CONDITIONS P - Z
These pages offer explanations of pediatric medical surgical conditions including:
- what the condition is
- signs and symptoms
- how it is diagnosed
- treatment
- home care
- long-term outcomes
Use it as a reference when discussing your child’s individual condition and treatment with your doctor and medical professionals.
Pancreas Divisum
Condition: Pancreas Divisum
Overview (“what is it?”)
- The pancreas is an organ that sits behind the stomach and secretes chemicals (called enzymes) that help in digestion.
- Pancreas divisum is a congenital (meaning present at birth) pancreatic abnormality in which two parts of the pancreas fail to come together while the baby is developing inside the uterus (Figure 1). The digestive juice that the pancreas makes drain into the intestine through a tubular structure. Because of the failure of the pancreas to fuse, the duct does not drain the digestive juice effectively. The opening of the main pancreatic duct is narrowed.
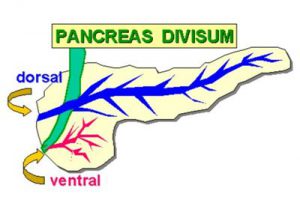 Figure 1
Figure 1
- The number of people affected is unclear but it is believed to be present in as many as 5 to 10% of people.
- Pancreas divisum is sometimes associated with choledochal cysts or intestinal malrotation. These are congenital abnormalities of the gallbladder and intestines that occur during development.
Signs and Symptoms (“What symptoms will my child have?”)
- The majority of individuals born with pancreas divisum experience no symptoms throughout life. These individuals will remain undiagnosed and do not require treatment. Approximately 5% of people will develop symptoms.
- Common symptoms include:
- Abdominal bloating and/or pain which is usually in the mid-abdomen (middle area of the upper belly) and sometimes radiates to the back
- Jaundice (or yellowing of the skin)
- Nausea
- Food intolerance
- Recurrent episodes of pancreatitis (inflammation of the pancreas)
Diagnosis (“What tests are done to find out what my child has?”)
- The diagnosis of pancreas divisum is usually made by endoscopic retrograde cholangiopancreatography also known as an ERCP. ERCP is a special test where your child is sedated so that a flexible camera (called an EGD – esophagogastroduodenoscopy) can be inserted through the mouth down to the level of the pancreas to visualize the anatomy of the ducts (Figure 2).
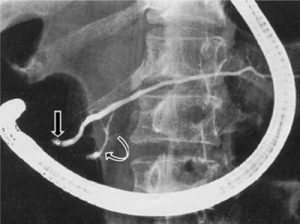 Figure 2
Figure 2
- Magnetic resonance cholangiopancreatography (MRCP) has also been used successfully. It is an MRI scan specific for the pancreas
- MRI (Magnetic Resonance Imaging)—uses a magnet, radio waves and computer to obtain images of organs in the body. MRI does not use radiation.
- This often requires some sedation for infants and young children
- Other tests that are occasionally done are abdominal ultrasounds, CT scans, amylase and lipase (blood tests for the pancreas function).
Treatment (“What will be done to make my child better?”)
- Endoscopic sphincteroplasty: The goal of endoscopic (flexible tube-like camera inserted into the intestines) therapy is to relieve the obstruction of the ducts that drain fluid from the pancreas to the intestines.This is done by enlarging or cutting the opening (sphincter) that will allow the pancreatic juice to drain into the intestines.
- Preoperative preparation depends on the condition of the child. If your child is dehydrated, has a bacterial blood infection (cholangitis), or currently suffering from inflammation of the pancreas, then these conditions need to be taken care of prior to the procedure (fluids, antibiotics, pancreatic rest)
- Postoperative care: Your child will recover in a monitored surgical ward, and the length of the hospital stay depends upon the child’s age, preprocedural condition and postprocedural complications.
- Risks: Immediate complications are injury to the esophagus, stomach or intestines, bleeding, infection and pancreatitis (inflammation of the pancreas).
- Benefits: Ability of pancreas to drain pancreatic juice effectively, relief of symptoms and recurrent pancreatitis
Home Care (“What do I need to do once my child goes home?”)
- Diet: No dietary restrictions are necessary, and children are often allowed to resume their normal diet. If the child is recovering from pancreatitis, a low fat diet may be suggested.
- Activity: No activity restrictions apply. Your physician will give you specific instructions.
- Medicines: Mild pain relievers may be needed for the first days.
- What to call the doctor for
- Fevers, vomiting or food intolerance, or yellowing of the skin or eyes
- Worsening belly pain
- Follow-up care: Appointments may be frequent for the first month, and further endoscopic procedures may be necessary.Your physician will give you specific instructions for follow up.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Long-term results are dependent upon the procedure performed and associated abnormalities. Most patients have excellent long term results.
References
- Holcomb. G, and Murphy. P. Ashcraft’s Pediatric Surgery 5th Edition 2010, Elsevier.
- Madura JA, Fiore AC, O’Connor KW, et al. Pancreas divisum. Detection and management. American Surgery 1985; 51:353.
- O’Neill JA: Surgical management of recurrent pancreatitis in children with pancreas divisum. Annals of Surgery 231:899-908, 2000.
- http://pathology.jhu.edu/pc/BasicOverview1.php?area=ba.
- Figure-1-ERCP-showing-type-1classic-pancreatic-Divisum-with-major-dorsal-duct-opening.
Updated: 11/2016
Author: Romeo C. Ingacio, Jr., MD; L. Prescher, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Pancreatic Cysts
Condition: Pancreatic Cysts (pseudocyst, fluid collections, duplication cyst)
Overview (“What is it?”)
- The pancreas is a gland located in the abdomen surrounded by the stomach, small intestine, liver, spleen and gallbladder (see Figure 1). The pancreas is a gland that aids in two bodily functions—digestion and blood sugar regulation.
- Pancreatic cysts are collections of fluid that can be due to congenital (someone is born with it) or acquired (something that developed after birth) conditions. Pancreatic cysts are classified based on the underlying cause of the fluid collection.
- Pancreatic cysts are often classified into congenital and developmental, retention, enteric duplication and pseudocysts. The first three types of cysts are rare.
- Congenital and developmental cysts may be detected on prenatal ultrasound. These cysts may be associated with cysts in other areas of the body.
- Retention cysts are a result of blockage of a portion of the gland downstream causing a back-up of fluid.
- Duplications of the gastrointestinal (enteric) system may involve the pancreas and lead to cyst formation. Duplication cysts are abnormal portions of the intestine. In this location, there may be duplication of the pancreas or duplication of an organ next to the pancreas.
- The most common cause of a pancreatic fluid collection is a pseudocyst. This type of fluid collection is a result of inflammation of the pancreas (pancreatitis) or trauma to the pancreas. The fluid leaks from the injured pancreatic ducts and collects in areas next to the pancreas. Over time, a capsule forms around this fluid collection becoming a pseudocyst.
 Figure 1
Figure 1
Signs and Symptoms (“What symptoms will my child have?”)
- Congenital/developmental cysts or enteric duplications may be seen on prenatal ultrasound. Early signs of cysts may be feeling of fullness or bloating and early satiety or decreased appetite. A history of pancreatitis or pancreatic trauma may be an early indication that a pseudocyst may form.
- Later signs/symptoms include pain and discomfort due to the cyst. A mass may be detected on physical exam if the cyst becomes large. Patients may also develop jaundice, persistent vomiting, weight loss and fluid within the abdomen.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: The most common lab tests include a serum amylase and lipase as well as liver function tests (bilirubin, alkaline phosphatase, GGT, AST, ALT). In many cases, all or most of these labs will be normal.
- Diagnosis is usually first made with ultrasound.
- Once the diagnosis is made with ultrasound, additional imaging with CT scan or MRI maybe obtained to provide more detailed anatomic information about the cyst.
- Conditions that mimic this condition include other cystic lesions in nearby organs (adrenal gland, duodenum, stomach, etc.).
Treatment (“What will be done to make my child better?”)
- There are really no medications that can be used to treat pancreatic cysts. Some pancreatic fluid collections that develop after trauma or pancreatitis may resolve over time. Medications may be required to treat complications associated with pancreatic cysts (i.e. antibiotics if the cyst becomes infected).
- Surgery is the main treatment for pancreatic cysts.
- Preoperative preparation: Patients will usually have preoperative labs and imaging (see above). Patients will often require blood to be available during surgery. Children will not be able to eat the morning of surgery.
- Postoperative care: Most patients will not be allowed to eat or drink immediately after surgery. This will allow for everything to heal on the inside. Many patients will have a tube in place to keep the stomach empty. This tube is usually inserted through the nose and into the stomach while the patient is asleep under anesthesia. Some patients may have a drain in place after surgery. Most of the time, the drain is removed prior to going home. However, in some instances the drain may be left in place to collect additional fluid. If this is the case, parents will be given careful instruction on how to care for the drain. In most instances, when children are discharged from the hospital, they are eating normally and require minimal additional care.
- Risks/Benefits: The standard risks of surgery include bleeding, blood transfusion, infection, anesthetic risks, damage to surrounding structures, leakage from the pancreas and recurrent fluid collections. The benefit of surgery is to relieve symptoms and to prevent future complications associated with the pancreatic cysts (infection, bleeding, etc.).
Home Care (“What do I need to do once my child goes home?”)
- Diet: In most cases, a regular diet
- Activity: No heavy activity for 4-6 weeks for an open operation and 2-4 weeks for a laparoscopic operation
- Wound care: None, unless a drain is still in place
- Medicines: Pain medicine for a couple of days
- What to call the doctor for: Fever greater than 101⁰ F or 38⁰C, persistent vomiting, wound problems (redness or drainage), or worsening pain.
- Follow-up care: With your surgeon 1-2 weeks after discharge.
Long-Term Outcomes (“Are there future conditions to worry about?”)
In most cases, surgical excision or drainage of the cyst will be curative.
Updated: 11/2016
Author: Steven L. Lee, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Pancreatitis
Condition: Pancreatitis in children
Overview (“What is it?”)
- The pancreas is a gland located in the abdomen surrounded by the stomach, small intestine, liver, spleen and gallbladder. The pancreas is a gland that aids in two bodily functions—digestion and blood sugar regulation. The pancreatic duct is a tube that runs the length of the pancreas and carries pancreatic enzymes and other secretions made by the pancreas, often called “pancreatic juice”. This pancreatic duct connects with the common bile duct, which carries bile from the gallbladder. These two ducts drain bile and pancreatic juice to into the small intestine, where these substances aid with the breakdown of food. The hormones that regulate blood sugar (insulin and glucagon) are released into the blood stream rather than the intestine.
- Definition: Pancreatitis is a disease in which the pancreas becomes inflamed from a number of different causes. Pancreatic damage occurs when enzymes in the pancreatic juice are activated before they are released into the small intestine and begin attacking the pancreas. Acute pancreatitis is a sudden inflammation that ranges from mild to severe. It can be life threatening.
- Most children with acute pancreatitis recover completely with appropriate treatment. In severe cases, acute pancreatitis can result in bleeding into the gland, infection and cyst formation. Patients with severe acute pancreatitis may also suffer problems in other organs such at the kidneys, lungs and heart. Common causes of acute pancreatitis in children include injury (such as handlebar injuries from a bicycle), gallstones which lodge in the opening of the pancreatic duct, certain medications (some anti-seizure medications, or drugs used to treat cancer) or congenital problems of how ducts of the pancreas formed during fetal development.
- Chronic pancreatitis is a slow, progressive illness of the pancreas in which the ability of the pancreas to produce pancreatic juices and the sugar controlling hormones becomes altered. Children at risk for chronic pancreatitis are those with specific genetic, metabolic or anatomic abnormalities.
Signs and Symptoms (“What symptoms will my child have?”)
Common symptoms of pancreatitis include abdominal and back pain, nausea and vomiting. These symptoms are not limited to pancreatitis and can easily be confused with signs of another disease. Patients with chronic pancreatitis may experience weight loss, diarrhea and oily bowel movements, poor growth and diabetes.
Diagnosis (“What tests are done to find out what my child has?”)
- There is no single test to diagnose pancreatitis. The rapid onset of upper mid-abdominal pain with nausea and vomiting may prompt your doctor to obtain blood tests to see if there is evidence of pancreatitis. Testing the blood for substances that the pancreas makes (amylase and lipase) is used most commonly. When the pancreas is injured or inflamed, the blood levels of these pancreatic enzymes can rise above normal. If these blood tests are abnormal, an ultrasound or CT scans are commonly obtained to look for evidence of pancreatitis. However, all of these tests may be falsely normal in the setting of pancreatitis, and repeated vigilance on the behalf of the medical team may be required to ultimately make the diagnosis.
