Joseph Church, MD
2021
Assistant Professor of Surgery, University of Michigan
Ann Arbor, MI
Natasha Corbitt, MD
2020
Assistant Professor of Surgery, UT Southwestern
Dallas, Tx
Curriculum Information
Call Schedule
1st year: no in house call back up at home 1 in 2 come in for level 1 traumas
2nd year: no in house call back up at home 1 in 2 come in for level 1 traumas
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Program will pay for APSA and colorectal conference in years 1 and AAP and one other conference in year 2
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1247
Board passage rate (3 years): 100%
Fellow salary: $87,934 (2024-PGY 6)
University of Mississippi Medical Center – Pediatric Surgery Fellowship Program
Last updated: 1/12/2023
Program website: https://www.umc.edu/som/Departments%20and%20Offices/SOM%20Departments/Surgery/Fellows/Pediatric-Surgery/Pediatric-Surgery1.html
Our fellowship is an ACGME-accredited two-year program that is designed to develop proficiency in the care of infants, children and adolescents with surgical problems. Our program began in 2012 under the direction of Dr. Christopher Blewett.
We designed our program to provide an educational experience which results in a trainee acquiring the knowledge and skills to become a proficient and independent practitioner of pediatric surgery. Whether your goal is to be in a private practice or a faculty appointment in an academic medical center, our program will give you a broad-based training experience.
In the fellow’s first year of training, clinical rotations in pediatric surgery as well as PICU and NICU lay the foundation; the second year of training is devoted exclusively to pediatric surgery. While clinical rotations are necessary, it must be realized that these rotations are not sufficient to achieve the overall goal. A robust program of didactic learning is also required to develop the knowledge base needed by a pediatric surgeon. This is accomplished through our weekly conference and teaching schedule. When you successfully complete our pediatric surgery fellowship program, you will be eligible to take the qualifying and certifying examinations offered by the American Board of Surgery.
Institution Information
Batson Children’s Hospital at the University of Mississippi Medical Center
Jackson, MS United States
Number of beds: 250
Percentage of time at this location: 100%
Training site type: Children’s hospital within adult hospital
Batson Children’s Hospital is the flagship of Children’s of Mississippi, part of the University of Mississippi Medical Center (UMMC). As Mississippi’s only children’s hospital, we care for kids from across the state, offering everything from emergency care to highly specialized heart and cancer care for kids.
Batson Children’s Hospital treats about 150,000 children each year in more than 30 specialty areas, including newborn medicine, pediatric cardiology, neurology, and surgery. It houses the state’s only pediatric intensive care unit and emergency department along with Mississippi’s only pediatric treatment programs for cancer, cystic fibrosis, sickle cell anemia, congenital heart defects, and more.
Faculty Information
Program Director: David E. Sawaya, Jr.
Associate Program Director:
Program manager: Stacy Burgess
sburgess@umc.edu
(601) 984-5102
Faculty:
Christopher Blewett, MD — Dr. Richard C. Miller Chair of Pediatric Surgery; Surgeon-in-Chief, Children’s of Mississippi
Barry Berch, MD — Associate Professor
Michael W. Morris Jr., MD — Assistant Professor
David E. Sawaya, Jr., MD — Professor
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Colin Muncie, MD
Previous 5 fellows:
Dan W. Parrish, MD
2019
West Virginia University, Morgantown WV
Michael W. Morris, Jr., MD
2017
University of Mississippi Medical Center, Jackson MS
Richard S. Herman, MD
2015
Case Western Rainbow Babies; Cleveland OH
Tamarah Westmoreland, MD, PhD
2013
Nemours Children’s Hospital, Orlando FL
Curriculum Information
Block Schedule
| Year 1 | Aug | Sept | Oct | Nov | Dec | Jan | Feb | March | April | May | June | July |
| Rotation | Peds Surg | Peds Surg | Peds Surg | NICU | PICU | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg |
| % OP | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% |
| % Research | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% |
| Year 2 | Aug | Sept | Oct | Nov | Dec | Jan | Feb | March | April | May | June | July |
| Rotation | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg | Peds Surg |
| % OP | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% | 10% |
| % Research | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% | 5% |
Call Schedule
1st Year – in-house/home and every other weekend
2nd Year – in-house/home and every other weekend
Conference Schedule
Pediatric Surgery Grand Rounds Conference—A weekly didactic series devoted to essential topics in Pediatric Surgery. This will be organized by the Pediatric Surgery fellow and program director. A variety of Pediatric Surgery topics will be presented and discussed by Pediatric Surgery faculty, the fellow, residents as well as invited guest moderators from other sub-specialties including but not limited to urology, ENT, anesthesia. The final 10-15 minutes of the conference will include a review of the next week’s scheduled cases.
Divisional Morbidity & Mortality Conference—A twice monthly discussion of deaths and complications on the Pediatric Surgery service. Pediatric Surgery will continue to submit case logs for the departmental M&M, and participate in that conference as invited. The divisional conference is intended to be a more rigorous discussion of complications than is allowed in the departmental forum.
Pediatric Surgery Divisional Journal Club—A quarterly journal club meeting to discuss relevant Pediatric Surgery topics. The quarterly journal “Seminars in Pediatric Surgery” will be the primary source for these articles. This is a faculty-driven conference. The articles are presented by the Pediatric Surgery faculty and open for discussion with the fellow, residents and guest pediatric specialty divisions such as Pediatric Pulmonology, Pediatric Urology, etc.
Pediatric Surgery SCORE Conference—A twice monthly conference with mandatory attendance by all Pediatric Surgery faculty, the fellow, and any residents that wish to participate. This conference is designed to prepare the fellow for the Pediatric Surgery oral certifying exam. The SCORE curriculum will be completed in its entirety over 2 years for each fellow. We use the SCORE template to spawn oral board questions and allow the fellow to formulate answers and to simulate the certifying exam. Faculty critique the fellow’s knowledge base and ability to formulate appropriate and safe treatment algorithms.
Pediatric Surgery Attending Rounds—Rounds are accomplished every morning, led by the Pediatric Surgery fellow and residents. The Pediatric Surgery attending of the week sees every patient every day with the fellow, residents, medical students, and/or nurse practitioners. Care plans are formulated and teaching rounds are completed.
Tumor Board—A weekly conference at 1500 on Wednesdays, where the ongoing management of Pediatric Hematology-Oncology patients is discussed. The conference is multidisciplinary in nature, with representatives from Pediatric Hematology-Oncology, Radiology, Pathology, Radiation Oncology, Pediatric Surgery, Child Psychology, and Palliative Care in attendance.
Pediatric Trauma Performance Improvement Committee—A bimonthly meeting held the 2nd Tuesday of the month at 0700. This is a multidisciplinary meeting involving all pediatric subspecialties including but not limited to Pediatric Surgery, Orthopedics, Urology, Neurosurgery, Pediatric Intensivists, Emergency Medicine physicians and care providers.
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Program pays for fellow to attend APSA conference as a junior fellow (up to $2000)
Program pays for fellow to attend AAP conference as a senior fellow (up to $2000)
Additional funding based on fellow’s merit:
$500 with PSITE score >90%ile
$2000 for podium presentation at national meeting. Faculty co-author must attend podium presentation.
$1000 for podium presentation at regional meeting. Faculty co-author must attend podium presentation.
$2000 for poster presentation at national meeting
$1000 for poster presentation at regional meeting.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): 4 of 4 Examinees passed the QE on their 1st attempt; 2 of 3 Examinees passed the CE on their 1st attempt
Fellow salary: 2019-2020 Salaries: PGY-6 $59,337; PGY-7 $60,709
University of Missouri – Kansas City/Children’s Mercy Kansas City
Last updated: December 2024
Program web page URL Pediatric Surgery Fellowship | Children's Mercy Kansas City
Overview of Fellowship
The pediatric surgery program at Children’s Mercy Hospital is a recognized as a leader in innovative clinical care, minimally invasive surgery, and research excellence. The fellowship will allow each to gain knowledge and experience in physiology, the disease processes, and the preoperative, intra-operative, postoperative care of infants and children. In addition, fellows have the luxury of practicing in a model with evidence based clinical pathways and protocols with a low level of variation in care. To that end, we look for a fellow with a strong clinical and research background.
Institution Information
Children’s Mercy Kansas City
2401 Gillham Road
Kansas City, MO United States
Training site #1:
Name free standing children’s hospital
#beds 390
Percentage of time at this location: 100%
Brief description of other hospital information
Children’s Mercy is verified as a Level 1 Children’s Surgery Center and Level 1 Trauma Center accredited by the American Board of Surgeons
Faculty Information
Program Director: Rebecca Rentea, MD
Assistant Program Director (if applicable): Rich Hendrickson, MD
Program manager and email: Danelle Vogt, MBA
Dkvogt@cmh.edu
List of Faculty and titles
Shawn St. Peter, MD – Senior Vice President; Surgeon-in-Chief; Chair Department of Surgery
Charles Snyder, MD – Chief, Division General Surgery
Richard Hendrickson, MD – Associate Program Director Pediatric Surgery Program, Director, Surgical Director Intestinal Rehabilitation; Surgical Director, Prenatal Consultation
Pablo Aguayo, MD – Director Burn Program; Program Director Surgical Critical Care Fellowship Program
Tolulope Oyetunji, MD – Director, Surgical Scholars Program, Director Health Outcomes Research
Rebecca Rentea MD –Program Director Pediatric Surgery Program, Director Comprehensive Colorectal Center
Bhargava Mullapudi, MD - Chief, Section of Transplant Surgery and Co-Director of the Brendan Elam Transplant Center
Iris Lim-Beutel, MD, MPH – Surgical Director, Inflammatory Bowel Disease Clinic; Associate Director, Comprehensive Colorectal Center
Fellow Information
Number of fellows: one per year and one every other year (January)
Current fellow(s) names:
Mimi Denning, MD
Nathan Rubalcava, MD
AJ Gonzalez Salazar, MD
List of previous 5 fellows: name, grad year, current position
Charlene Dekonenko, MD
2022-2024
Christus Children's, San Antonio, TX
Christopher Laird, MD
2022-2024
Children’s Wisconsin, Milwaukee, WI
Angela Kao, MD
2021-2023
Inova Fairfax Hospital, Fairfax, VA
Omar Nunez-Lopez MD
2020-2022
Valley Children’s Hospital, Fresno, CA
Justin Sobrino, MD
2019-2021
Saint Louis University/Cardinal Glennon Hospital, St Louis, MO
Call schedule
Fellows take on average one in five nights in house call. The 80-hour work week and all ACGME regulations are strictly agreed to.
Conference Schedule
Rotating conferences 3 morning per week including M&M, fellow conference (mock oral boards), journal club, core curriculum lectures, trauma review, trauma radiology, neonatal conference, surgery/GI conference
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Time away subject to RRC regulations governing time in training. Program pays for all traditional fellow courses: colorectal, MIS, oncology, APSA, AAP and any other meetings where the fellow presents their research.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: 1777
Board passage rate (last 10 years): N/A
Fellow salary: Pediatric Surgery Fellowship | Children's Mercy Kansas City (childrensmercy.org)
2023-24 salaries:
PGY 6: $78,852.80
PGY 7: $81,224.00
PGY 8: $83,626.40
PGY 9: $85,342.40
PGY 10: $87,049.25
Benefits for fellows
$1,500 Educational stipend per academic year for books, travel and other educational materials
$2,250 Professional stipend for academic year to present scholarly activity
Health and dental insurance for trainee and dependents with no premiums
Hospital-issued iPad or laptop
Free parking
Moving allowance
20 days of vacation
Paid sick time
Paid board exam
Access to clinical and research librarians, statisticians, scientific writers and learning specialists
Tuition allowance of $5,250 per year
On-site fitness center and wellness center
University of Nebraska Medical Center Pediatric Surgery Fellowship
Last updated: 12/03/2021
Program website: https://www.unmc.edu/surgery/residencies-fellowships/pedsurgery-fellowship.html
The University of Nebraska Medical Center and School of Medicine two-year Pediatric Surgery Fellowship in Omaha is an integrated experience between 3 world class institutions, UNMC, Children’s Hospital and Medical Center, and Boys Town National Research Hospital. Approximately 95% of the fellow’s operative experience takes place at Children’s. The University setting offers a world class NICU, pediatric cancer treatment, and access to an excellent general surgery residency. Boys Town offers an extensive outpatient surgical and clinic experience. Children’s Hospital and Medical Center is a free standing, state of the art, modern Children’s Hospital that will serve as the primary clinical location for training and serves as the only large inpatient Pediatric Center in the region. The institution has 14 operating rooms with an annual operative volume of 12,400 cases. The Fellows are involved in a typical wide variety of common Pediatric Surgical cases. Fellows tend to far outpace recommended numbers required by the ACGME. Specialty clinics include the Colorectal Center, The Pectus Clinic, a multidisciplinary Thyroid clinic, and a Bariatric Program. Off-service month-long rotations in the first year include the NICU and PICU. The second year offers experience in Cardiothoracic, ENT and Pediatric Urology. We also offer an opportunity to work in Vietnam for 1-2 weeks in the second year.
The mission of the Pediatric Surgery fellowship is to prepare well-rounded, technically excellent and compassionate pediatric surgeons for a career in academics and surgical education, private practice, or a subspecialty practice using an apprenticeship model. By apprenticeship model, our fellows are assigned to one attending for several months. During that time they will have exposure to the attending’s clinic and meetings in order to better prepare them for independent practice. This helps in the understanding of how to negotiate, RVU’s, Quality Improvement, and Hospital Committees.
Institution Information
Children’s Hospital & Medical Center
Omaha, NE United States
Number of beds: 245
Percentage of time at this location: 90%
Training site type: Free standing children’s hospital
Children’s Hospital & Medical Center is a free standing, state of the art, modern Children’s Hospital that serves as the primary clinical location for training. Children’s serves as a referral center for a multi-state area performing more than 12,000 surgeries annually. The current $400 million expansion includes 10 new operating rooms and 100 beds in 250, 000 square feet.
University of Nebraska Medical Center
Omaha, NE United States
Number of beds: 800
Percentage of time at this location: 5%
Training site type: Children’s hospital within adult hospital
The University setting offers a world class NICU and general surgery residency. The 800 bed facility and houses a level 4 NICU with 35 beds and greater than 350 admits annually. There is also a busy bone marrow transplant program and some general pediatric beds. Approximately 100 cases are done/year at this site, which is 10 minutes from Children’s Hospital and Medical Center.
Faculty Information
Program Director: Abdalla Zarroug, MD
Associate Program Director: Megan Fuller, MD
Program manager: Jolene Krueger
jolene.krueger@unnc.edu
402-559-8591
Faculty:
Abdalla Zarroug, MD, FACS, FAAP, Division Chief and Professor of Pediatric Surgery. Program Director
Angela Hanna, MD, FACS, Assistant Professor of Pediatric Surgery
Fellow Information
Number of fellows: one every other year
Current fellow(s):
N/A
Previous 5 fellows:
Oliver Lao, MD
2013
Pediatric Surgeon, Joe DiMaggio Children’s Hospital
Connie Rossini, MD
2015
Pediatric Surgeon, Assistant Professor, Rush University
Jonathan Papic, MD
2017
Pediatric Surgeon, Sacred Heart Medical Group
Justin Wagner, MD
2019
Pediatric Surgeon, UCLA Health
Melissa Suh, MD
2020
Pediatric Surgeon, Boystown Hospital
Curriculum Information
Call Schedule
1st Year – in-house/home and home call: come in for index pediatric surgical cases.
2nd Year – in-house/home and home call: come in for index pediatric surgical cases.
Conference Schedule
| Conference Schedule | |||
| Day | Conference | Time | Place |
| Daily rounds at 7:30 8:00 on Tues/Friday |
|||
| Monday | Tumor Board | 4pm | |
| 1st Tuesday | GI conference | 7am | 4th floor SPC conf. room |
| 2nd Tuesday | Perinatal/ Neonatal | 7am | Glow Auditorium |
| 3rd Tuesday | Surg / Rad/ Path | 7am | Glow A |
| 4th Tuesday | Staff Meeting | 630 | Panera |
| 4th Weds | SPIPS | Classroom 1 | |
| 1st Friday | Journal Club | 7am | 4th floor SPC conf. room |
| 2nd Friday | M&M | 7am | 4th floor SPC conf. room |
| 3rd Friday | Academic Conference/ Core Lecture |
7am | 4th floor SPC conf. room |
| 4th Friday | M&M | 7am | 4th floor SPC conf. room |
| 5th Tues/ Friday | Make-up / missed conf. | 7am | 4th floor SPC conf. room |
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Program Pays for one meeting and one course per year plus any additional meetings if fellow presenting own work. This is usually APSA in the first year and AAP in the second. Most fellows have chosen to go to the Colorectal Course and the Cancer course.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: 1100
Board passage rate (3 years): 4 of 4 Examinees Passed QE on their 1st Attempt (75%). 4 of 4 Examinees Passed CE on their 1st Attempt (100%).
Fellow salary: HO VI: $71,141; HO VII: $74,735
University of Ottawa/Children’s Hospital of Eastern Ontario Pediatric Surgery Program
Last updated: 01/12/22
Program website: N/A
General overview statement that might include the following:
The Pediatric Surgery Sub-Specialty Residency Program at CHEO accepts one Canadian Medical Graduate per year for the training duration of two years. The main teaching site is CHEO (Children’s Hospital of Eastern Ontario). The pathway is fairly standard for most residents, ensuring they have access to the other necessary rotations, with some flexibility provided to allow them to explore the vastness of Pediatric Surgery. The program partakes in the National Residency Matching Program, through the Pediatric Surgery Fellowship, as a method of matching their applicants. Trainees will be qualified to sit for examinations in Pediatric General Surgery given by the Royal College of Surgeons of Canada and the American Board of Surgery.