- Blood tests may be used to determine if the pancreatitis is improving, and imaging such as another CT scan or an MRI may be used if there is suspicion of ongoing damage to the pancreas, development of a cyst (called a pseudocyst), or to try and determine if abnormal anatomy of the pancreatic duct system is the cause of the pancreatitis.
Treatment (“What will be done to make my child better?”)
- Acute pancreatitis typically resolves within 2-7 days with appropriate intravenous fluid, pain control and nutritional support. In the past, patients were prevented from eating to allow the pancreas to rest (“bowel rest”), but today your doctor will decide what is safe—either limited oral intake, using nutrition delivered through a special tube placed through the nose (a nasojejunal tube), or nutrition given through the vein in severe cases. In cases of severe vomiting, the stomach may need to be suctioned to empty it out. This is done through a tube inserted through the nose with the end in the stomach. If the stomach is empty, then the vomiting usually stops, making the child more comfortable. Supporting other organ systems is important and may require admission to the intensive care unit so that the lungs, kidneys and heart can be supported with modern medical interventions when necessary.
- A surgeon may be involved in caring for your child as there is always a small chance that an operation or procedure may be necessary, but this is uncommon to treat the pancreas itself. However, in some cases, surgery may be necessary to treat the cause of the pancreatitis. For instance, when pancreatitis occurs as the result of gallstones, removal of the gallbladder is often recommended once the pancreatitis has resolved. This is typically done with an operation called a laparoscopic cholecystectomy in which the gallbladder is removed using small incisions. In patients with pancreatitis from trauma, a pediatric surgeon will likely care for your child to determine if surgery is necessary to remove a part of the damaged pancreas. Also, a surgeon may be helpful in cases where complications happen as the result of severe pancreatitis such as a pancreatic cyst or bleeding.
- The treatment of chronic pancreatitis largely depends on the cause. If there is problem with the anatomy of the duct system that drains the pancreas, then a procedure may be needed. This is often performed by endoscopy whereby a scope is inserted into the mouth that reaches the pancreatic duct opening in the intestine (endoscopy) under anesthesia. Surgery may be required if this is unsuccessful or is unavailable.
- Patients who have lost the ability to digest food will be prescribed pills containing pancreatic enzymes and special vitamins to aid in digestion. There is no clear evidence that a special diet is required for chronic pancreatitis, however many doctors will advise low-fat diet and more frequent, smaller meals. Currently, there are no effective medical treatments for patients with a genetic predisposition, however some patients are candidates for a newer operation called pancreatectomy with islet cell autotransplantion that is offered in some specialized medical centers. In this procedure, the surgeon removes the pancreas and the hormone-producing cells known as ‘islets’ are isolated and returned to the patient, usually by injecting them into the liver.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- When the symptoms are mild and the patient is able to drink enough liquids and be comfortable with oral pain medication, your child may not need to be treated in the hospital. When your child is hospitalized, even though symptoms of acute pancreatitis may last for a few days, it does not mean that your child needs to stay in the hospital that entire time.
- The complications of acute pancreatitis depend on how bad the inflammation was. The most common complication is the collection of fluid around the pancreas, which, in many cases, will resolve with time. If the pockets of fluid become infected or get really big, then a procedure may be necessary. This may include drainage of infected fluid or surgery.
- Death from acute pancreatitis is quite rare in children. Pancreatitis can recur in 10% of patients and patients who have recurrent episodes will likely benefit from further testing to determine the underlying cause.
Updated: 11/2016
Author: Casey M. Calkins, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Parathyroid Problems
Condition: Parathyroid problems in children
Overview (“What is it?”)
- Parathyroid glands are small organs of the endocrine system that are located in the neck behind the thyroid. Parathyroid glands (we all generally have four of them) are normally the size of a pea (or even smaller). These glands control the calcium in our bodies by making a hormone called parathyroid hormone or “PTH”. PTH controls the level of calcium and phosphorus—minerals that are bones but also circulates in the blood. PTH controls how much calcium is lost in the urine (by its effects on the kidneys) and works with vitamin D to control how much calcium we absorb from our food.
- Our bodies very carefully regulate calcium because it is important in many of the body’s functions. If the parathyroid glands make too much or too little hormone, it disrupts this delicate balance. If the glands do not make enough PTH, then you have hypoparathyroidism. More commonly, diseases of the parathyroid gland result in hyperparathyroidism—where your body is making too much PTH and the blood calcium rises. Too much calcium in the blood is called hypercalcemia. Although the thyroid and parathyroid glands are neighbors and are part of the endocrine system, the thyroid and parathyroid glands are not unrelated—they just have similar names. Parathyroid problems in children are less common in children compared to adults.
- Definition
- Hypoparathyroidism: Not enough PTH and low blood calcium levels is most commonly caused by injury during an operation of the parathyroid glands—but it only happens in 1-2% of those patients. Some children are born without parathyroid glands, or glands that cannot make enough PTH such as DiGeorge syndrome. Although DiGeorge syndrome may affect one baby out of every 2,000 births, not all of those children will suffer from hypoparathyroidism.
- Hyperparathyroidism: Too much PTH and high body calcium can be caused by a number of problems, but there are two general types.
- In primary hyperparathyroidism, an enlargement of one or more of the parathyroid glands causes too much PTH to be made and therefore high calcium in the blood. The chance of primary hyperparathyroidism in a child is less than 5 in 100,000. The most common cause of primary hyperparathyroidism is a benign (non-cancerous growth) tumor on a single parathyroid gland that makes it overactive. Sometimes, extra hormone is made from all four parathyroid glands being bigger than normal. Cancer of the parathyroid glands is very uncommon, but usually causes symptoms that are also due to high blood calcium levels.
- Secondary hyperparathyroidism occurs as a result of another disease that initially causes low levels of calcium in the body which this causes the parathyroid glands to make lots of PTH in an effort to increase blood calcium levels. Over time, this may cause hypercalcemia. Chronic kidney failure is the most common cause of secondary hyperparathyroidism as the kidneys have lost the ability to retain enough calcium in the body.
Signs and Symptoms (“What symptoms will my child have?”)
- Hypoparathyroidism: In mild cases, there may be no symptoms at all. When symptoms are seen, they are usually vague. Health care professionals call these symptoms “nonspecific”. These include feeling tired, irritable, depressed or anxious. When calcium levels drop very low, the patient may experience muscle or abdominal pain, tingling of the fingers, toes or face, numbness around the mouth, twitching of the face muscles, headaches, brittle nails, dry skin and hair, and uncontrolled spasms that cause muscle cramps. When calcium levels fall very fast or are extremely low, patients may experience seizures.
- Hyperparathyroidism: Like hypoparathyroidism, mild cases of hyperparathyroidism may cause no symptoms. When symptoms are seen, they are also vague and many are very similar to having low calcium levels. In mild cases these include muscle weakness, feeling tired, weak or depressed or muscle pain. In severe cases the patient may experience back or flank pain from kidney stones, belly pain, troubles concentrating, personality changes, memory problems, constipation or broken bones.
Diagnosis (“What tests are done to find out what my child has?”)
- Doctors usually diagnose a parathyroid problem after finding an abnormal level of calcium on a blood test when a child has some of the symptoms noted previously. It is especially important to tell the doctor about other family members that may have had similar calcium or parathyroid problems in the past. If the child was healthy before the onset of symptoms, then high calcium is almost always due to primary hyperparathyroidism. To narrow down why there is too much calcium in the blood, your doctor may also obtain other blood tests to look at the level of other elements in your body such as phosphorous, alkaline phosphate and the PTH level.
- The doctor may also order a test of the urine to see if the high blood calcium levels are due to a kidney problem.
- A special X-ray called “bone densitometry” is more commonly done in adults to see if the parathyroid problem has caused damage to the bones. This test is not performed commonly in children because a child’s bones are still growing and adapting, and the results of that X-ray test are unreliable in kids.
- The most common reason why the parathyroid gland works too hard is overgrowth of a single parathyroid gland called an “adenoma”. An adenoma is a benign (non-cancerous) growth that only causes a problem because it makes too much parathyroid hormone. Less commonly, one or more glands just get too large, which is called parathyroid hyperplasia. To see if there is evidence of an adenoma, the doctor may order a Sestamibi scan. Sestamibi is a very safe liquid radioactive compound that is absorbed by the overactive parathyroid but not by the healthy ones. The compound is injected through a small IV and then a special X-ray machine called a gamma camera is used to try and identify the abnormal parathyroid gland(s). This test is performed to locate which gland or glands may be abnormal to plan for treatment.
Treatment (“What will be done to make my child better?”)
- Patients with low blood calcium (hypoparathyroidism) are treated with medicine to replace calcium to keep the blood levels normal. These medicines include calcium and vitamin D (Calcitrol®), both of which can be given by mouth to maintain a normal level of calcium circulating in the body. Currently, giving a patient a drug that mimics PTH is not practical or effective. There is no surgical treatment for hypocalcemia.
- Hyperparathyroidism
- Medical Management: Although researchers continue to try and find medicines for the treatment of primary hyperparathyroidism, there are no medicines are currently available that can block the overproduction or PTH. In patients with secondary hyperparathyroidism that occurs with chronic kidney problems, medicine is available to try and treat the problem, and surgery is typically used as a last resort. For the rare patient who has severe hypercalcemia that has resulted in a seizure or other life-threatening problems, immediate admission to the hospital for intensive therapy with IV fluids and other medicines to bring the calcium level down to a lower level is required prior to considering any type of surgery.
- Surgical Treatment: The standard and most effective treatment for primary hyperparathyroidism is to remove the parathyroid tissue that is overproducing PTH—typically a single adenoma. The Sestamibi scan helps the surgeon to determine which gland(s) is abnormal and allows him or her to focus the operation on removal of the overactive gland(s). This operation is done under general anesthesia though a small incision (1-2 inches) in the neck. The surgeon identifies the abnormal gland and removes it. Many surgeons confirm that the gland in question is the only problem gland prior to closing the incision by using a blood test, while the patient is still under anesthesia, to make sure the PTH level has dropped to a more normal level after the gland has been removed. Since PTH doesn’t last for very long in the body, once the surgeon takes the gland out, the PTH level should drop to a normal level within 20-30 minutes.
- Risks from parathyroid surgery include temporary low blood calcium levels while the other normal parathyroid glands left behind regain their ability to make PTH. In modern surgery where the surgeon removes the adenoma and doesn’t “explore” the other glands, this may last a few days, and is generally treated with oral calcium supplements until it gets better. Risk of damage to a nerve that is close to the parathyroid glands (recurrent laryngeal nerve) is low (1%). If the nerve is injured, it typically regains function, but if the nerve is permanently damaged it can cause permanent hoarseness. This is very rare in the hands of a surgeon with considerable experience in parathyroid surgery.
- Benefits: Removing the overactive gland resolves the symptoms of high calcium. Bones are stronger.The results of surgery are generally excellent, with more than 99% of patients being “cured” of the disease, and in the vast majority of cases there is little risk of the high calcium levels returning because of disease of another parathyroid.
- Postoperative care: The operation may require an overnight stay just to ensure that the patient doesn’t exhibit any symptoms that would require more aggressive therapy for the temporary low calcium levels.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Usually the child can be on a regular diet appropriate for age when he or she goes home.
- Activity: Regular activity can resume slowly a few days after surgery.
- Wound care: Specific wound care issues should be addressed with your child’s surgeon. Usually wounds are kept dry for about three days, then the child may shower. Soaking the wound (such as baths or swimming) should wait until a week after surgery.
- Medicines
- Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- If your child has persistent low calcium levels, he or she will need calcium supplements.
- What to call the doctor for: Call to the surgeon if there is worry about infection (unexplained fevers, redness and drainage of the wound). If your child experiences numbness and/or tingling around the fingers and the face, you should call the surgeon or endocrinologist as well.
- Follow-up care: A wound check is often performed 2-3 weeks after surgery. Often, the child’s oncologist can also provide follow up of the wound as well.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Future outcomes for hypercalcemia secondary to hyperparathyroidism is excellent.
Updated: 11/2016
Author and Editor: Marjorie J. Arca, MD
Patent Ductus Arteriosus
Condition: Patent Ductus Arteriosus (PDA)
Overview (“What is it?”)
- Definition: The ductus arteriosus is a connection between the aorta (large blood vessel that carries blood to the entire body) and the pulmonary artery (blood vessel that carries blood to the lungs). This is a structure that is very important while the baby is developing inside the mother, because through it, the mother provides oxygen to the baby. When the baby is born, the baby starts breathing and the ductus arteriosus is not needed anymore. Normally it closes on its own after birth. Sometimes, especially in premature babies, the ductus stays open (“patent”)—thus, the condition is named “patent ductus arteriosus” (PDA). Blood that is supposed to go to the body will instead go to the lungs. This situation can cause too much blood to go to the lungs, requiring the baby to remain on the ventilator for a long time.
- Epidemiology: Happens in 7-38% premature babies
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs
- Murmur heard on exam
- Needs oxygen
- Blood pressure changes
- Later signs/symptoms
- Congestive heart failure—heart needs to work harder and over time, it may not be able to keep up
- Need to be on the ventilator a long time
- Murmur heard on exam in older kids
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests
- Exam: Murmur heard with stethoscope
- Chest X-ray: Findings of an enlarged heart or fluid in the lungs
- Echo (ultrasound of the heart) shows the presence and size of the PDA and the flow of blood in PDA
- Conditions that mimic this condition
- Lung disease due to prematurity (bronchopulmonary dysplasia)
- These babies will also have lung problems requiring ventilator but no murmur or PDA seen on echo.
- Lung disease due to prematurity (bronchopulmonary dysplasia)
Treatment (“What will be done to make my child better?”)
- Medicine
- There are medicines that can be given to help close the ductus. Indomethacin and acetaminophen are two of these medications.
- Risk of indomethacin includes association with intestinal perforation, bleeding and kidney abnormality.
- There are medicines that can be given to help close the ductus. Indomethacin and acetaminophen are two of these medications.
- Surgery
- Surgery is the only option if the baby fails medical therapy or if complications happen because of the medicines given to close the ductus.
- Procedure
- Can be done in the operating room or in the neonatal intensive care unit (NICU)
- Left thoracotomy (incision on side of left chest between ribs)
- Place clip on PDA to close it
- Older children can have PDA closed by placement of coils in PDA by accessing it using catheters through the artery in the groin (transcatheter coil embolization).
- Preoperative preparation: Antibiotics are given by vein to decrease risk of infection.
- Postoperative care
- Chest X-ray after surgery
- Supportive care (fluids, possible blood pressure medication, ventilator, pain medication) after surgery. It will take some time for the baby to recover from surgery and get used to new blood circulation.
- A small tube may be placed in the chest cavity after the surgery to drain extra air and fluid. This will be removed a few days after the operation.
- Risks
- Bleeding
- Damage to lung (low)
- Damage to nerve (recurrent laryngeal nerve) which can affect vocal cord on left side. Voice is preserved, but may have swallowing problems.
- Death (low incidence but can happen due to bleeding)
- Benefits
- Improve baby’s lungs and may help baby to get off the ventilator
- Improve blood flow to intestines and rest of body
- Improve heart function
Home Care (“What do I need to do once my child goes home?”)
- Diet: Formula or breast milk appropriate for the baby
- Activity: By the time baby goes home, activity should be normal
- Wound care: Incision on chest can be washed with soap and water.
- Medicines: Nothing particular to this condition
- What to call the doctor for: Redness, warmth, drainage from incision, fever, problems breathing
- Follow-up care: The surgeon usually sees baby two weeks after surgery (if baby is still in hospital, the surgeon will usually see baby while still in hospital)
Long-Term Outcomes (“Are there future conditions to worry about?”)
No significant long-term outcomes except that the titanium clip (if used) will always be visible on chest X-ray (but will not go off in metal detectors or have problems with MRIs).
Updated: 11/2016
Author: Grace Mak, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Pectus Carinatum
Condition: Pectus Carinatum (pigeon chest)
Overview (“What is it?”)
- Pectus carinatum is a condition where the bones of the chest did not develop as they should. The chest cage is made up of the center breast bone (sternum) in the front, the ribs (made of bone and cartilage, with the cartilage connecting the ribs to the breast bone), and the spine in the back. In pectus carinatum, the breast bone is pushed out. One side of the chest may be more affected giving an uneven look
- Epidemiology: More common in males than females. It can get worse with age, especially during growth spurts.
- Etiology (cause): Some people think that the cartilaginous ribs grow unevenly, pushing the breastbone outward. Sometimes it can be seen members of the same family. Pectus carinatum can also be seen in children who had cardiac surgery as babies, with incisions in the breast bone.
Signs and Symptoms (“What symptoms will my child have?”)
- Pectus carinatum abnormalities range from barely noticeable to severe.
- Early symptoms: The outward appearance of the chest is something that the child and parents can see.
- Late symptoms: On occasion, there may be trouble breathing or irregular heart rate, but these are rare. Sometimes there may be pain the area of the chest.
- Associated problems: Children with pectus carinatum may have scoliosis (abnormal curve of the spine). Some may also have connective tissue problems.
Diagnosis (“What tests are done to see what my child has?”)
- Chest X-ray: May initially be done to look at the general appearance of the breast bone, ribs and spine.
- Computed tomography (CT) of chest: Detailed pictures of the chest are taken, reconstructed in different views to get a better picture of the chest. This shows the doctor how bad the pectus is—mild, moderate or severe.
- Echocardiography: Ultrasound of the heart to look at flows and function. This is not done routinely, but may be ordered if there is concern about heart function.
- Lung function tests: Testing how strong the lungs are. Again, not all patients need this; your doctor will decide whether your child requires this study.
Treatment (“What will be done to make my child get better?)
- Medical management—BRACING: There is no medicine that can make pectus carinatum better. However, if the pectus carinatum is mild to moderate, the use of a custom-fitted chest wall brace has good results.
- The brace is constructed to fit your child’s chest.
- As the child grows, the contour of the chest changes. The brace will need to be changed.
- THE BRACE WILL ONLY WORK IF THE CHILD WEARS IT. The child should wear it as much as possible (greater than 20 hours a day, if possible).
- Every six months, there is follow up with your surgeon
- Surgery: For severe pectus carinatum with symptoms, surgery may be considered. Surgery is usually delayed until middle teenager years.
- Ravitch Procedure: The goal of the surgery is to straighten out the breast bone. The cartilaginous ribs are removed from their connection to the breast bone. The breast bone may have to be fractured before it can be straightened out, and a strut may be placed as the breast bone heals. Drains are placed under the muscle and skin to collect fluid.
- Preoperative preparation: The child is asked to shower or bathe the night before or the morning of surgery. He or she should not eat anything solid for at least eight hours before surgery.
- Postoperative care: The child is admitted to the hospital for several days. Pain control is achieved using epidural anesthesia, patient controlled analgesia (PCA), nerve cryoablation, oral pain medications.
- Pain medications can be given by mouth or through the vein. These may include acetaminophen (Tylenol®), ketorolac or ibuprofen, as well as narcotics.
- PCA: Patient controls when pain medication is given. A syringe of pain medication is connected to the patient’s IV. Based on the patient’s weight, a safe dose of narcotic is given each time patient pushes a button.
- Epidural: A long thin catheter is placed in the spine around the spinal cord. Pain medications are injected through this route, which the patient may also be able to control with a button.
- Gradual activity is directed by the surgical, nursing, and physical therapy teams.
- In a Ravitch procedure, drains to collect fluid after surgery will be removed before discharge
- Ravitch Procedure: The goal of the surgery is to straighten out the breast bone. The cartilaginous ribs are removed from their connection to the breast bone. The breast bone may have to be fractured before it can be straightened out, and a strut may be placed as the breast bone heals. Drains are placed under the muscle and skin to collect fluid.
- Risks: Bleeding, infection, pain
- Benefits: The chest wall is straightened out.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Most patients are able to eat a general diet.
- Activity: Ask your surgeon for specific recommendations. It is generally recommended to limit activity, especially those that twist the body or use the arm significantly (golf, tennis, swimming), for at least six months after surgery. Vigorous activity may dislodge the bar, and the patient would need another operation.
- Wound care: The patient can shower in three days but may want to wait seven days after surgery before soaking the wound. If drains are still present, do not wet the drains.
- Medicines: Medication for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain. Constipation is a very common problem after this surgery.
- What to call the doctor for: Problems that may indicate infection such as fevers, wound redness and drainage should be addressed. If the patient feels at any time that the strut has moved or there is chest pain, call the doctor.
- Follow-up care: The patient should be seen by the surgeon a few weeks after surgery to check on the wound, the shape of the chest, and/or placement of the strut. These strut is removed a few months after surgery..
Long-Term Outcomes
The normal shape of the chest is maintained in majority of children after the Ravitch operation.
Updated: 11/2016
Author and editor: Marjorie J. Arca, MD
Pectus Excavatum
Condition: Pectus Excavatum (sunken chest, funnel chest)
Overview (“What is it?”)
- Pectus excavatum is a condition where the bones of the chest did not develop as they should. The chest cage is made up of the center breast bone (sternum) in the front, the ribs (made of bone and cartilage, with the cartilage connecting the ribs to the breast bone), and the spine in the back. In pectus excavatum, the breast bone appears sunken or hollowed out. Sometimes the ribs are also malformed and do not appear even.
- Pectus excavatum means hollowed chest.
- Epidemiology: It occurs in 1 in 400 births.
- Etiology (cause): Sometimes the child may have been born with a pectus. It may get worse with age. Some people think that the cartilaginous ribs grow unevenly, pushing down the breastbone. Some patients with problems of bones and cartilage (Marfan’s syndrome) can have a higher risk of pectus excavatum.
 Figure 1: Pectus excavatum. Picture courtesy of MJArca 12/2016
Figure 1: Pectus excavatum. Picture courtesy of MJArca 12/2016
Signs and Symptoms (“What symptoms will my child have?”)
- Early symptoms: A hollow appearance of the breast bone, asymmetry of the ribs and the lower edges of the ribs.
- Late symptoms: Worsening deformity. Occasionally may have problems breathing during exertion. Occasionally, pectus may cause breathing troubles or heart issues.
Diagnosis (“What tests are done to see what my child has?”)
- Computed tomography (CT) of chest: Detailed pictures of the chest are taken, reconstructed in different views to get a better picture of the chest. This shows the doctor how bad the pectus is—mild, moderate, or severe.
- Echocardiography: Ultrasound of the heart to look at flows and function. This is not done routinely, but may be ordered if there is concern about heart function.
- Lung function tests: Testing how strong the lungs are. Again, not all patients need this; your doctor will decide whether your child requires this study.
Treatment (“What will be done to make my child get better?)
- Medical management: There is no medicine that can make pectus excavatum better. However, if the pectus excavatum is mild, exercises can make the chest muscles stronger. Being more conscious of having a good posture is also very helpful.
- Surgery: For moderate or severe pectus with symptoms, surgery may be considered. Surgery is usually delayed until middle teenager years. This can be done using two approaches.
-
 Nuss Procedure: A steel bar is used to push out the breast bone. The bar stays in the chest for two to three years.
Nuss Procedure: A steel bar is used to push out the breast bone. The bar stays in the chest for two to three years. - Ravitch Procedure: The cartilaginous ribs are removed from their connection to the breast bone. The breast bone may have to be fractured before it can be straightened out, and a strut may be placed as the breast bone heals.
- Preoperative preparation: The child is asked to shower or bathe the night before or the morning of surgery. He or she should not eat anything solid for at least eight hours before surgery.
- Postoperative care: The child is admitted to the hospital for several days. Pain control is achieved using epidural anesthesia, patient controlled analgesia (PCA), nerve cryoablation, oral pain medications
- Epidural: A long thin catheter is placed in the spine around the spinal cord. Pain medications are injected through this route, which the patient may also be able to control with a button.
- PCA: Patient controls when pain medication is given. A syringe of pain medication is connected to the patient’s IV. Based on the patient’s weight, a safe dose of narcotic is given each time patient pushes a button.
- Nerve cryoablation: This method is available in certain centers where the nerves by the ribs are frozen. There is numbness in the area around where the incisions and the bar are located. This method is currently only available for the Nuss procedure.
- Pain medications can be given by mouth or through the vein. These may include acetaminophen (Tylenol®), ketorolac or ibuprofen, as well as narcotics.
- Gradual activity is directed by the surgical, nursing and physical therapy teams.
- In a Ravitch procedure, drains to collect fluid after surgery will be removed before discharge.
- Risks: Bleeding, infection, pain. If the patient has Nuss procedure, the bar can get dislodged.
- Benefits: The chest wall is straightened out.
-
Home Care (“What do I need to do once my child goes home?”)
- Diet: Most patients are able to eat a general diet.
- Activity: Ask your surgeon for specific recommendations. It is generally recommended to limit activity, especially those that twist the body or use the arm significantly (golf, tennis, swimming), for at least six months after surgery. Vigorous activity may dislodge the bar, and the patient would need another operation.
- Wound care: The patient can shower in three days but may want to wait 5-7 days after surgery before soaking the wound.
- Medicines: Medication for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain. Constipation is a very common problem after this surgery.
- What to call the doctor for: Problems that may indicate infection such as fevers, wound redness and drainage should be addressed. If the patient feels at any time that the bar has moved or there is chest pain, call the doctor.