Institution Information
CHEO (Children’s Hospital of Eastern Ontario) Ottawa Canada
Number of beds: 167
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
The Pediatric surgery program is based on consults in the outpatient department as well as the emergency room and from the inpatient wards. The volume is adequate to support the Pediatric surgery trainee. CHEO is also a designated site for trauma. In 2020-2021 there were 62 major trauma patients (defined by an ISS> 12) of that there were 33 trauma team activations. This also supports the non-operative trauma that is required for our Pediatric surgery trainee. In October 2020 to October 2021 a total of 1,112 operative cases were done of which 602 were elective, 510 were emergencies, and 329 cases were done after hours. These numbers certainly support the Pediatric surgery trainee in meeting all of his/her training requirements
Faculty Information
Program Director: Dr. Kyle Cowan
Program Admin and contact info: Ann Marie Tessier
613-737-7600 x 2803
Faculty:
Dr. Ahmed Nasr – Chief Division of Pediatric Surgery
Dr. Marcos Bettolli
Dr. Gilgamesh Eamer
Dr. Justyna Wolinska
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Fouad Youssef
Previous 5 fellows:
Simon Byrns 2019-2021 – Pediatric Surgeon, Edmonton Alberta
Troy Perry 2017 – 2019 – Pediatric Surgeon, Edmonton Alberta
Anwar Abdul Hadi – 2015-2017 – Pediatric Surgeon San Juan Puerto Ricco
Kathryn Martin – 2013-2015 – Pediatric Surgeon Hersey PA
Ramanath Haricharan 2011-2013 – Pediatric Surgeon Charleston WV
Curriculum Information
Block schedule:
1st year – NICU/PICU (4 weeks) and Pediatric Surgery Service
2nd year – Pediatric surgery, electives if requested (Urology/GI
Call Schedule
1st Year – Home Call – Q5
2nd Year – Home Call – Q5
Conference Schedule:
PS program pays for trainee to attend annually the CAPS (Canadian Association of Pediatric Surgeons) conference or APSA (American Pediatric Surgery Association) conference.
Regular conference schedules: weekly/monthly/annual:
Pediatric Surgery Teaching/Academic half day
Radiology Rounds
Combined NICU/MFM/Surgery
Tumor Board
QI/M&M
Journal Club
Research Rounds
Thyroid Rounds
National/Joint Rounds
Complex Case discussion
Program Information
RRC accreditation status: Continued Accreditation – Fully accredited by the RCPSC next full accreditation 2026
Meeting/Training Course policy: PS program pays for Transition to Fellowship Boot Camp, 2 courses plus CAPS/APSA in the first year and two courses plus CAPS/APSA during the 2nd year. The Program pays for additions conferences if the fellow is presenting on behalf of the division. External pediatric surgical courses during the 2 years include: Colorectal; Oncology, MIS and Essentials of Pediatric Surgery. Educational funds provided to the program via the Office of Education/PGME
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: -1250 +/-
Board passage rate (10 years): 100%
Fellow salary: PGY 6: $88,452.95, PGY 7: $92,848.99 and a Call Stipend $127.60 for in house and $63,80 for home call.
University of Texas Medical Branch / Driscoll Children’s Hospitals Program
Last updated: March 2024
Program website: https://www.utmb.edu/surgery/divisions-sections/pediatric-surgery/welcome
The mission of the UTMB Pediatric Surgery Division is to advance the institution’s tripartite mission of clinical, teaching and research excellence. The goal of the UTMB Medical School is to Build Excellent Scholarship and Service Together (BESST). In addition, UTMB and DCH are committed to serve the Texas Gulf Coast and South Texas Communities. This represents a large, diverse area of the state. As a result, our educational program focuses on preparing fellows with the necessary clinical, educational and research skills to serve these communities.
The Pediatric Surgery Fellowship program will continue that mission by training the pediatric surgery fellow to become an excellent clinical surgeon by offering a robust didactic and clinical experience. In addition, the program will allow the fellow to work closely with the surgery residents in the OR and on the wards to develop the teaching skills of the fellow. Finally, the fellow will be expected to participate in the Division’s research efforts to further develop their research skills. This will allow the fellow to obtain all the skills necessary to become a successful surgeon in any practice environment.
Institution Information
Training Site #1:
The University of Texas Medical Branch (UTMB)
Galveston, TX United States
Number of beds: 42 NICU, 8 PICU, 40 Floor
Percentage of time at this location: 46%
Training site type: Children’s hospital within adult hospital
The University of Texas Medical Branch (UTMB) comprises 4 campuses with the flagship hospital in Galveston, TX. Pediatric Inpatient services are housed in the Galveston and Clear Lake Campuses. The UTMB system has a 43 bed level IV NICU, a 4 bed PICU (with surge capacity for an additional 4 beds), and a 40 bed inpatient floor capacity. There are 163 medical and surgical pediatric specialists at UTMB, providing 24/7 pediatric medical (general and subspecialty), pediatric surgery, orthopedics, pathology, neurosurgery, plastics, radiology and anesthesiology coverage to children. ER services are available 24 hours a day, 7 days a week at all 4 UTMB campuses. Total Operative Experience July 1, 2019-June 30, 2020: 1522 index cases
Training Site #2:
Driscoll Children’s Hospital (DCH)
Corpus Christi, TX United States
Number of beds: 61 NICU, 18 PICU, 110 Floor
Percentage of time at this location: 50%
Training site type: Free standing children’s hospital
Driscoll Children’s Hospital (DCH) is a 189-bed, free-standing, pediatric tertiary care center with more than 30 medical and surgical sub-specialties and over 263 pediatric physicians, providing 24/7 pediatric surgery, cardiac, neurosurgery, orthopedics, pathology, transplant, and plastics services. DCH has an 18 bed PICU and a 61 bed Level IV NICU. Total operative experience: July 1, 2018-June 30, 2020: 5,094 index cases
Training Site #3:
Shriners Hospital for Children – Texas (SHC)
Galveston, TX
Number of beds: 15 ICU. 15 Floor
Percentage of time at this location: 4%
Training site type: Free standing children’s hospital
Shriner’s Hospitals for Children-Galveston (SHC-G) is an ABA and ACS verified Pediatric Burn Center with 15 ICU beds and 15 floor beds. There are 12 faculty physicians dedicated to caring for patients at SHC-G, with additional specialists from UTMB assisting as needed.
Faculty Information
Program Director: Ravi Radhakrishnan, MD, MBA
Associate Program Director: P. Stephen Almond, MD
Program manager: Karley Garcia
kbgarcia@utmb.edu
+1-409-772-5666
Faculty:
Ravi Radhakrishnan, MD, MBA, Program Director, Associate Professor, Program Director
Stephen Almond, MD, Associate Program Director, Clinical Associate Professor
Mohammad Ali Emran, MD, Clinical Associate Professor
Shannon Koehler, MD, PhD, Clinical Assistant Professor
Bindi Naik-Mathuria, MD, MPH, Clinical Associate Professor, Division Chief
Maria "Carmen" Mora, MD Clinical Assistant Professor
Fellow Information
Number of fellows: Two per year
Current fellow(s):
Paul Aylward, MD (start July 2022)
Keyan Mobli, MD (Start July 2023
Previous 5 fellows:
Jonathan DeAntonio, MD (Graduated July 2023)
Curriculum Information
Call Schedule
1st Year – Home Call
2nd Year – Home Call
Conference Schedule
Conference Schedule for UTMB/DCH/SHC Fellowship Program – to be held jointly with UTMB/SHC-Galveston and DCH via virtual platform (Teams, Zoom, etc.)
Tuesday
Time Conference
6:30-7:30am SCORE didactic conference (combined UTMB/DCH)
7:30-8:30am Rotating Conference
Week 1: Radiology, Pathology
Week 2: Radiology, Pathology
Week 3: Combined UTMB/DCH Pediatric Surgery Division M&M
Week 4: Radiology, Pathology or Journal Club (combined UTMB/DCH)
8:30-9:30am Case conference (separate)
Wednesday
7a-8am UTMB Department of Surgery Morbidity and Mortality Conference
8a-9am UTMB Department of Surgery Grand Rounds
10:00-11:10am UTMB Department of Surgery Quality Improvement Conference (fellow will attend while on rotation in Galveston)
Program Information
RRC accreditation status: Initial accreditation
Meeting/Training Course policy: The program will pay for the fellow to attend the following courses:
- Minimally Invasive Surgery Course
- St. Jude Oncology Course
- Pediatric Colorectal and Pelvic Reconstruction Course
- American Pediatric Surgical Association (PGY-6 only)
- American Academy of Pediatrics (PGY-7 only)
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): N/A
Fellow salary: Effective July 1, 2024: PGY-6: $75,574 PGY-7: $78,248
University of Texas Health Science Center at Houston
Last updated: January 2025
Program website: https://med.uth.edu/pediatricsurgery/training/
The Pediatric Surgery Fellowship at McGovern Medical School at The University of Texas Health Science Center at Houston (UTHealth) seeks well-trained, diverse candidates for comprehensive training for a career in pediatric surgery. Our program began in 2005 and has grown in scale and complexity over the years. The fellowship encompasses the entire spectrum of pediatric surgery. Under the direction of 9 pediatric surgery faculty, our trainees have experienced the highest acuity and complexity of neonatal, pediatric, and adolescent conditions. In addition to the broad scope of general pediatric surgery, our fellows are exposed to high-end pediatric surgical subspecialty programs including fetal, oncology, critical care, burns, extracorporeal membrane oxygenation (ECMO), vascular anomalies, short bowel syndrome, chest wall deformities, robotics, trauma, and minimally invasive surgery.