- Follow-up care: The patient should be seen by the surgeon a few weeks after surgery to check on the wound, the shape of the chest, and/or placement of the bar. These visits will continue until the bar is removed in 2-3 years. If a Ravitch procedure is done, the strut may be removed sooner.
Long-Term Outcomes (“Are there future conditions to worry about?”)
The normal shape of the chest is maintained in majority of children after the Ravitch or Nuss procedure.
Updated: 11/2016
Author and editor: Marjorie J. Arca, MD
Rectal Prolapse
Condition: Rectal Prolapse
Overview (“What is it?”)
The rectum is the end of the large intestine (also known as the colon) where stool travels before it exits outside through the anus.
- Rectal prolapse is condition where a portion or all of the rectum (the end of the colon) protrudes through the anus and can be seen on the outside of the body. (See Figure 2)
 Figure 2: Infant with rectal prolapse. (Pictures provided by Dr. Romeo C. Ignacio, Naval Medical Center San Diego, California)
Figure 2: Infant with rectal prolapse. (Pictures provided by Dr. Romeo C. Ignacio, Naval Medical Center San Diego, California)
- Rectal prolapse affects boys and girls equally, but is rarely seen in the absence of predisposing conditions. It is most commonly seen from infancy to four years of age (potty training phase).
- Predisposing conditions include the following conditions:
- Cystic fibrosis which is a genetic (inherited) disease that can lead to chronic respiratory problems and gastrointestinal symptoms
- Diarrheal diseases
- Malnutrition
- Weakness of the muscles of the pelvis
- Conditions that increase pressure in the abdomen which include chronic cough, constipation, toilet training and excessive vomiting. Chronic constipation and excessive straining is the cause in approximately 15% of causes.
- Prolapse may range from minor, which goes away spontaneously, to more severe cases that require the tissue be pushed back in manually.
Signs and Symptoms (“What symptoms will my child have?”)
- Rectal prolapse is usually obvious based on physical exam alone. It appears as a dark red mass at the anus. The mass may only be present during stooling. (See Figure 3A)
- A mass at the anus that does not go away on its own needs immediate medical attention. This mass needs to be pushed back in before the blood to the segment is compromised.
- Rectal prolapse is associated with discomfort of having something coming out of the bottom. Increasing pain might mean that the tissue coming out may not be getting good blood flow.
- Sometimes there can be passage of mucous or small amounts of blood.
Diagnosis (“What tests are done to find out what my child has?”)
- Usually no blood tests are needed for the diagnosis of prolapse. If other clinical signs are present to worry about cystic fibrosis, malnutrition or weakness, then blood tests may be sent to see if these conditions are present.
- Depending on the age of the child and the clinical situation, an X-ray of the belly may be needed. Additionally, a contrast enema may also be helpful. In this test, a tube is placed inside the child’s anus and contrast liquid is injected slowly. The contrast lights up the inside of the rectum and large intestine. This study shows the anatomy of the large intestine to see if anything may contribute to rectal prolapse.
- Rectal prolapse may be transient. Your health care provider may ask your child to sit on the commode in the office to see if the prolapse would happen. Additionally, pictures taken at home can be helpful because the prolapse may not happen during the clinic visit.
Prevention
- AVOIDING rectal prolapse is the main way of dealing with the problem.
- If a child has constipation resulting in straining and sitting on the toilet for a long time, the sphincter muscle that holds the rectum in relaxes and makes prolapse happen. Recommended changes in defecation habits. Avoiding constipating foods such as milk products, rice and bananas may help. Medications such as polyethylene glycol (Miralax®), docusate and senna may be helpful in keeping stools soft.
- Changes in stooling habits may include: restriction of time spent on the commode, use of a child-specific commode or placement of a stepstool in front of an adult commode. Having the child sit on the toilet for a long time during potty training can contribute to prolapse; limiting time on the toilet is important.
- A chronic cough should be treated.
- If diarrhea is present, it should be treated.
- Specific medical treatments may be necessary in some cases, such as cystic fibrosis (which requires enzyme replacement) to prevent recurrent prolapse.
Treatment (“What will be done to make my child better?”)
- In the majority of cases, rectal prolapse reduces on its own mostly after the child stops squatting.
- If the rectal prolapse does not go back on its own, gently pushing back (reduction) of any tissue with some lubricant may help. Having the child lay on the side and relax may aid in this.
- If not successful, apply granulated sugar to the prolapsed rectum. Let the sugar sit for 15 minutes and then attempt to reduce the prolapse again. The sugar will absorb the extra water in the prolapse and cause the prolapse to shrink. You must use granulated sugar. A sugar substitute will not work for reducing the prolapse.
- If not successful, bring child to doctor.
- At times, your health care provider may gently reduce the prolapse using gloves and lubricant. If prolapse recurs shortly after reduction, taping your child’s buttocks together temporarily may have decrease the swelling in the tissue.
- Surgery may be necessary in cases where medical therapy and changes in defecation habits are not successful. Operative therapy may also be required to reduce a prolapsed rectum that cannot be reduced manually, ulcerations (injury to the lining of the rectum), painful prolapse or excessive bleeding.
- A number of surgical procedures are used (See Figure 3B – 3D). The choice of procedure is determined based on the severity of the prolapse, the underlying cause or condition, the severity of symptoms and the experience of the treating surgeon. The surgeon will check whether the rectum is healthy.
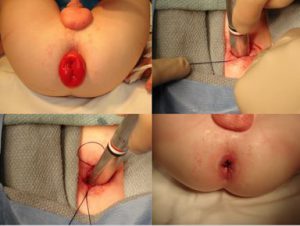 Figures 3A – 3D. Infant with rectal prolapse (2A upper left corner). Figure 3B (lower left corner) shows an infant with recurrent rectal prolapse who underwent a modified Thiersch procedure. Figure 3C (upper right corner) shows the suture tightened over a metal rectal dilator. Figure 3D (lower right corner) shows postoperative result with resolution of rectal prolapse. (Pictures provided by Dr. Romeo C. Ignacio, Naval Medical Center San Diego, California)
Figures 3A – 3D. Infant with rectal prolapse (2A upper left corner). Figure 3B (lower left corner) shows an infant with recurrent rectal prolapse who underwent a modified Thiersch procedure. Figure 3C (upper right corner) shows the suture tightened over a metal rectal dilator. Figure 3D (lower right corner) shows postoperative result with resolution of rectal prolapse. (Pictures provided by Dr. Romeo C. Ignacio, Naval Medical Center San Diego, California)
- In certain patients with a redundant rectosigmoid colon, consideration will be given to removal of this segment and fixing the remaining segment internally (rectopexy). This procedure is done either open (large incision on the belly) or laparoscopically (multiple small incisions on the belly to allow a video camera and small instruments to perform the procedure).
- Preoperative preparation: If the child is taken to the operating room to reduce prolapse as an emergency, antibiotics will be given to decrease infection. For scheduled cases where part of the large intestine may be removed, the child may need to drink fluid to clear stool out of the intestines.
- Postoperative care:
- Activity: Typically, the child is encouraged to walk around as soon as possible.
- Diet: Patients are started on liquids after their surgery then advanced to a general diet.
- Medicines: Your child may need any of the following:
- Antibiotics: To help prevent or treat an infection caused by bacteria.
- Anti-nausea medicine: To control vomiting (throwing up).
- Pain medicine: Pain medicine can include acetaminophen (Tylenol®), ibuprofen (Motrin®), or narcotics. These medicines can be given by vein or by mouth.
- Stool softeners: Polyethylene glycol (Miralax®), Docusate (Colace®) or senna are among the medications used to avoid straining after surgery.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child may eat a normal diet after surgery. Avoid constipating foods such as dairy products, rice and bananas.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after laparoscopic surgery, 4-6 weeks after open surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol®l) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, diarrhea, problems with urination, or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper post-operative healing.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- The long-term prognosis for children with rectal prolapse is good. More than 90 percent of children who experience rectal prolapse between nine months and three years of age will respond to medical treatment and will not require surgery.
- Children who develop rectal prolapse after the age of four are more likely to have underlying neurologic or muscular defects of the pelvis. These children are less likely to respond to medical treatments and should be seen early for surgical intervention.
References
- Holcomb, George W III, et al. Ashcraft’s Pediatric Surgery. New York. Elsevier, 2014. E-book.
Updated: 11/2016
Author: Romeo C. Ignacio, Jr., MD; J. Liebig, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Ruptured Appendicitis
Condition: Ruptured (Perforated) Appendicitis
Overview (“What is it?”)
Definition: Inflammation/Infection of the appendix
- The appendix is a small extension of the intestine that is connected to the large intestine (colon). The appendix is usually located in the right lower side of the belly, and it is tubular in shape. Its length differs based on the age. The appendix has no known important function.
- Appendicitis is inflammation and infection of the appendix and often results from blockage of the appendix by stool (feces). Sometimes the feces forms a small stone called a fecalith. Other causes of appendicitis include swelling of lymph tissues within the appendix wall because of recent infection; sometimes worms can also block the appendix.
- Once blockage of the appendix occurs, several things happen:
- The appendix cannot empty the mucus and fluid that it makes.
- The pressure in the appendix increases and it swells.
- Bacteria multiples inside the appendix.
- The swelling cuts off the blood supply to the appendix. If the infection continues, part of the appendix wall dies and a hole results. This is how ruptured or perforated appendix happens.
- Ruptured Appendicitis: The time interval between onset of symptoms and rupture of the appendix is about 36 to 72 hours. Rupture occurs in about one of three patients admitted to children’s hospitals. The severity of ruptured appendicitis is different for every patient. Some children have a small rupture, while others may have a big spillage of stool and pus into the abdomen. Still others can have problems with intestinal blockage from the inflammation and infection. Some children who have appendicitis going on for days before the diagnosis may be so sick that the infection spreads into the blood stream. This is a serious condition and can be life-threatening. These patients will need to be stabilized before undergoing surgery. Therefore, the treatment including timing of surgery depends on how sick the patient is.
- Incidence: There are 70,000 appendicitis cases in kids per year in the United States. Overall, 7% of people in the United States have their appendix removed during their lifetime.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs:
- When inflammation in the appendix begins, there is pain around the middle of the belly by the belly button. The child may have decreased appetite and feels like vomiting. The pain never completely goes away and becomes sharper with time.
- Most children with appendicitis have a fever of 38°C to 39° C (100.5°F to 102°F).
- Later signs/symptoms: More than 24 hours after the pain starts, it moves to the right lower side of the belly. Sometimes, a child complains of right lower abdominal pain while walking or refuses to stand up or walk due to pain. Younger children (less than five years old) have a higher chance of having ruptured appendicitis because they may not be able to talk clearly about their symptoms. If the appendix ruptures, a high fever may be seen. There may be episodes of diarrhea.
Diagnosis (“What tests are done to find out what my child has?”)
- History: The doctor will obtain a history and perform a physical exam. This is important for diagnosis of appendicitis. The surgeon will be interested in the type and location of pain: right lower side that hurts with jumping, walking or other jarring movements. The doctor will ask whether the child may have nausea, vomiting, refusal to eat, fever or diarrhea.
- Physical examination: Includes a careful abdominal examination performed by the surgeon. Other medical problems that cause belly pain will be investigated.
- Laboratory tests: Bloodwork may be sent to look at suggestion of an infection. Urine may be tested for a bladder infection or a kidney stone. Female teenagers should have a urine pregnancy test.
- Diagnostic studies: In some cases, the child’s story and the examination by the doctor may be very convincing that appendicitis is present. If the diagnosis is not clear, other tests may be ordered:
- Chest X-ray: If there is a concern for pneumonia
- Abdominal X-ray: A belly X-ray looks for clues regarding what may be causing the pain in general.
- Ultrasound: Ultrasound is very helpful to diagnose appendicitis. A probe is placed over the belly and sound waves are used to look at the appendix. Ultrasound may be useful for girls to look at the ovaries.
- Computed tomographic (CT) scan: CT is most useful when the diagnosis is not clear or if ruptured appendicitis suspected. Unlike ultrasound, CT scan uses radiation to obtain images. The child may be asked to drink a liquid that outlines the stomach and intestines. Sometimes, the contrast is given through the rectum. In some cases, an IV medicine is needed to help the CT get better pictures leading to a more accurate diagnosis.
- Conditions that mimic appendicitis: Gastroenteritis (“stomach flu”), constipation, ovarian cyst, twisting of ovary (torsion), groin (inguinal) hernia, pneumonia, Meckel’s diverticulum, inflammatory bowel disease, kidney diseases, urinary tract infection, intestinal obstruction, pregnancy.
- It is important to note that
- Children with history and physical exam findings that are convincing with appendicitis may not need any further tests
- In children with unclear cause of belly pain, there are several possibilities.
- If the diagnosis of appendicitis is not clear, the doctor may recommend observation in the emergency room or hospital for a period of time. A doctor will examine the child every few hours to see if the pain gets better or worse.
- Ultrasound or CT may be done depending on the situation.
Treatment (“What will be done to make my child better?”)
- Medical treatment
- Since appendicitis is an infection, antibiotics are an important part of the treatment. Antibiotics are medicines that fight bacteria. It is given through the vein.
- Patients with ruptured appendicitis have a high risk of getting infection of their wound or developing an abscess or pus collection inside their belly. They need several days of antibiotics depending on how bad the rupture is.
- Fluids are needed for patients with appendicitis. Since appendicitis causes loss of appetite, the patient may be dehydrated. Fluids are usually given through the vein.
- Medicine is also given to the patient to help make their belly pain better.
- Since appendicitis is an infection, antibiotics are an important part of the treatment. Antibiotics are medicines that fight bacteria. It is given through the vein.
- Surgery: The standard way to treat appendicitis is by removing it (appendectomy). This can be done the traditional way (“open” or larger incision) or laparoscopic.
- Open appendectomy: The appendix is removed through a transverse open incision in the right lower part of the belly.
- Laparoscopic appendectomy: In laparoscopic appendectomy, several small cuts (incisions) are made. Through one of the cuts, a video camera is placed. The surgery itself is done using small instruments placed through the other incisions. The usual number of incisions (cuts) for laparoscopic surgery vary from one (single port umbilical) to three. Sometimes an extra cut is needed if the appendix is really ruptured and stuck. The placement of the incisions depends on the location of the appendix.
- Open and laparoscopic appendectomy take the same amount of time to perform. Appendectomies for ruptured appendicitis take longer than those for non-ruptured appendicitis. One benefit of laparoscopy is that other abdominal structures can be examined using the video camera during surgery. Laparoscopy also has lower risks of wound infection.
- Special circumstances with ruptured appendicitis and their treatment
- Ruptured appendicitis with abscess. Patients with ruptured appendicitis spill stool from the appendix into the belly. This causes an infection resulting in a collection of pus or an abscess. The abscess may be seen on ultrasound or CT. If the abscess is big, the surgeon may decide that the infected fluid should be drained first to calm down the infection before doing surgery. With an operation done when there is a large abscess, there is a higher complication rate than an operation done when the abscess is resolved.
- Drainage of the abscess is usually done by a specialist that will use either an ultrasound or CT to look for a safe window to drain the pus. Sometimes the window is through the front of the belly, the side of the belly or even through the opening of the anus. Placement of the drain depends where the abscess is located and the internal organs around it. Usually, the radiologist leaves a small drainage tube to allow all the infected fluid to come out. The drain is removed when all the pus has been drained.
- Drainage of the abscess and antibiotics settle the infection. The patient feels better and is able to be sent home. The appendix is removed weeks later.
- Ruptured appendicitis and intestinal obstruction:
- Sometimes the inflammation from ruptured appendicitis is so bad that it causes kinking of the intestines. This leads to blockage of the flow of food through the intestinal tract. Intestinal blockage or obstruction is suspected if the patient has lots of vomiting and the vomit is green or bright yellow in color. X-rays or CT may show intestinal obstruction.
- When obstruction is present, it usually means the appendicitis is severe. Although a laparoscopic approach may be possible, an open operation may be needed. This may require a large vertical incision in the middle of the belly.
- Preparation for surgery: Your child will be given fluids, antibiotics, pain medicine prior to surgery.
- Postoperative care
- Activity: Your child’s caregiver will tell you when it is okay for your child to get out of bed. Usually, the child is encouraged to walk around as soon as possible.
- Diet: In patients with ruptured appendicitis, it may take a few days for the intestines to work normally. Your doctor will make the decision when your child should ready to eat. This depends on many things such as how badly ruptured the appendix was, whether there was intestinal blockage, if your child is still vomiting, and whether he or she is passing gas.
- Foley catheter: Sometimes there is a tube or catheter that may be put into your child’s bladder to drain urine.
- Nasogastric tube: Sometimes a nasogastric (NG) tube is inserted through your child’s nose or mouth and down into his stomach. This tube keeps the stomach empty to decrease vomiting after surgery.
- Medicines: Your child may need any of the following:
- Antibiotics: This medicine is given to help prevent or treat an infection caused by bacteria.
- Anti-nausea medicine: This medicine may be given to control vomiting (throwing up).
- Pain medicine: Pain medicine can include acetaminophen (Tylenol®), ibuprofen (Motrin®), or narcotics. These medicines can be given by vein if the intestines are not fully working yet.
- Ruptured appendicitis with abscess. Patients with ruptured appendicitis spill stool from the appendix into the belly. This causes an infection resulting in a collection of pus or an abscess. The abscess may be seen on ultrasound or CT. If the abscess is big, the surgeon may decide that the infected fluid should be drained first to calm down the infection before doing surgery. With an operation done when there is a large abscess, there is a higher complication rate than an operation done when the abscess is resolved.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after laparoscopic surgery, 4-6 weeks after open surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening belly pain, fever 38.5°C (101oF), vomiting, jaundice, f the wounds are red or draining fluid, diarrhea or problems with urinating.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper post-operative healing.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Patients do well after removal of appendix.
- Complications:
- Wound infection: Happens around 3% of the time. Infections may need only antibiotics or may require opening up of the wound depending on how bad the infection is.
- Abscesses (pus pockets): Happens about 10-20% of the time with ruptured appendicitis. If the abscess is small, antibiotics may treat it. If it is big, it may need to be drained. The technique is the same as described in the section Ruptured Appendicitis with Abscess
- Small bowel obstruction: 3-5% risk after appendicitis and appendectomy.
- Complications:
Updated: 11/2016
Author: Joanne E. Baerg, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Sacrococcygeal Teratoma
Condition: Sacrococcygeal Teratoma
Overview (“What is it?”)
- Definition
- Sacrococcygeal teratoma (SCT) is a type of tumor that starts at the end of the tailbone (coccyx). It can be quite large and extend outside of the body and/or inside the belly. The tumor contains many different types of tissue including hair, teeth, bone, muscle, nerve, among others. There can be cancer tissue within SCT. The likelihood of cancer is higher in older children, and much less in newborns.
- Most SCT in newborns are non-cancerous.
- Epidemiology: SCTs are the most common tumor seen in newborn infants, occurring in 1 in 30,000-70,000 live births. SCTs are more common in girls. Most SCTs are found in infants, but some can be seen in toddlers and children four years or younger. Larger tumors, especially those outside the body, are often seen on prenatal ultrasound. Twelve to fifteen percent of children with SCTs have associated congenital anomalies, most commonly anorectal malformations and spinal abnormalities.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs
- Mass seen starting from tailbone
- In some cases, the tumor may be mostly within the belly and is difficult to diagnose on the outside.
- Tumor complications
- If the mass is very large, the heart has to pump large amounts of blood to the tumor. Symptoms of heart failure can be seen even while the baby is still in the uterus—such as fluid around the lungs, in the belly, around the heart and within the baby’s tissues. This condition is called “hydrops fetalis”.
- Bleeding from mass
- Tumor rupture: When the skin from the tumor rips off
- If a large part of tumor is inside the belly, it can block the flow of urine or stool.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests
- Blood tests: AFP, beta-HCG levels. These proteins are made by the tumor. Other blood tests such as blood count and electrolytes (minerals) will also be checked.
- Computed tomography (CT) or Magnetic Resonance Imaging (MRI) of the abdomen/pelvis will look at how big the mass is, the extent of the tumor located and blood supply.
- Chest X-ray or CT to look for pulmonary spread.
- Conditions that mimic this condition
- Lipomeningocele, lipoma, chordoma (spinal cord anomalies)
- Rectal duplication
- Epidermoid cyst
- Neuroblastoma (tumor from neural crest cells)
Treatment (“What will be done to make my child better?”)
- Prenatal Care
- Since SCTs can have complications, the mother of the baby undergoes frequent visits to her obstetrician for check-ups and ultrasounds to monitor for signs of heart failure and/or hydrops
- In most cases of SCT that is external to the baby, a Caesarian section (C-section) is recommended to avoid bleeding or rupture of the tumor.
- Medicine
- There is no medicine to treat the mass, only surgery
- Surgery
- Preoperative preparation
- Studies as above
- Intravenous antibiotics to help prevent infection
- Procedure: The goal of the surgery is to completely remove the mass. Depending on the location, the cuts (incisions) needed for the surgery can be by the buttocks only (external masses), the belly only (internal masses) or both. The tailbone (coccyx) is removed with the tumor. Not removing the coccyx is associated with up to 40% recurrence of the tumor. Sometimes a small plastic drain is placed under the skin flaps of the buttock incision.
- The mass will be sent for examination to see if there are components of cancer in the mass.
- Postoperative care
- Baby often has to lay on belly for first couple of days after surgery to allow incision to heal
- Incisions may open up and need dressing changes
- Drain are usually left in place for 3-7 days after surgery
- Medications needed will include pain medications, antibiotics and maybe nutrition delivered through the vein
- If cancer is seen in the mass, the baby will need medicine (chemotherapy) to help control the recurrence of cancer. If this is the case, cancer specialists (oncologists) will be involved in the care of your baby.
- Preoperative preparation
- Risks
- Bleeding requiring transfusion
- Wound breakdown—the skin close to the tumor can have a fragile blood supply
- Wound infection
- Urinary retention—there is a high risk of urinary problems after this procedure, likely due to the stretch of the nerves and muscles of the pelvis. The length of time that this is a problem varies from one child to another.
- Incontinence of muscles of anus—there is a risk of having problem with continence of stool. Often the tumor stretches the muscles involved in control of continence. This will gradually get better in most cases.
- Benefits: Removal of mass
Home Care (“What do I need to do once my child goes home?”)
- Diet: Normal for age
- Activity: Normal for age
- Wound care: Depends on wound. May need to do dressing changes if wound had opened up. In this case, your surgeon will help explain wound management, as it differs from one child to another.
- Medicines: Pain medications such as acetaminophen (Tylenol®) may be needed.
- What to call the doctor for: Redness, warmth, or drainage from incision. Problems with urinating or stooling
- Follow-up care
- Regular follow-up with surgeon for physical examinations and checking AFP levels. Since AFP is made by the tumor, blood levels should normalize once the tumor is removed. AFP levels is followed regularly because if it increases, it signals tumor recurrence.
- If cancer is present in the mass or if there are metastases (tumor spread beyond the main tumor such as the lungs, for example), the child will need follow-up with oncology for chemotherapy
Long-Term Outcomes (“Are there future conditions to worry about?”)
Survival rate for sacrococcygeal teratomas is more than 95%. The risk of bowel or bladder dysfunction even in benign tumors is quoted as 30-40%. Tumor recurrence can happen, therefore careful follow up is needed.
Updated: 11/2016
Author: Grace Mak, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Short Bowel Syndrome
Condition: Short Bowel Syndrome (also known as short gut syndrome, short gut, small intestinal insufficiency)
Overview (“What is it?”)
- Definition: Short Bowel Syndrome (SBS) is a condition in which the intestines, specifically the small intestine, are unable to digest and absorb the proper amount of nutrients from food to sustain life.
- This condition requires intravenous (IV) or enteral (oral) supplementation of nutrients to maintain continued growth and development for the child.
- SBS can be caused by congenital (conditions present at birth) defects, malabsorptive diseases (diseases where the intestines cannot absorb adequate calories and nutrients) or surgical removal of long segments of intestines.
- The normal length of the small intestine in a full-term infant is approximately 250 cm (about eight feet). In general, if most of the intestinal length is gone or removed, SBS can result. In some situations, although there can be adequate length of intestine, the intestine may not work well, therefore leading to inability to digest and absorb nutrients.
- Epidemiology: Short bowel syndrome can occur anywhere from birth into adulthood.
- The most common cause of SBS in infants and babies is necrotizing enterocolitis (NEC) which accounts for up to 40% of SBS patients. NEC is a severe infection of the intestines that is common in premature infants and may require removal of a long segment of intestine.
- SBS can also result from volvulus (twisted intestine leading to lost blood flow), atresia (something causes the intestine to have lost blood flow while the baby is developing in the uterus, causing segments of intestine to disappear) or complications of meconium ileus (impacted intestines commonly associated with cystic fibrosis), among other causes
- Later in childhood, intestinal trauma or inflammatory bowel conditions such as Crohn’s disease can also cause SBS.
Signs and Symptoms (“What symptoms will my child have?”)
- Diarrhea: Inability to absorb leads to diarrhea
- Failure to thrive: Since the baby is not able to digest or absorb food, it is difficult to grow and gain weight.
- Lack of energy and failure to meet milestones
Diagnosis (“What tests are done to find out what my child has?”)