Strengths
- Diverse academic pediatric surgery faculty with subspecialty expertise
- High acuity training environment with 118-bed Level IV NICU and one of the busiest trauma programs in the country
- Broad exposure to general pediatric surgery including acute urologic problems, pediatric and adolescent gynecological conditions, and acute airway and esophageal pathology
- Robust fetal program that provides extensive exposure to congenital anomalies
- Robust critical care/ECMO experience where pediatric surgery runs ECMO
- Integrated pediatric surgical oncology program with MD Anderson Cancer Center that provides the highest level of oncology care
- Primary management of Extra-corporeal life support for all non-cardiac conditions
Weakness
- No transplantation experience
Institution Information
Training Site #1:
Children's Memorial Hermann Hospital
Houston, TX United States
Number of beds: 338
Percentage of time at this location: 90%
Training site type: Children's hospital within adult hospital
Children’s Memorial Hermann Hospital is a 338-bed quaternary care women and children’s hospital located in the Texas Medical Center, the largest medical center in the world. As a primary teaching hospital for the pediatric and obstetrics/gynecology programs at McGovern Medical School at UTHealth, the multidisciplinary team of affiliated doctors, nurses, therapists and other allied healthcare professionals are focused on the personalized needs of women and children. Within the institutions, there is a strong emphasis on quality, education, outcomes, customer service and advanced research. Children’s Memorial Hermann Hospital consists of 76 specialty care rooms in the Women’s Center located one floor below the NICU; 138 pediatric beds including a pediatric intensive care unit (PICU), pediatric specialty care unit (PIMU), general pediatrics area (including medical / surgical care), pediatric observation unit, epilepsy monitoring unit, renal dialysis unit; and 118 neonatal intensive care (NICU) beds, including Level IV NICU provides the highest level of neonatal care including ECMO.
Training Site #2:
MD Anderson Cancer Center
Houston, TX United States
Number of beds: 710
Percentage of time at this location: 10%
Training site type: Children's hospital within adult hospital
In addition to the time spent at Children’s Memorial Hermann Hospital, the primary clinical service includes The University of Texas MD Anderson Children’s Cancer Hospital, which consists of a 35-bed inpatient unit within the MD Anderson Cancer Center that provides inpatient care for pediatric and adolescent patients undergoing treatment for cancer. The Children’s Cancer Hospital is a quaternary referral center for children and adolescents with new diagnoses to advanced cancer that has both a national and international referral base.
Faculty Information
Program Director: KuoJen Tsao, MD
Associate Program Director: Mary Austin, MD, MPH
Program manager: Scottie Wahlstrom
scottie.wahlstrom@uth.tmc.edu
713-500-7300
Faculty:
Mary T. Austin, MD, MPH
Charles S. Cox, Jr., MD
Natalie A. Drucker, MD
Matthew T. Harting, MD, MS
Danielle Hsu, MD
Akemi L. Kawaguchi, MD
Kevin P. Lally, MD, MS
Allison Speer, MD
KuoJen Tsao, MD
Fellow Information
Number of fellows: one per year
Current fellow(s):
Henry Caplan, MD
Jennifer Yonkus, MD
Previous 5 fellows:
Natalie Drucker, MD
2023
University of Texas Health Science Center at Houston
Houston, TX
Mary K. Arbuthnot, DO
2022
Military practice
Naval Medical Center Portsmouth
Portsmouth, Virginia
Alfred Francois Trappey, MD
2021
Military practice
Brooke Army Medical Center
San Antonio, Texas
Megan Coughlin, MD
2020
Riley Children’s Hospital, University of Indiana School of Medicine
Indianapolis, Indiana
Carey Watson, MD
2019
private practice
Fort Wayne, Indiana
Curriculum Information
Call Schedule
1st year: Q3
2nd year: Q3
Conference Schedule
Weekly – Fetal multidisciplinary, Fellows education conference, Morbidity and Mortality Conference
Weekly on rotation – Surgery/Pathology/Radiology/Oncology, NICU walk rounds, Trauma M&M, GI/surgery conference
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The program supports attendance for the St. Jude surgical oncology, colorectal course, APSA meeting (junior fellow), AAP meeting (senior fellow) as well as any additional meetings if the fellows present academic product, subject to RRC regulations governing time in training.
Financial support for candidate interviews: Yes
Average total number of cases performed by graduating fellows over the past 5 years: 1391
Board passage rate (3 years): 100%
Fellow salary: Stipends and fringe benefits are administered through The University of Texas System Medical Foundation. Residents are appointed at stipend levels reflecting their years of prior training.
University of Texas Southwestern Medical Center; Department of Surgery
Last updated: December 2024
Program website: https://www.utsouthwestern.edu/education/medical-school/departments/surgery/divisions/pediatric-surgery/fellowship/
The educational mission of our Pediatric Surgery Fellowship Program at UTSW is to teach pediatric surgical fellows the specialized knowledge and skills needed to manage surgical diseases in children and become competent, thoughtful leaders in academic pediatric surgery. We offer a two-year fellowship training program with a new fellow accepted annually. Our fellows spend most of their time at Children’s Health- Children’s Medical Center of Dallas – the seventh-largest pediatric health care provider in the country, with expansion plans currently underway, and consistently recognized among the top children’s hospitals in the country by U.S. News & World Report.
Our division is dedicated to the education of knowledgeable, independent leaders in academic pediatric surgery. We are committed to fostering and incorporating innovative pediatric surgery treatments and techniques as well as promoting and retaining thoughtful, inquisitive pediatric surgeons to be local and national leaders in academic pediatric surgery. Our fellows are well trained across all aspects of pediatric surgery.
Keys to this training include:
- Robust Multi-disciplinary Clinical Programs– Surgical Oncology, Fetal Evaluation and Treatment Alliance Center/neonatal surgery, Pediatric Intestinal Rehabilitation Program, Surgical Endocrine Program, Center for the Pectus and Chest Wall Anomalies, ACS Level 1 accredited Trauma Program, ECMO program (we perform non-cardiac ECMO), Robotic Surgery, Adolescent Weight Loss Program (including Bariatric Surgery), Transplantation
- Outstanding array of > 50 pediatric specialty and subspecialty programs including national experts in pediatric Hematology/Oncology, Neonatology, Cardiology, Cardiac Surgery including transplant, Endocrinology, GI (ERCP, endoscopic intervention and endoscopic US), Nephrology, Intervention Radiology, Pathology, Neurology, Neurosurgery, Orthopedics, Pulmonology, and Urology to name a few.
- One of the busiest pediatric emergency medicineprograms in the country with an annual volume of ~170,000 patients with 20-40% of all hospital admission coming through the ED.
- Robust Educational Curriculum– learn from experts in surgery and other disciplines at regularly scheduled conferences: Grand rounds, Mortality and Morbidity Conference, Journal Club, Pediatric Surgery in Review (utilizing Score curriculum and NAT), SurgRadPath Conference, Oncology Review, Fetal conference, Fetal Journal Club, Professor Rounds, Multidisciplinary Combo Conferences (fetal, NICU, PICU, ECMO, GI, urology) and pediatric tumor boards (solid tumor, thyroid, musculoskeletal tumor board).
- Surgical Simulation center– We utilize fresh tissue and inanimate models to teach advanced minimally invasive neonatal surgical techniques with faculty proctors.
- Mentorship:Through our mentorship program, we coach our fellows to identify specific career goals and encourage clinical, educational, research, and leadership opportunities to further develop unique expertise.
- Research Opportunities: Our faculty are involved in clinical, translation, and basic science research including multi-center national trials, drug/device trails, local clinical trials, prospective registries, retrospective/prospective reviews, and bench research. Fellows participate in research most fitting with their career goals and clinic interest.
Institution Information
Training Site #1
Children’s Health – Children’s Medical Center of Dallas
Dallas, TX United States
Number of beds: 490
Percentage of time at this location: 98%
Training site type: Free standing children’s hospital
Children’s Health – Children’s Medical Center Dallas is a 490-bed hospital with a level 1 trauma center with a large level IV NICU, a PICU, a cardiac ICU, and an active ECMO program. In an average year, the pediatric surgery service performs more than 4,000 cases, sees more than 5,000 outpatients, and is primarily responsible for more than 1,000 injured trauma patients. The surgical team consists of pediatric surgery fellows, PGY 4 surgical residents, surgical interns, medical students, ~10 nurse practitioners/PAs, and multiple wound ostomy nurses. Our NPs are in house 7 days a week for both trauma and general surgery. Radiology, IR, and ECHO is available 24-7. PICC team is available 7 days a week.
Training Site #2
Parkland Memorial Hospital
Dallas, TX United States
Number of beds: 96 NICU and Special Care Nursery beds
Training site type: Other
With over 12,000 deliveries and over 1,400 neonatal discharges per year, Parkland provides an excellent clinical experience for surgical conditions affecting neonates. Located across the street from Children’s, these patients are managed cooperatively with the Surgical and Neonatology teams. Patients deemed to need complex surgical intervention are transferred over to Children’s Health for the surgical procedure and acute post-surgical care. Throughout the year, the fellows see and manage complex neonates perioperatively at Parkland and our first-year fellow rotates to Parkland during the NICU rotation.
Pediatric Surgical faculty from UT Southwestern see, evaluate, and manage patients cooperatively with the UT Southwestern Neonatologists at Texas Health Regional Hospital. For neonatal index cases beneficial to their education, the fellows evaluate and treat neonates at THR. This additional NICU augments the fellows experience at Children's Health Dallas for the management of complex neonatal index cases.
Faculty Information
Program Director: Diana Diesen, MD
Associate Program Director: Samir Pandya, MD
Program manager:
Rachel Howell
Rachel.howell@utsouthwestern.edu
214-648-9576
Faculty:
Barbara Gaines, MD, FACS – Professor and Chief of the Division of Pediatric Surgery
Diana Diesen, MD, BS -- Associate Professor; Pediatric Surgery Fellowship Program Director
Samir Pandya, MD – Professor, Associate Pediatric Surgery Fellowship Program Director
Faisal Qureshi, MD, MBA -- Professor, Director Adolescent Surgical Weight Loss Program
Stephen Megison, MD, BS -- Professor, Medical Director of Trauma Services and Robotic Surgery
Joseph Murphy, MD, MS – Professor, Minnie Stevens Piper Professor
Mark Ryan, MD, MSPH -- Assistant Professor, Associate Medical Director of Trauma Services
Natasha Corbitt, MD, PhD – Assistant Professor, Director of Hepatobiliary Program
Lauren Gillory, MD – Assistant Professor, Director Pediatric Trauma at Children’s Health Plano; Pediatric NSQIP Champion
Charles Hong, MD – Assistant Professor, Director of Pediatric Colorectal Program
Adam Alder, MD -- Associate Professor, Director of the Center for Pectus and Chest Wall Anomalies, Medical Director of Clinical Operations Children's Health, Plano
Nathalie Brewer, MD -- Assistant Professor
Dai Chung, MD, MBA -- Professor and Strauss Chair, Pediatric Surgery; Executive Vice Chair, Department of Surgery, UTSW; Chief Medical Officer & Surgeon-in-Chief, Children’s Health
Laura Purcell, MD, MPH – Assistant Professor
Russell Hawkins, MD, MS – Assistant Professor
Carrie Moore, MD, MS, PhD – Assistant Professor
Fellow Information
Number of fellows: one per year
Current fellow(s):
Hallie Quiroz, MD
Amanda Louiselle, MD
Previous 5 fellows:
Laura Purcell, MD, MPH
2022-2024
Assistant Professor, Pediatric Surgery at UT Southwestern Medical Center
Dallas, TX
Kristin Gee, MD
2021-2023
Pediatric Surgeon at Mission Health Hospital
Ashville, NC
Sarah Cairo, MD, MPH
2020-2022
Assistant Professor, Pediatric Surgery at University of California San Francisco Benioff Children’s Hospital
San Francisco, CA
Aaron Scott, MD
2019-2021
Assistant Professor, Pediatric Surgery at St. Joseph’s Children’s Hospital
Tampa, FL
Jessica Zagory, MD
2018-2020
Assistant Professor, Department of Surgery, Division of Pediatric Surgery,
Associate Program Director, General Surgery Residency, Louisiana State University Health Sciences Center
New Orleans, LA
Curriculum Information
Block Schedule
*Updated Block Diagram below
Call Schedule
Q4-Q6
Conference Schedule
Updated Conference Schedule below
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course:
- First year – Colorectal course, APSA conference, plus additional meetings if fellow is presenting substantive work.
- Second year – AAP conference, Surgical Oncology Review course, plus additional meetings if fellow is presenting substantive work.
Average total number of cases performed by graduating fellows over the past 5 years: 1289-1470
Board passage rate (3 years): 100%
Fellow salary:
First year fellow: $83,617
Second year fellow: $88,055
University of Toronto/The Hospital for Sick Children
Last updated: September 2023
Program website: http://www.sickkids.ca/GeneralSurgery
We are among the oldest pediatric surgical training programs in North America, having trained over 135 pediatric surgeons. The Hospital for Sick Children is the largest pediatric health sciences centre in Canada and one of the largest and most reputable in the world. It is affiliated with the Department of Surgery at the University of Toronto which was recently ranked 2nd among the top departments of surgery in the world (US News & World Report). We are dedicated to improving the health of children by providing the best in family-centered care, creating ground breaking scientific and clinical advances and in training the next generation of experts in pediatric subspecialties. SickKids is made up of more than 13,000 staff, students and volunteers. The recently built Peter Gilgan Centre for Research and Learning is yet another example of our world class commitment to research and education. Project HORIZON will see a staged complete overhaul of the two city blocks that constitutes SickKids
Institution Information
The Hospital for Sick Children
Toronto, ON Canada
Number of beds: 350
Percentage of time at this location: 95%
Training site type: Free standing children’s hospital
We are among the oldest pediatric surgical training programs in North America, having trained over 135 pediatric surgeons. The Hospital for Sick Children is the largest pediatric health sciences centre in Canada and one of the largest and most reputable in the world. It is affiliated with the Department of Surgery at the University of Toronto which was recently ranked 2nd among the top departments of surgery in the world (US News & World Report). We are dedicated to improving the health of children by providing the best in family-centered care, creating ground breaking scientific and clinical advances and in training the next generation of experts in pediatric subspecialties. SickKids is made up of more than 13,000 staff, students and volunteers. The recently built Peter Gilgan Centre for Research and Learning is yet another example of our world class commitment to research and education.
Humber River Hospital
Toronto, ON Canada
Number of beds: 656
Percentage of time at this location: 5%
Training site type: Children’s hospital within adult hospital
This large general hospital in the north part of Toronto serves as a location for patients with garden variety pediatric surgical problems over one year of age to be assessed and operated upon. Most cases are done as outpatients though there is a rarely used option for overnight admission. This site provides excellent surgical care for common pediatric surgical problems and ensures our trainees exposure to the bread and butter of pediatric surgery. It is also the site where our trainees have achieved the greatest exposure to upper GI endoscopy.
Faculty Information
Program Director: Georges Azzie, MD
Program manager: Shannon Hannah
shannon.hannah@sickkids.ca
Faculty:
Georges Azzie, MD
Priscilla Chiu, MD
Annie Fecteau, MD
Sharifa Himidan, MD
Jacob Langer, MD
Agostino Pierro, MD
Mercedes Pilkington, MD
Joshua Ramjist, MD
Rodrigo Romao, MD
Saurabh Saluja, MD
Blayne Sayed, MD
Kasper Wang, MD
Augusto Zani, MD
Fellow Information
Number of fellows: 5
Current fellow(s):
Lorenzo Anez-Bustillos, MD
Sam Han, MD
Previous 5 fellows:
Benjamin Carr, MD
2023
Joshua Ramjist, MD
2023
Assistant Professor, Department of Surgery, University of Toronto
Aodhnait Fahy, MD
2022
Assistant Professor, Department of Surgery, Penn State
Kaitlyn Wong, MD
2021
Assistant Professor, Department of Surgery, UMass Chan Medical School
Eric Sparks, MD
2021
Assistant Professor, Department of Surgery, The University of Alabama at Birmingham
Curriculum Information
Block Schedule
-22 months of pediatric surgery
-1 month NICU rotation
-1 month PICU rotation
Call Schedule
1st year: Q5 in-house
2nd year: Q5 in-house
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The program pays for Transition to Fellowship Boot Camp, one course and APSA in the first year, one course and AAP in the second year. The program pays for additional meetings if the fellow is presenting on behalf of the division.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1000 +/-
Board passage rate (3 years): 90+%
Fellow salary: PGY6: $89,337.48, PGY7: $92,767.48. There is also a stipend of $132.67 (weekday) and $145.94 (weekend) for every call shift
University of Utah/Primary Children’s Hospital
Last updated: December 2024
Program website: https://medicine.utah.edu/surgery/pediatric-surgery/message-from-program-director.php
Primary Children’s Hospital serves an encatchment area that includes Utah, Wyoming, Idaho, Montana, and Nevada. Our program therefore provides our fellow with a broad-based experience encompassing both common and unusual pediatric surgical conditions. Infants and children from this large geographic area seek tertiary and quaternary care principally at Primary Children’s. This results in our fellows having extensive experience in the perioperative and operative care of children with complex conditions. This is reflected in their operative case logs which we routinely share with applicants for our fellowship. We believe that excellent training in pediatric surgery must be based upon exposure to a high volume of infants and children with complex problems.