- Physical examination by a physician is routinely performed with emphasis on height and weight curves. In addition, signs of vitamin deficiencies are also performed.
- Stool tests to see if fat and carbohydrates are being digested
- Blood and urine tests will be ordered regularly to check your child’s electrolyte, vitamin and nutrition parameters
- Radiographic imaging such as abdominal X-rays, ultrasound or CT scans can be used to investigate the different causes of SBS.
Treatment (“What will be done to make my child better?”)
- Most children with SBS are managed either fully or partially with nutrition delivered by vein (Total Parenteral Nutrition or TPN).
- The goal of treating SBS patients is to train the intestines gradually to digest and absorb nutrients and transition the child’s nutrition from being given by vein to being given into the gut.
- Medical strategies can take months to years to properly treat SBS. Principles of intestinal rehabilitation include:
- Early oral feeding is recommended as soon as your child is stable.
- Sometimes, feeding needs to be given continuously and your child may require a gastrostomy tube.
- Often special formula that has been partially digested is needed.
- Total Parenteral Nutrition (TPN) is a way to give nutrition through the vein. It consists of carbohydrates, protein, fat, vitamins and minerals. Often, TPN is needed to supplement nutrition in patients with SBS.
- Long-term use of TPN use is associated with blood stream infections and liver disease.
- Antimotility (anti-diarrheal) agents may be used to slow down intestinal transit time and allow food to spend more time in the intestine, thus allowing more opportunities for nutrient absorption.
- Medicines to decrease acid production in the stomach are used because high acid content that reaches the intestine can make diarrhea worse.
- Antibiotics are selectively used if bacterial overgrowth is suspected.
- Vitamin/mineral supplementation and electrolyte repletion as needed
- Early oral feeding is recommended as soon as your child is stable.
- In select patients, surgery can be used to lengthen short intestine, taper dilated intestine or slow down the movement of intestinal contents. Some options include:
- Longitudinal intestinal lengthening and tailoring (LILT) procedure is also known as the “Bianchi” procedure. Originally described in the 1980s, LILT procedure can only be done once per patient. Currently, this procedure is rarely performed.
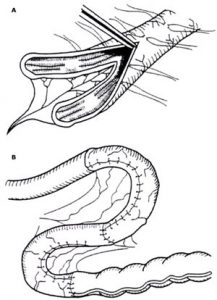 Figure 1.
Figure 1.
- Serial transverse enteroplasty procedure (STEP) is a intestinal lengthening procedure which is now the preferred intervention at most SBS centers because it can be repeated and used after a prior Bianchi procedure. The STEP increases intestinal length and improves intestinal absorptive ability by using a special stapler to make intermittent transverse cuts in the intestinal wall that can then be stretched.
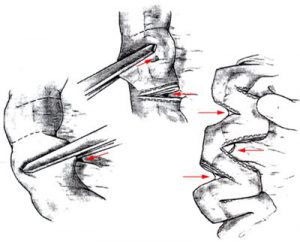 Figure 2
Figure 2
- Interpositioned reversed intestinal segmentation is a procedure where a section of intestine is removed and then connected in the reverse direction. This leads to decreased nutrient transit time with peristalsis (intestinal contraction) occurring in the opposite direction through that segment.
- Combined small intestine/liver transplantation is indicated in patients who have irreversible intestinal failure-associated liver disease. Five-year survival rates are greater than 75% if a suitable donor can be found. Possible complications include graft rejection (condition where the transplant fails) and sepsis (infection) and patients require lifelong immunosuppression therapy.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Long-term use of TPN can lead to liver disease, which is a major cause of complications and death associated with SBS.
- Depending on the original cause of your child’s SBS, how much intestine is left, whether or not the valve between the small and large intestine (ileocecal valve) remains, the condition can improve, with or without surgery, as the intestine “adapts” and improves its ability to digest and absorb.
- In most cases, babies start with a combination of TPN and feeds through the gut (by mouth and/or by G tube). Slowly increasing the food that the intestines process can make the intestines adapt and rehabilitate.
- If no progress is made with advancing feeding through the gut, then intestinal lengthening operations are considered.
- If all medical and surgical options have been tried and no progress is made with advancing on feedings through the gut, a transplant may be considered.
References
- Coran: Pediatric Surgery, Seventh Edition © 2012, Elsevier Inc.
- Ziegler: Operative Pediatric Surgery, First Edition ©2003, McGraw-Hill Inc.
- NIH Medline, https://www.nlm.nih.gov/medlineplus/ency/article/000237.htm
- UpToDate, http://www.uptodate.com/contents/management-of-the-short-bowel-syndrome-in-children
Updated: 11/2016
Authors: Romeo C. Ignacio, Jr., MD, Manuel Lizardo, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Skin Lesions
Condition: Skin Lesions: lumps and bumps – dermoid cyst, epidermal cyst, pilomatrixoma, sebaceous cyst
Overview (“What is it?”)
- Definition: The term “cyst” generally means an abnormal ball or collection of fluid surrounded by a thin wall of tissue. Children can get small cysts in the skin or in the fatty tissue under the skin. Some types of cysts may be present at birth, and others may develop in childhood. Different names may be applied to these cysts depending on what type of tissue is causing the cyst to develop. Cysts are generally benign (not cancer).
- Epidemiology: Many kinds of skin cysts are very common in babies and children.
- A dermoid cyst is congenital (present at birth) because it is formed during fetal development. These are most commonly seen in the head and neck area, such as the scalp, eyebrow and nose, but can be found in other places in the body as well. This type of cyst is filled with fluid and hair from skin structures within the cyst.
- Epidermal cysts may be congenital as well, but can also form spontaneously from an abnormal hair follicle or result from trauma. They are found typically on the scalp, face, neck and trunk.
- Pilomatrixoma is a small benign solid tumor (i.e. not a cyst) of the skin that develops commonly during childhood. It results from abnormal calcium deposits in a hair follicle.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs and symptoms: Cysts are usually found by a child or parents as a non-painful and non-tender bump on or under the skin (1-2cm). A cyst feels soft while a pilomatrixoma is very hard. The skin itself over the bump is usually normal, but it may have a slight red or blue discoloration and sometimes a small skin dimple or sinus tract (hole connecting with the cyst).
- Later signs/symptoms: Many cysts may slowly get bigger over time and may cause symptoms of pain as they enlarge. The most serious problem that can happen with these cysts is infection. Infection is suspected when there is redness, increasing pain and swelling, and possibly fevers and pus draining out of the skin over the cyst.
Diagnosis (“What tests are done to find out what my child has?”)
- Physical exam by a physician
- Blood tests are usually not necessary.
- Ultrasound may be helpful if it is unclear if the skin bump is a simple cyst or something deeper or more complicated, but this is often not necessary.
- Dermoid cysts on the scalp can erode into or through the bone of the skull, so may require a CT scan or MRI to look for this.
Treatment (“What will be done to make my child better?”)
- Treatment: Treatment with medicine will not make any of these skin lesions go away. If a cyst becomes infected, treatment with antibiotics may be needed before it can be safely removed with surgery.
- Surgery to remove these benign skin lesions is recommended, even if there are no symptoms, because they tend to enlarge and can become infected. Surgery to remove a cyst is quite straightforward if it has not been infected. A cyst that has already been infected can and should be removed, but the surgery may be more difficult and the risks are slightly higher.
- To prepare your child for surgery, it is important to keep him or her as healthy as possible before surgery. If infection is present, your child may be given antibiotics before surgery is completed. It is important to keep the area as clean as possible. You may be instructed to bathe him or her the day prior to or the day of surgery to decrease the skin contamination.
- Postoperative care consists of pain management and wound care. Most children can go home from the hospital that same day.
- Risks/Benefits: The primary benefit of removing the cyst is eliminating the risks of infection or pain symptoms as the bump becomes bigger. Depending on the location of the cyst, there may also be cosmetic benefits. While all surgery has some risks, this is generally considered low risk. There is a small risk of infection or bleeding in the wound within a few days after the surgery. The cyst may recur (form again or come back) if it is not completely removed, which is a higher risk if it has been infected or had ruptured .
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child may resume a normal diet after surgery. You should encourage your child to have plenty of fluids, fruits and vegetables to prevent constipation.
- Activity: Your child may be naturally less active after the surgery due to pain for 1-2 days, but may resume any activity that they wish as their pain resolves.
- Wound care: Surgical incisions should be kept clean and dry for about 2-3 days after surgery. Thereafter, the child may shower, but soaking the area of the wound should be avoided for about a week. If stitches were used, these are usually absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care that applies to your child specifically.
- Medicines: Children are sent home with medicines to control their pain. These may include acetaminophen (Tylenol®), ibuprofen (Motrin® or Advil®), or sometimes even oral narcotics. Your doctor will decide which of these medicines are needed. If narcotics are prescribed, it is advisable for the child take a stool softener (docusate, Miralax® ) to prevent constipation since narcotics can have this side effect. Antibiotics are not needed unless infection was suspected at the time of surgery.
- What to call the doctor for: Call your doctor for signs of infection in the incision including increasing pain, redness, swelling, fever and fluid or pus draining out of the wound.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing. Follow-up can sometimes be arranged with your child’s primary care doctor or even with a phone call depending on what your surgeon deems appropriate.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- After surgical treatment, the long-term prognosis is excellent. Your child should be expected to grow and develop normally after the surgery.
- Once removed, the only long-term risk is recurrence if the cyst is not completely removed and forms again, which is rare.
Updated: 11/2016
Author: Charles M. Leys, MD, MSCI
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Spontaneous Pneumothorax
Condition: Spontaneous Pneumothorax
Overview (“What is it?”)
- Definition: Often referred to as “collapsed lung”,” pneumothorax” refers to the presence of air around the lung in the chest. This air is introduced either from the outside world through a chest wound or from leakage of a portion of lung itself. Such air leakage is usually caused by injury or recent surgery; spontaneous pneumothorax specifically refers to those instances in which there was no apparent cause for air leakage from the lung.
 Figure 1. A chest X-ray of a patient with a large right pneumothorax. The chest space on the left half of the picture (which is the patient’s right) is much darker than the other side. This is because the lung is totally collapsed.
Figure 1. A chest X-ray of a patient with a large right pneumothorax. The chest space on the left half of the picture (which is the patient’s right) is much darker than the other side. This is because the lung is totally collapsed.
- Epidemiology: It is estimated that roughly 20,000 cases of adult and pediatric spontaneous pneumothorax occur in the United States each year. Males are affected six times more frequently than females. While they are more common in tall, thin males, only in rare circumstances is an associated genetic alteration present.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: The early signs are pain and shortness of breath. Pain is on the affected side of the chest and typically worse with deep breaths. Shortness of breath can make the child feel like they can’t catch their breath or just that they can’t exert themselves. There may be coughing as well. The pain is not typically associated with tenderness (pressing on the chest won’t make it worse).
- Later signs/symptoms: As pneumothorax progresses, the lung shrinks smaller and smaller. This will not cause different symptoms, but the existing symptoms will become worse.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: A chest X-ray is the first test that is usually taken when a child has breathing problems or chest pain. If a pneumothorax is seen, a computed tomography (CT) scan of the chest may be obtained to look for blebs that may be the cause of this problem. Imaging tests (chest X-rays and CT scans) are used to diagnose spontaneous pneumothorax.
- Conditions that mimic this condition: Pneumonia and rib fractures can mimic pneumothorax.
Treatment (“What will be done to make my child better?”)
- There are three basic means of treating the condition: Observation, chest tube placement and operation (surgery).
- Observation relies on the body to reabsorb the air around the lung, presuming that the amount is small and the lung has already sealed over so that it is not continuing to leak air.
- There are no medications that can be prescribed to cure pneumothorax. Oxygen is sometimes used to speed the reabsorption of the air around the lung (in those cases of small pneumothorax in which observation is planned).
- Placement of a temporary chest tube between two ribs actively withdraws air and helps the lung re-expand. Alternatively, in some cases, a needle may be introduced into the chest cavity to aspirate the air to allow the lung to expand.
- Surgery: Surgery is an option if the pneumothorax does not get better with the first two options, pneumothorax returns or there are circumstances that require definitive results. Most spontaneous pneumothoraces are believed to be caused by a weakness in the lung called a bleb (Figure 2). The bleb pops and air exits from the lung to the chest cavity. The goals of surgery goals include removal of the bleb and preventing the lung from collapsing should another bleb occur. A pleurodesis operation aims to generate scar formation between lung and chest cavity to prevent future collapse. A temporary chest tube is left in place after surgery to evacuate air and allow the lung to heal.
- Observation relies on the body to reabsorb the air around the lung, presuming that the amount is small and the lung has already sealed over so that it is not continuing to leak air.
 Figure 2. View of lung tissue from inside the chest during a thoracoscopic (minimally invasive operation). In the middle of the image, a third of the way up from the bottom, there is an outpouching of tissue with a more white color; this is a “bulla” or “bleb” of lung, which is a weakened area that can rupture and cause spontaneous pneumothorax.
Figure 2. View of lung tissue from inside the chest during a thoracoscopic (minimally invasive operation). In the middle of the image, a third of the way up from the bottom, there is an outpouching of tissue with a more white color; this is a “bulla” or “bleb” of lung, which is a weakened area that can rupture and cause spontaneous pneumothorax.
- There are two approaches to this operation. An open operation requires a large cut between the ribs on the side of the pneumothorax. Most commonly, the operation is performed using thoracoscopy. In this approach, several small cuts (incisions) are made. Through one of the cuts, a video camera is placed. The surgery itself is done using small instruments placed through the other incisions.
- Preoperative preparation: Preparation for operation requires a skin cleansing and dose of antibiotic.
- Postoperative care: This portion of the care is focused on minimizing pain and waiting for the lung to heal. The chest tube can only be removed once the lung has no air leaking from it and is able to remain fully inflated without the tube providing assistance by suction. Typically, the tube is removed by 3-5 days after operation.
- Risks/Benefits: The benefit of operation is that it is the most definitive means of treating the condition as well as minimizing the possibility of recurrence. Every operation has risks; for this operation are bleeding, infection, recurrence of pneumothorax, and injury to chest structures requiring conversion to an open operation.
Home Care (“What do I need to do once my child goes home?”)
- Diet: No restrictions. Maintaining adequate nutrition (including calories from protein) speeds wound healing.
- Activity: If surgery or chest tube placement was performed, sports and vigorous play may be a little painful in the first two weeks or so. Within a few weeks, most patients are feeling “like themselves” and have no lingering discomfort. Controversy exists when discussing special situations such as traveling to altitude or SCUBA diving. Your surgeon will discuss their recommendations with you.
- Wound care: If surgery was performed, the wounds should stay dry for three days, then the child may shower. Wait for about one week after surgery before soaking the wounds. There may be a small healing area (less than half an inch) where the chest tube was in place that may need special attention. Ask your surgeon what should be done with the chest tube dressings.
- Medicines: No long-term medications are required. Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Any concern about the incisions or difficulty breathing.
- Follow-up care: A routine clinic visit to ensure proper healing. Long-term follow-up is not generally necessary.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- There are two long-term issues to keep in mind.
- Recurrence (pneumothorax occurring again) is expected about 30% of the time if operation is not performed. If operation (pleurodesis) is performed, that risk is less than 5%.
- Activity in settings of altered pressure (extreme altitude, skydiving and SCUBA) is a gray area for which we don’t expect to ever have firm, scientific recommendations. Because of the changes in pressure that the lung experiences in these settings, it is believed that recurrence is more likely and that the consequences can be much more severe. The threat to life is probably reduced in patients who have undergone thorough pleurodesis, but we can’t be certain.
Updated: 11/2016
Author: Ramin Jamshidi, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Testicular Torsion
Condition: Testicular Torsion
Overview (“What is it?”)
- A young male’s testicle hangs from a cord called the “spermatic cord“. This is the cord that brings blood and other important structures to the testicle. (See Figure 1)
- Testicular torsion is when the testicle rotates and twists the spermatic cord. When this happens, the blood flow is pinched off and unable to get to the testicle, causing severe pain and swelling. (See Figure 1).
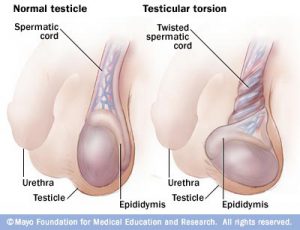 Figure 1 Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved.
Figure 1 Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved.
- Testicular torsion can happen in all ages, but usually happens in boys ages 12-16 (about 65% of all testicular torsion) or as a young baby (also called neonatal torsion).
- Usually, the testicle is held in place by surrounding tissue, but some boys don’t have enough anchoring tissue, allowing the testicle to move freely and twist within the scrotum.
- Testicular torsion can also be caused by an injury to the scrotum, commonly occurring during sports or activity.
- Testicular torsion is a SURGICAL EMERGENCY and you must seek medical help as soon as possible.
Signs and Symptoms (“What symptoms will my child have?”)
- The most common symptom of testicular torsion is sudden, severe testicular/scrotal pain. This pain can often wake boys from sleep in the middle of the night.
- Other signs and symptoms include
- Abdominal pain
- Nausea and vomiting
- Swelling of the scrotum
- Redness of the scrotum
- Pain in the groin
- Pain while urinating
- A testicle that sits higher or in a different position than usual
Diagnosis (“What tests are done to find out what my child has?”)
- Usually, the diagnosis is made based on the child’s medical history and physical exam done by an experienced doctor.
- Another test that is usually done is a scrotal ultrasound. Ultrasound uses sound waves to create images and pictures. It is particularly good at looking at blood flow. This is a test that does not cause pain or emit radiation. It involves using a wand to check the blood flow to the testicles.
- Urine and blood tests may be done to make sure that there is not another reason for the child’s pain.
Treatment (“What will be done to make my child better?”)
- The treatment for testicular torsion is surgery to detorse (untwist) the testicle. It is important that a surgeon evaluates the child, as surgery must be done as quickly as possible to prevent loss of the testicle.
- The doctor may temporarily untwist the testicle manually to allow blood to flow in and out of the testicle before surgery. Nevertheless, this is a surgical emergency.
- TIME IS KEY! The testicle must be detorsed (untwisted) with surgery as soon as possible.
- If detorsed within 4-6 hours after the start of symptoms = 98% chance of saving the testicle
- If detorsed within 12 hours after the start of symptoms = 20% chance of saving the testicle
- If detorsed 24 hours or more after the start of symptoms = 0% chance of saving the testicle.
- In some rare cases, the testicle may have gone too long without blood flow, and may need to be removed (also called orchiopexy).
- During the surgery, the surgeon will check the other testicle and fix it to the scrotum if necessary to prevent future torsion.
Home Care (“What do I need to do once my child goes home?”)
- Your child’s care at home will vary depending on the hospital, doctor and the child’s unique case. It is important to remember to follow all of the discharge instructions given to you when leaving the hospital. The following are general guidelines for your discharge.
- Diet: Your child should eat a normal diet after surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe. Usually wounds are kept dry for 3-5 days, then can be washed gently with soap and water. Avoid soaking surgical wounds for at least seven days after surgery.
- Medicines: Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, diarrhea, problems with urination, or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow up with his surgeon 2-3 weeks after surgery to ensure proper postoperative healing.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- If one testicle has to be removed (orchiopexy), the boy will still be able to make hormones (testosterone) due to the presence of the other testicle and will still be able to have children in the future.
- A testicular implant may be surgically placed for cosmetic appearance during the initial surgery or in the future. Your surgeon will discuss this option with you if an orchioectomy is required.
- The prognosis is overall good with excellent fertility function if the testicle is successfully saved.
References
- Crain, E., Gershel, J. (2010). Clinical Manual of Emergency Pediatrics (5th ed.). New York: Cambridge University Press.
- Ashcraft, K. (2010). Ashcraft’s pediatric surgery (5th ed.). Philadelphia: Saunders/Elsevier.
- Brenner, J. et. al. (2015, July 10). Causes of Scrotal Pain in Children and Adolescents. UpToDate.
- Figure 1: https://www.riversideonline.com/health_reference/Mens-Health/testicular-torsion.cfm
Updated: 11/2016
Author: J. Beck, MD, Romeo C. Ignacio, Jr., MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Thyroglossal Duct Cyst
Condition: Thyroglossal Duct Remnant or Cyst
Overview (“What is it?”)
- Definition: A thyroglossal duct cyst (TGDC) is the most common congenital neck lesion observed in children. The most common presentation is a soft nodule in the center of the upper neck under the chin in a toddler or child.
- Epidemiology:
- TGDC slightly more common in females.
- It most commonly presents in the first decade of life, usually between years two and five.
- It may present with redness, and drainage if it is infected.
- The thyroglossal duct is a remnant of the developing thyroid gland. When the thyroid develops in baby, it starts at the base of the tongue and travels to its final location in the lower neck. In normal development, the tract that the thyroid creates from the tongue to the neck dissolves. The tract can persist at any point on its line of travel from the tongue to the thyroid, creating a fluid collection or cyst. The most common location is over the small bone called the hyoid bone, in the upper neck, right under the chin.
- The cyst connects through the hyoid bone towards the base of tongue. Removing the middle part of the hyoid bone is necessary to decrease the recurrence of TGDC.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: Thyroglossal cysts will initially present with a painless swelling in the midline. This cyst will move with swallowing or with tongue protrusion.
- Later signs/symptoms: If infected, the child will have a tender neck mass and there may be draining pus. The child may have a fever. If the mass swells, changes in voice or pain with swallowing or shortness of breath are possible. Seek immediate medical attention if this is the case.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: This condition is diagnosed on physical examination
- Ultrasound is used to look at the cyst, but also confirm the presence of a normal thyroid gland in the neck.
- Conditions that mimic this condition:
- A dermoid cyst is a simple cyst from the skin over the neck.
- A simple lymph node in the location over the hyoid bone can mimic TGDC.
Treatment (“What will be done to make my child better?”)
- Medicine: If the TGDC has become infected, antibiotics are needed to help control the infection.
- Surgery
- If the TDGC is infected, an incision and drainage is necessary to control the infection completely. The infection needs to be controlled before definitive removal of the TDGC.
- Preoperative preparation: If surgical excision of a thyroglossal duct cyst is planned, then the child will generally come to hospital the morning of surgery with an empty stomach. The child should shower or bathe the night before or the morning of the surgery. Antibiotics will be given in the operating room, prior to starting the operation. No other preparation is needed.
- The procedure to remove a thyroglossal duct cyst is called the Sistrunk operation. When the child is asleep under general anesthesia, an incision is made over the cyst and it is removed. A central piece of the hyoid bone is removed with the cyst to decrease chance of recurrence. If there is a history of infection, a small drain may be sewn in place.
- Postoperative care: Often the child will stay one night in hospital to observe for any swelling of the airway and ensure normal breathing. Pain medications will be given.
- Risks/Benefits
- Risks: Immediate surgical risks are intra-operative bleeding, damage to the surrounding structures such as the airway, the risk of anesthesia and postoperative infection. The risk of recurrence of the cyst is reported at 1-5%.
- Benefits: Surgical excision of a TGDC by the Sistrunk procedure prevents infection in the cyst and decreases the chance of a cancer developing in the future.
Home Care (“What do I need to do once my child goes home?”)
- Diet: No limitations of diet.
- Activity: Normal activity and return to school in 3-5 days after operation. Generally, the child will be restricted from physical education or gym class until the surgeon reviews the child in the office at the postoperative visit.
- Wound care: This will be explained prior to discharge. Usually keep the wound dry for about three days, after which showers may resume. May want to wait until about a week for soaking the wound (baths, swimming). If a drain is in place, its care would be explained to you prior to discharge.
- Medicines: Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Any shortness of breath, breathing difficulties or swelling of the neck, call your doctor immediately or call 911. Spreading redness or drainage can be signs of infection and the surgeon should be contacted.
- Follow-up care: Post-operative visit at 2-3 weeks after surgery. As the surgery heals, no further treatment is needed.
Long Term Outcomes (“Are there future conditions to worry about?”)
- Long term outcomes are excellent. Most children heal completely with no further problems. The surgeon will observe for signs of a recurrence.
- If the TGDC recurs, then a second operation may be needed. However, if the center of the hyoid was removed at the first operation, and the operation was performed when no infection was present, then the risk of recurrence is low.
Updated: 11/2016
Author: Joanne E. Baerg, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Thyroid Cancer
Condition: Thyroid Cancer
Overview (“What is it?”)
- Definition: Thyroid cancer is a cancer that involves the thyroid gland, a butterfly-shaped gland in the front part of the neck. The thyroid makes hormones that are important for growth, metabolism and control of calcium levels in the body.
- Epidemiology: Thyroid cancer is the third most common solid tumor malignancy in children. It occurs four times more commonly in females compared to males. Some risk factors for the development of thyroid cancer include history of radiation and chemotherapy. Other types of cancer (medullary thyroid cancer) are common in certain families.
Signs and Symptoms (“What symptoms will my child have?”)
The most common presentation is a firm, non-painful neck mass in the location of the thyroid gland. This may be accompanied by swollen lymph nodes, difficulty swallowing. Less commonly, a fullness in the neck, persistent hoarseness or difficulty swallowing may be experienced.
Diagnosis (“What tests are done to find out what my child has?”)