The faculty has chosen to be a single-fellow program despite this large patient volume to assure that emphasis of the fellowship is educational. This allows our trainee to engage in complex neonatal operations from the first day of fellowship. It also allows the fellow to choose the cases which are most educational and to direct the service for the entire training period. Care of the large number of operative patients with a small continent of trainees is successful because we have a large group of well-trained pediatric surgical, advanced practice clinicians.
The faculty includes 10 surgeons each of whom has an individual focus area of clinical practice and academic. This facilitates our ability to develop the level of expertise expected at a referral center. Multispecialty clinics led by our surgeons include: fetal treatment center, colorectal center, inflammatory bowel disease center and esophageal airway center. We are a level 1 trauma center and lead statewide pediatric trauma network. Additionally, some of our surgeons are recognized as national leaders in oncology. All of the surgeons care for the full range of neonatal and childhood surgical diseases so the fellow receives training in multiple approaches. Members of our faculty actively participate in the leadership of national organizations.
Our Division and Fellowship are characterized by Western spirit of hard work and comradery. Our goal is to bring our fellow into the circle of surgeon who genuinely enjoy working together to care for children and their families. We are fortunate to live and work in a place where others go for vacations year-round.
Our ideal candidate brings strong training in general surgery and a desire to be a leader in the future of pediatric surgery. We recognize that there are various roles these leaders may take in the future. In short, we are looking for fellows who love surgery and want to make an impact.
Institution Information
Primary Children’s Hospital
Salt Lake City, UT United States
Number of beds: 289
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Faculty Information
Program Director: Brian T. Bucher, MD
brian.bucher@hsc.utah.edu
Associate Program Director:
Program manager: Carly Arellano
carly.arellano@hsc.utah.edu
(801)662-2989
Faculty:
Douglas C. Barnhart, MD
Lauren M. Baumann, MD
Brian T. Bucher, MD
Stephen J. Fenton, MD
Zachary J. Kastenberg, MD
Michael D. Rollins, MD
Katie W. Russell, MD
Eric R. Scaife, MD
Scott S. Short, MD
David E. Skarda, MD
Robert A. Swendiman, MD
Maren E. Shipe, MD
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Michael D. Traynor, MD
Previous 5 fellows:
Robert A. Swendiman, MD
2021-2023
Elisabeth K. Wynne, MD
2019-2021
Pediatric Surgeon, Attending Dayton Children’s Hospital
Dayton, Ohio
Zachary J. Kastenberg, MD
2017-2019
Pediatric Surgeon, Assistant Professor, University of Utah School of Medicine/Primary Children’s Hospital
Salt Lake City, Utah
Scott S. Short, MD
2015-2017
Pediatric Surgeon, Assistant Professor, University of Utah School of Medicine/Primary Children’s Hospital
Salt Lake City, Utah
Justin H. Lee, MD
2013-2015
Pediatric Surgeon, Attending Phoenix Children’s Hospital
Phoenix, Arizona
Mark S. Molitor, MD
2011-2013
Pediatric Surgeon, Attending Phoenix Children’s Hospital
Phoenix, Arizona
Curriculum Information
Call Schedule
1st Year – Every other Saturday
2nd Year – Every other Saturday
Conference Schedule
Conferences consist of a combination of Interesting Case Conference, Faculty Didactic, Research Conference and NICU Conferences.
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Our fellow routinely attends APSA in the first year and AAP in the second year. Additionally, our fellow attends 2-3 offsite courses during the fellowship. These have typically included the colorectal and oncology course. The fellow may attend additional meetings to foster development of particular academic or clinical interest. Time away is subject to RRC regulations governing time in training.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1862
Board passage rate (3 years): 100%
Fellow salary: PGY6 - $87, 436
PGY7 - $89,857
Additional call pay compensation
University of Washington/Seattle Children’s Pediatric Surgery Fellowship
Last updated: December 2024
Program website: https://www.seattlechildrens.org/healthcare-professionals/education/residency-fellowships/pediatric-fellowships/pediatric-surgery-fellowship/
This fellowship covers the entire spectrum of pediatric surgery, with a high volume of neonatal, oncologic, thoracic, gastrointestinal, and minimally invasive surgery cases. Fellows are expected to attend clinic and become familiar with the outpatient aspects of pediatric surgery. Our fellows gain extensive experience in caring for critically ill infants in the Neonatal Intensive Care Unit (NICU) the Pediatric Intensive Care Unit (PICU), and the Cardiac Intensive Care Unit (CICU). The Pediatric Surgery Fellowship was established in 1967 and benefits from the expertise of dedicated teachers who enjoy mentorship and sharing their knowledge.
This is a busy clinical fellowship covering the broad spectrum of pediatric surgery. Emphasis is on the pre-, post- and intraoperative management of pediatric surgical patients from the prenatal phase to age 21. Fellows receive extensive experience in the surgery of congenital malformations, oncology, minimally invasive procedures and routine pediatric cases. They manage all patients on the pediatric surgery service with attending supervision, including patients in the NICU, PICU and on the surgical wards. Clinical experience includes 1-month rotations in the NICU (at both University of Washington and Seattle Children’s) and on the trauma service at Harborview Medical Center.
Strengths
- Breadth of surgical experience
- Breadth of care (pre/post op, ICU, ED, ward)
- Large geographic catchment area
- Neonatal surgery
- Faculty involvement
- Multidisciplinary specialty clinics (colorectal, aerodigestive, intestinal failure, IBD, CDH)
- Simulation program
- Ambulatory surgical experience (at Bellevue satellite facility)
Weaknesses
- No cardiac surgery rotation,
- Foreign body call staffed by ENT
Institution Information
Training Site #1:
Seattle Children’s Hospital
Seattle, WA United States
Number of beds: 407
Percentage of time at this location: 95%
Training site type: Free standing children’s hospital
Training Site #2:
Harborview Medical Center
Seattle, WA
Number of beds: 413
Percentage of time at this location: 5%
Training site type: Other
Faculty Information
Program Director: Patrick J. Javid, MD
Associate Program Director: Caitlin Smith, MD
Program manager:
Jessica Mattheis
Jessica/mattheis@seattlechildrens.org
206-987-1177
Faculty:
Steven Lee, MD – Professor, Division Chief
Patrick Javid, MD –Professor, Program Director
Jeff Avansino, MD –Professor
Matthew Dellinger, MD, MPH – Assistant Professor
Adam Goldin, MD, MPH –Professor
Sarah Greenberg, MD –Assistant Professor
Patrick Healey, MD –Professor
John Meehan, MD – Associate Professor
Samuel Rice-Townsend, MD – Associate Professor
Kimberly Riehle, MD – Associate Professor
David Rothstein, MD, MS - Professor
Robert Sawin, MD – Professor Emeritus
Caitlin Smith, MD – Associate Professor
Rebecca Stark, MD – Associate Professor
John Waldhausen, MD – Professor Emeritus
Fellow Information
Number of fellows: 2 (1 per year)
Current fellow(s):
Alan Utria, MD
Mark Barry, MD
Previous 5 fellows:
Guy Jensen, MD, MPH
Children's Hospital Colorado/University of Colorado
Hira Ahmad, MD
2021-2023
Children’s Hospital of Orange County
Jamie Anderson, MD
2020-2022
Assistant Professor, University of California - Davis
Matthew Dellinger, MD, MPH
2019-2021
Assistant Professor, University of Washington, Seattle Children’s Hospital
Marko Rojnica, MD
2018-2020
Assistant Professor, University of Illinois-Chicago
Sarah Greenberg, MD, MPH
2017-2019
Assistant Professor, University of Washington, Seattle Children’s Hospital
Caitlin Smith, MD
2015-2017
Assistant Professor, University of Washington, Seattle Children’s Hospital
Curriculum Information
Block Schedule
1st year fellow: one month rotations in NICU (October) and Harborview Medical Center for trauma (April), all other months at Seattle Children’s
2nd year fellow: 12 months at Seattle Children’s
Call Schedule
1st year: Home call split with senior fellow. Three research fellows take primary call one night per week each, and one weekend per month each. On these days, the fellow is on backup call.
2nd year: Home call split with junior fellow. Three research fellows take primary call one night per week each, and one weekend per month each. On these days, the fellow is on backup call.
Attending surgeon presence in house all day, and on call within 20 minutes at night.
APPs participate in Floor care 7 days per week, and ICU care 5 days per week.
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Yes
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1184
Board passage rate (3 years): 100%
Fellow salary: Junior fellow: $87,768; Senior fellow: $93,096
UPMC Children's Hospital of Pittsburgh
Last updated: December 2024
Program website: https://www.chp.edu/health-care-professionals/education/fellowships/pediatric-surgery/surgery
General overview statement that might include the following:
Description of type of candidate program seeks -
Demonstrate appropriate oversight of the pediatric surgery service, both on the general wards and in the various intensive care units.
Participate in the emergency and outpatient evaluation of infants and children with surgical disease and trauma. Participation in all phases of care including the pre-operative and post-operative evaluation as well as in-hospital course is required.
Develop the technical skills required for complex surgical procedures in infants and children. Residents will be facile with advanced techniques in laparoscopy, thoracoscopy, and endoscopy, as well as open surgical procedures.
Understand the multi-disciplinary nature of today’s medical environment and effectively work with all members of the patient care team to achieve the best outcome for the patient.
Be an active participant in the educational process, both during the residency and beyond. Residents are to consult the literature and perform self-study during the training, as well as participate in scholarly activities.
Strengths: The goal of the advanced residency training in Pediatric Surgery at UPMC Children’s Hospital of Pittsburgh is to develop the specialized knowledge and skills required to care for surgical disease in infants and children. At the conclusion of the two-year training program, residents will be competent pediatric surgeons, qualified for certification in Pediatric Surgery by the American Board of Surgery, and able to assume responsibility for the pre-operative, operative, and post-operative management of surgical problems in infants and children. During the training program, residents will demonstrate mastery of the six competencies set forth by the Accreditation Council of Medical Education (ACGME) and be afforded increased responsibility and independence according to their skill.
Weaknesses: n/a
Institution Information
UPMC Children’s Hospital of Pittsburgh
One Children’s Way
4401 Penn Avenue
Pittsburgh, PA 15224
Number of beds: 313
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Faculty Information
Program Director: Kevin P. Mollen, MD, Associate Professor of Surgery
Associate Program Director: Paul K. Waltz, MD, Assistant Professor of Surgery
Program manager: Pat Fustich
patricia.fustich@chp.edu
412-692-8735
Faculty:
Kelly M. Austin, MD — Associate Professor of Surgery
Geoff Bond, MBBS — Assistant Professor of Surgery
Serena Chan, MD – Assistant Professor of Pediatric and Adolescent Gynecology
Courtney Crain, MD – Clinical Professor
George K. Gittes, MD — Professor and Division Chief
Devin Halleran, MD - Assistant Professor of Surgery
Marcus M. Malek, MD — Assistant Professor of Surgery
Kevin P. Mollen, MD — Assistant Professor of Surgery
Michael J. Morowitz, MD — Professor of Surgery
Carolina Pinzon-Guzman, MD - Assistant Professor of Surgery
Ward Richardson, MD — Assistant Professor of Surgery
Stefan Scholz, MD — Assistant Professor of Surgery
Paul Waltz, MD – Assistant Professor of Surgery
Fellow Information
Number of fellows: one per year
Current fellow(s):
Anghela Z. Paredes, MD, Chief Fellow
Amelia Collings, MD, Junior Fellow
Previous 5 fellows:
2024
Kathryn Tinsley Anderson, MD, Assistant Professor University of Illinois
2023
Charles R. Hong, MD, Assistant Professor, University of Texas, Southwestern
2022
Bryanna M. Emr, MD, Assistant Professor, Penn State Health Children's Hospital
2021
Joseph C. Fusco, MD, Assistant Professor of Pediatric Surgery at Vanderbilt University Medical Center
2020
Paul K. Waltz, MD, Assistant Professor of Surgery, UPMC Children’s Hospital of Pittsburgh
Curriculum Information
Block schedule: n/a
Conference Schedule: Academic Morning – weekly didactic training session, attendance required.
Program Information
RRC accreditation status:
Initial Accreditation - yes
Continued Accreditation - yes
Meeting/Training Course policy (Does program pay for courses or meetings?): Two to three per year.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): 100%
Fellow salary: PGY6 $79,831; PGY7 $82,625; PGY8 $85,517
Vanderbilt University Medical Center/Monroe Carell Jr. Children's Hospital - Pediatric Surgery
Last updated: October 2023
Program website: https://www.vumc.org/pedssurgdept/residencyfellowship-education
Program Brochure: Click Here
It offers one position annually through the National Residency Match Program (NMRP).The Department of Pediatric Surgery promotes excellence in the comprehensive surgical care of children. Our unified group of pediatric surgeons is committed to the practice and teaching of excellence in clinical care. This includes both clinical outcomes and basic laboratory research and the education of pediatric surgery residents, general surgery and pediatric residents, medical students, and nursing students.
Our department and hospital offer an excellent opportunity for the clinical and academic training of future pediatric surgeons. These future surgeons will develop a unique expertise in the clinical approach to the surgical problems of childhood, as well as a critical and analytical approach to the evidence-based practice of pediatric surgery.
The program is an ACGME accredited two-year subspecialty program.
Institution Information
Training Site #1:
Monroe Carell Jr. Children’s Hospital at Vanderbilt
Nashville, TN United States
Number of beds: 343
Percentage of time at this location: 100%
Training site type: Free standing children’s hospital
Vanderbilt Children’s Hospital by the Numbers • Total Inpatient Beds: 343 • Emergency Department Rooms: 42 (including 2 trauma bays and 7 fast track bays) • Operating Rooms: 18 (onsite) • Inpatient Discharges: 16,232 • Clinic Visits: 360,314 • ER Visits: 47,446 • The only Level 1-designated Trauma Unit and dedicated Burn Unit in the region • The only Level 4-designated Neonatal Intensive Care Unit in the region • More than 400 physicians trained in 30 pediatric and surgical specialties • 10th Floor Expansion opened in June 2019 (Pediatric Heart Institute – 38 beds) • 11th Floor Expansion opened in March 2020 (NICU, Cardiology and Transplant – 38 beds)
Faculty Information
Program Director: Harold N. Lovvorn, III, MD
Associate Program Director: Eunice Y. Huang, MD
Program manager: Christine Hamby
christine.hamby@vumc.org
615-936-1612
Faculty:
Eunice Y. Huang, MD – Professor of Pediatric Surgery, Associate Program Director
Jeffrey Upperman, MD — Department Chair and SIC
Harold N. Lovvorn, III, MD — Professor of Pediatric Surgery, Program Director
Walter Morgan, MD — Assistant Professor of Pediatric Surgery
Melissa Danko, MD — Assistant Professor of Pediatric Surgery
Gretchen Jackson, MD, PhD — Associate Professor of Pediatric Surgery
Irving Zamora, MD — Assistant Professor of Pediatric Surgery
Monica Lopez, MD – Associate Professor of Pediatric Surgery
Joseph Fusco, MD — Assistant Professor of Pediatric Surgery
Jamie Robinson, MD – Assistant Professor of Pediatric Surgery
Margaret Gallagher, MD – Assistant Professor of Pediatric Surgery
Kevin Johnson, MD – Assistant Professor of Pediatric Surgery
Fellow Information
Number of fellows: 2 per year (Recruits 1 new candidate per year)
Current fellow(s):
Maren E. Shipe, MD, Senior
Roshan D'Cruz, MD, Junior
Previous 5 fellows:
Laura L. Stafman, 2021 – 2023 – Graduate (Univ of Alabama at Birmingham/Children’s of Alabama) MD
Jacob K. Olson, 2020 – 2022 – Graduate (Riley Children’s Health) MD
Laura Y. Martin, 2019 – 2021 – Graduate (NYU Langone Health) MD
Lauren A. Gillory, 2018 – 2020 – Graduate (UT Southwestern Medical Center) MD
Margaret Gallagher – 2017 – 2019 – Graduate (Brooke Army Medical Center) MD
Curriculum Information
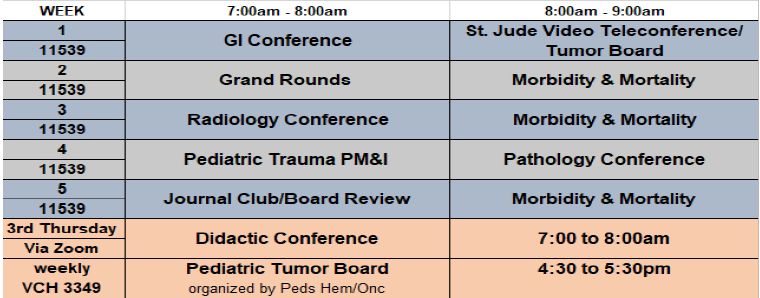
Call Schedule
1st year: In house call average every 5th night
2nd year: In house call average every 5th night
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: Program pays for 3 to 4 meetings during the 2 year fellowship
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: N/A
Board passage rate (3 years): 100%
Fellow salary: PGY 6 – 77,873.00; PGY 7 – 81,377.00
Washington University School of Medicine/St. Louis Children's Hospital Pediatric Surgery Fellowship
Last updated: September 2023
Program Name: Washington University School of Medicine Pediatric Surgery Program Fellowship
Program Location:
Children’s Hospital
Suite 6110, Mail Stop 8235-0049-06
Once Children’s Place
St. Louis, MO 63110
Program website: https://pediatricsurgery.wustl.edu/education/
Overview of Fellowship:
The Division of Pediatric Surgery offers a two-year fellowship program for physicians seeking specialized training in pediatric surgery.
In order to be eligible for the program, applicants must first complete a general surgery residency program that has been approved by the Accreditation Council for Graduate Medical Education (ACGME). One applicant is selected for the two-year fellowship each year. He or she is based at St. Louis Children’s Hospital, where the Division of Pediatric Surgery averages approximately 1,750 surgical admissions and 9,500 inpatient days per year. In addition to clinical duties, the fellow has administrative responsibilities for residents in general surgery and pediatrics as well as for medical students on the service.
The fellow’s clinical responsibilities include the preoperative, operative and postoperative care of patients on the pediatric surgical service. He or she develops detailed knowledge of congenital, neoplastic, infectious and other acquired conditions of the gastrointestinal tract and of other abdominal organs, the diaphragm and thorax, endocrine glands, gonads and reproductive organs, head and neck, and blood and vascular system.
The fellow develops expertise in treating the following conditions:
- Major disease processes(congenital anomalies of the thorax and gastrointestinal tract, tracheoesophageal fistula, intestinal atresia, malrotation, anorectal malformation, inperforate anus and abdominal wall defects)
- Gastrointestinal problems(esophageal disorders, gastroesophageal reflux, hypertrophic pyloric stenosis, Meckel’s diverticulum, intestinal duplication, intussusception, necrotizing enterocolitis, appendicitis, Hirschsprung’s disease, inflammatory bowel disease, hepatobiliary problems and diseases of the pancreas)
- Abdominal wall abnormalities(gastroschisis, omphalocele, hernias and hydroceles)
- Undescended testes and ambiguous genitalia
- Pediatric oncology(Wilms’ tumor, neuroblastoma, pheochromocytoma, soft tissue sarcomas, germ cell tumors, lymphomas and Hodgkin’s disease)
- Head and neck masses(lymphadenopathy, congenital lesions of the neck, and thyroid and parathyroid disorders)
- Extracorporeal membrane oxygenation (ECMO)for pediatric and neonatal disease
The fellow also gains knowledge and experience in treating pediatric trauma and burn patients. This trauma care includes the management of cases where children have sustained injuries to multiple organs. The fellow not only provides surgical treatment of these patients, but also manages these patients in a nonoperative setting.
The fellowship includes rotations on the pediatric intensive care unit, neonatal intensive care unit, urology and otolaryngology services as well as outpatient and other areas.
The fellowship’s broad curriculum encompasses the electrolyte and nutritional needs of neonates and pediatric patients as well as the basic principles of cardiothoracic surgery, gynecology, neurologic surgery, orthopedic surgery, otolaryngology, anesthesia, vascular surgery and transplant surgery.
Fellows participate in a series of conferences — both didactic and bedside — that also are attended by the house staff and medical students. The fellow helps prepare for grand rounds and other conferences.
Strengths
- Large volume of solid tumor cases
- Large volume neonatal cases
- Strong support for academic career development
Weaknesses
- No coordinated sharing of foreign body cases.
- No coordinated sharing of ovarian cases.
Institution Information
Children’s Hospital
One Children’s Place, St. Louis, MO 63110
Number of beds: SLCH has 455 licensed beds, which includes 77 pediatric intensive care beds, a 150-bed newborn intensive care unit, and a 16-bed pediatric bone marrow transplant unit.
Percentage of time at this location: 100%
Training site type: Children’s Hospital part of the Washington University/BJH/Children’s Consortium
- Louis Children’s Hospital (SLCH) serves the health care needs of children, from infancy to adolescence, and advocates on behalf of children and families.
- Founded in 1879, SLCH is the oldest pediatric hospital west of the Mississippi River and the 7th oldest in the United States.
- Each year the hospital receives about 275,000 patient visits, and the school of medicine receives about 150,000 patient visits.
- Louis Children's Hospital is nationally ranked in the top 12 percent of Children’s Hospitals by U.S. News & World Report, which in 2021 ranked the hospital in all 10 specialties surveyed for the 13th consecutive year.
- Physicians at SLCH are faculty at Washington University School of Medicine (WUSM), ranked as one of the top medical schools in the nation by U.S. News & World Report.
Faculty Information
Program Director: Patrick Dillon, MD
Associate Program Director: Brad Warner, MD
Program Manager: Katie Fuhs
fuhs@wustl.edu
Office: 314-362-8028
Faculty:
Andrew Yeh, MD Assistant Professor
Jacqueline Saito, MD, MSCI Associate Professor
Jesse Vrecenak, MD Assistant Professor
Brad Warner, MD Professor of Pediatric Surgery
Colin Martin, Surgeon in Chief, Division of Pediatric Surgery
Fellow Information
Number of fellows: one per year, 2 year fellowship
Current fellow(s):
Kristen Seiler, MD
Michelle Kallis, MD
Previous 5 fellows:
Paul McGaha
2023
Oklahoma Children’s Hospital
Andrew Yeh
2022
Washington University School of Medicine
Ryan Antiel
2021
Duke Children’s Hospital and Health Center
Nicole Wilson
2020
University of Rochester Surgical Associates
Baddhr Shakhsheer
2019
Assistant Professor of Surgery, Comer Children’s Hospital (Chicago)
Curriculum Information
Block Schedule
Call Schedule
Click Here
Conference Schedule
Click Here
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: The program pays for one meeting and one course per year plus additional meetings if the fellow is presenting their own work.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1,094
Fellow salary:
Current Stipend PGY 6 $80,426
Current Stipend PGY 7 $84,047
Yale University
Last updated: 10/4/2024
Program website: https://medicine.yale.edu/surgery/education/fellowships/pediatric-surgery/
The Division of Pediatric Surgery at Yale University has been training Pediatric Surgery Fellows since 1994. Our Program matches one Fellow every other year. The overall goals of the Fellowship Program are to train academic pediatric surgeons and to provide the Fellow with a broad education in clinical Pediatric Surgery. The Program seeks superbly trained general surgery residents or graduates of general surgery residency programs who are adult learners and self-motivated. The Program uses a vaired and broad case mix, personal mentoring by Faculty, specialty-specific and multidisciplinary didactic conferences, as well as national courses to educate Fellows. The relatively small group of six (6) Faculty results in a closely-knit group and opportunity for one-on-one teaching.
Institution Information
Yale-New Haven Children’s Hospital
New Haven, CT United States
Number of beds: 221
Percentage of time at this location: 100%
Training site type: Children’s hospital within adult hospital
Faculty Information
Program Director: Robert A. Cowles, MD
Associate Program Director: N/A
Program manager: Sema Webb
sema.webb@yale.edu
203-785-2701 op. 3
Fax 203-785-3820
Faculty:
Michael G. Caty, MD, MMM — Professor, Division Chief, Surgeon-in-Chief
Robert A. Cowles, MD —Professor, Program Director
Emily R. Christison-Lagay, MD — Associate Professor
David H. Stitelman, MD — Associate Professor
Daniel G. Solomon, MD — Assistant Professor
Matthew A. Hornick, MD – Assistant Professor
Robert J. Touloukian, MD — Emeritus Professor
Fellow Information
Number of fellows: one every other year
Current fellow(s):
Matthew Shaughnessy 2023-2025
Previous 5 fellows:
Barbara Coons
2023
NYU Grossman School of Medicine
New York, New York
Saurabh Saluja, MD
2021
Sydney Children’s Hospital, Randwick
New South Wales, Australia
David J. Worhunsky, MD
2019
Assistant Professor, University of Kentucky
Lexington, KY
Muriel A. Cleary, MD
2017
Assistant Professor, University of Massachusetts
Worchester, MA
Gustavo A. Villalona, MD
2015
Wolfson Children’s Hospital
Jacksonville, FL
Curriculum Information
Call Schedule
1st Year - Home
Q22nd Year - Home
Q2
Conference Schedule
Attending Rounds - Daily
Teaching/Curriculum Conference – Weekly
Fetal Diagnosis and Treatment Conference – Weekly
Tumor Board – Weekly
Radiology/Pathology/Surgery Conference – Monthly
QI Conference – Monthly
Trauma Conference – Monthly
Surgery/GI Conference – Monthly
ECMO Conference – Quarterly
Program Information
RRC accreditation status: Continued Accreditation
Meeting/Training Course policy: One course and one meeting will be paid per year. Fellows also have a “professional development fund” that can be used for travel and currently is $1400.
Financial support for candidate interviews: No
Average total number of cases performed by graduating fellows over the past 5 years: 1340
Board passage rate (3 years): 100%
Fellow salary: Changes yearly