- If you are worried regarding symptoms that we mentioned previously, you should take a child to a doctor who can perform a careful examination of the head and neck area which would include the thyroid and the surrounding lymph nodes to check for lumps.
- Types of Thyroid Cancer:
- Papillary: This form of thyroid cancer arises from cells that make thyroid hormone. This cancer grows slowly, but can spread to the lymph glands close to the thyroid (80% of the time). It can rarely spread to other organs such as the lungs (20% of the time) and other structures of the neck such as the esophagus, neck muscles and airway (30%). It is the most common type of thyroid cancer in children.
- Follicular: This type of cancer also comes from the cells that make thyroid hormone. It spreads through blood vessels and therefore, more commonly spreads to sites of the body away from the neck.
- Medullary Thyroid Cancer (MTC): This more aggressive type of cancer occur in cells within the thyroid gland that control calcium levels. It is seen more commonly within families with a specific genetic mutation (RET gene) such as multiple endocrine neoplasia type 2 (MEN 2). These cancers occur in younger children and can be very aggressive. If your family has known MEN 2, it is important to have your baby examined even at a very young age (age less than one year) in order to treat this cancer before it spreads. In fact there are certain inheritable changes in Chromosome 10 (M918T and A883F) that are classified as “D” subtypes, the highest risk of MTC. In these cases, thyroid removal is recommended before one year of age.
- Anaplastic: This form of cancer is not seen in children. It is fast growing and can be fatal.
- Labs and tests
- A blood test may be performed to see how well the thyroid is functioning.
- An ultrasound of the thyroid, which consists of examining the gland with sound waves and a computer, can determine characteristics of the lump—such as its location, whether if contains fluid (cyst), or whether other lumps exist.
- Another test that may be performed is a radioactive iodine scan, which looks at whether or not the mass takes up iodine. Sometimes masses that do NOT take up iodine are more likely to be cancerous.
- In some situations, a fine needle aspirate is performed, where a doctor inserts a needle directly into the mass and removes a sample of the cells. Another doctor will examine the cells under the microscope to determine whether they are cancerous. Sometimes it is necessary to remove part of the gland with the tumor in order to help with the diagnosis and treatment of the problem.
- If MEN 2 is a disease process in your family, it is mandatory that your child be tested for the possibility that he or she inherited the abnormal chromosome. The type of RET gene abnormality will determine when surgery should be performed.
- Conditions that mimic this condition: Other tumors or growths arising from the neck need to be ruled out, including other thyroid masses or enlarged lymph nodes.
Treatment (“What will be done to make my child better?”)
- Surgery
- Most cases of papillary and follicular thyroid cancer start with thyroid lobectomy (removal of the half of the thyroid that contains the disease). This aggressive approach in children is because there is a higher chance of thyroid cancer in children compared to adults, and a fine needle aspiration may miss cancerous tumors from the mass. At the time of the thyroid lobectomy, the sample containing the tumor is frozen and examined under a microscope. If papillary or follicular cancer is seen and confirmed, removal of the rest of the gland performed. Removal of the rest of the gland is performed because extensive disease, higher rates of spread, and recurrences are more common in children. Sometimes the pathologist (doctor who examines the cells under the microscope) cannot definitively make a call with regard to the presence of cancer using this quick technique. If so, he or she will need to do more extensive tests which may take a few days. If cancer is seen, then the other half of the thyroid is removed as soon as possible, before scarring of the operative site can occur.
- If lymph nodes are involved, then they need to be removed.
- If follicular cancer is small (less than 1.5 cm in its largest dimension), a lobectomy may be considered.
- In MTC, most children between 3-5 years of age should have RET testing, thyroid ultrasound and a blood test to check their calcitonin levels, and thyroid removal before age of five years. However, some types of RET abnormalities (“D types”) put the patients at such high risk that surgery to remove the thyroid is recommended before age one.
- Preoperative preparation: No special preparation is needed. The child should shower or bathe the night before or the morning of surgery.
- Postoperative care: Your child may require an overnight hospitalization or may require a hospital stay for a couple of days. Some surgeons leave a small drain in the surgical bed to allow excess fluid to be removed. Your child will be checked for evidence of bleeding (neck swelling), nerve injury (hoarseness), and low calcium levels for several hours after surgery.
- Risks/Benefits: Risks of surgery include bleeding in the hours immediately following surgery. This manifests as swelling in the neck, and if there is a lot of blood, it may compress the airway and cause difficulty breathing. This occurs rarely, but will require an emergent operation to evacuate the blood clot and find the bleeding vessel. Another complication is injury to the nerves around the thyroid. These nerves control the muscles of the voice box and may cause hoarseness. The injury may be temporary or permanent. The thyroid is located very close to the other glands that also control calcium levels (parathyroid glands). These glands may be injured or removed at the time of the surgery; calcium levels may go down after thyroid surgery. Calcium blood levels will be checked. Symptoms of low calcium include numbness or tingling around the face, mouth and fingertips.
- Radioactive Iodine Therapy: For papillary and follicular cancer, radioactive iodine therapy is usually performed six weeks or so after surgery to destroy remaining cancer calls. The iodine is concentrated by the remaining thyroid cells, and the radiation specifically kills remaining thyroid cells.
- Chemotherapy: If the cancer has spread to other parts of the body, drugs may be required to stop or slow down the growth of the cancer.
- Radiation therapy: Some forms of cancer may require radiation.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Usually the child can be on a regular diet appropriate for age when he or she goes home.
- Activity: If your child had a biopsy only, regular activity can be resumed about two days after surgical procedure. Regular activity can resume slowly a few days after surgery.
- Wound care: Specific wound care issues should be addressed with your child’s surgeon. Usually wounds are kept dry for about three days, then child may shower. Soaking the wound (such as baths or swimming) should wait until a week after surgery.
- Medicines
- Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- If your child required removal of the entire thyroid gland, he or she will require thyroid hormone replacement to help normalize his or her growth and metabolism. Thyroid hormone also slows down the growth of thyroid cells, which may be present.
- If your child has persistent low calcium levels, he or she will need calcium supplements.
- What to call the doctor for: A call to the surgeon should be done if there is worry about infection (unexplained fevers, redness and drainage of the wound). If your child experiences numbness and/or tingling around the fingers and the face, you should call the surgeon or endocrinologist as well.
- Follow-up care: A wound check is often performed in 2-3 weeks after surgery. Often, the child’s oncologist can also provide follow-up of the wound as well.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Future outcomes for this type of cancer are excellent. The best outcomes are seen in teenage girls, papillary type of tumor, and tumors localized to the thyroid gland.
Updated: 11/2016
Author: Marjorie J. Arca, MD
Editor: Patricia Lange, MD
Torticollis
Condition: Torticollis (wry neck)
Overview (“What is it?”)
- Torticollis or wry neck or fibromatosis colli is a condition where the side muscle of the neck (sternocleidomastoid, Figure 1) becomes inflamed. The inflammation causes the muscle to tighten and shorten, tilting the back of the head towards the affected side and rotating the chin away from the affected side. Because it usually happens on one side only, the condition results in the child’s head tilting to one side all the time. It usually affects babies in the first few months of life. There is no known cause but sometimes it is associated with birth trauma from a breech delivery,
- In rare situations, it does occur in older children, secondary to trauma to the neck or certain spine conditions.
- Epidemiology: Torticollis occurs in 0.3-2.0% of babies.
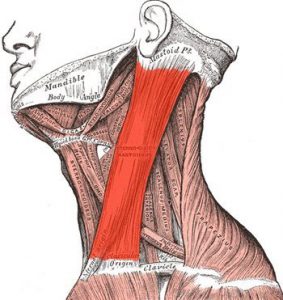 Figure 1: Sternocleidomastoid muscle. https://upload.wikimedia.org/wikipedia/commons/1/1a/Sternocleidomastoideus.png
Figure 1: Sternocleidomastoid muscle. https://upload.wikimedia.org/wikipedia/commons/1/1a/Sternocleidomastoideus.png
Signs and Symptoms (“What symptoms will my child have?”)
- The parents notice that the head is tilted one way and the chin is rotated towards the other side, forcing the baby to look to one direction. Because the back of the head is pulled towards one side the eyes become uneven, with the one on the affected side being higher than the other. In other situations, the parents or the pediatrician feel a hardening of the muscle. Sometimes, it is mistaken for a tumor.
- If left untreated, two long-term problems arise. The head and skull grow lopsidedly. The child’s vision can be affected because of the abnormal position of the eyes.
Diagnosis (“What tests are done to find out what my child has?”)
- All that is needed to make the diagnosis in an infant are the physical findings of the rotated chin and tilted head and a physical examination that shows a tight sternocleidomastoid muscle.
- If there is doubt regarding the diagnosis, an ultrasound is obtained. Torticollis looks very distinctive on ultrasound.
- Tumors of the sternocleidomastoid muscle are very rare and can present with a thickening of the muscle. In a patient older than a few months of age with new onset torticollis, a thorough search for a cause (spine conditions, trauma, tumors, certain antipsychotic mediations) should be done.
Treatment (“What will be done to make my child better?”)
- Physical therapy: Aggressive physical therapy exercises under the direction of a physical and occupational therapist will loosen up the muscle over the course of a few months. Most infants do well with this treatment alone.
- Surgery: In rare situations, the condition is discovered late and the sternocleidomastoid muscle is scarred irreversibly. Surgery is required.
- Preoperative preparation: The child should have a shower or a bath the night before or the morning of surgery. The child should not eat anything solid for eight hours before surgery.
- Procedure: It is an outpatient procedure, meaning the child would likely be able to go home the same day of his or her surgery. An incision is made on the affected side of the neck and the muscle is divided.
- Benefits and risks: The risks are small and include infection and bleeding and recurrence of the scarring. The procedure is done as a last resort to prevent the flattening of the skull and the vision problems.
Home Care (“What do I need to do once my child goes home?”)
- If only physical therapy is needed: Parents are taught the physical therapy exercises by the therapist. It is important to keep doing the exercises faithfully as directed by the therapist. Placing attractive objects in the room away from the affected side encourages the baby to look towards that side and complements the regimen of physical therapy.
- If an operation is required
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child will have to resume physical therapy promptly after surgery. Ask the surgeon when therapy should start.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe. Usually wounds are kept dry for three days; shower can resume after that. Soaking the wound (baths, swimming) should wait about one week after surgery.
- Medicines: Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor fever or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow-up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Long-term outcomes are excellent with physical therapy only and rarely is an operation required. Once it is resolved, there are no other future conditions to be concerned about.
Updated: 11/2016
Author: A. Alfred Chahine, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Ulcerative Colitis
Condition: Inflammatory Bowel Disease – Ulcerative Colitis
Overview (“What is it?”)
- Definition: Ulcerative colitis is a chronic inflammatory disease of the colon (large intestine), where the mucosa, or lining of the bowel, becomes inflamed and develops ulcers. Ulcerative colitis (UC) is thought to be due to the body’s immune system over-reacting against the intestine. This results in bleeding and damage to the cells of the colon. The colon becomes less effective in its function of absorbing water and salt.
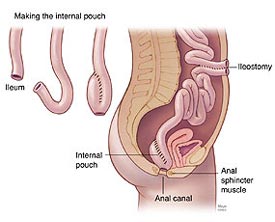 Figure 1.
Figure 1.
- Epidemiology: Ulcerative colitis affects girls and boys equally and is most commonly diagnosed in adulthood (age 30s). However, UC can be diagnosed at any age and occurs in about 2-4 out of every 100,000 people. In children, the inflammation is more likely to affect the entire colon.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: Ulcerative colitis usually presents diarrhea—frequent loose bowel movements that may have blood, mucus and/or pus. The child may have of a constant feeling of needing to move his or her bowels and cramping. Many children have loss of appetite and energy, partly because of a low blood count because of bleeding in the stool. A minority of children will have more severe disease at the time of original diagnosis with fevers, severe abdominal pain and bloody diarrhea. These children have “fulminant colitis” and need more urgent medical, and sometimes surgical, treatment.
- Later signs/symptoms: Many children experience a loss of appetite over time with associated weight loss and decreased energy levels. They may also have trouble sleeping due to frequent bowel movements at night. Additional symptoms that some children experience include delay in bone development and puberty, joint pain, kidney stones, eye irritation and skin lesions.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: The diagnosis of UC is usually suspected based on a combination of history and physical exam findings. It is important for your doctor to try to distinguish between inflammatory bowel disease (Crohn’s and ulcerative colitis) and an infectious cause of diarrhea. Blood tests should be done to check blood count, electrolytes and nutritional markers.
- Plain abdominal X-rays can see the pattern of gas within the intestines.
- Computed tomography (CT) scan may be obtained, depending on the symptoms that the child has.
- Colonoscopy: In this procedure, a flexible lighted telescope is introduced in the anal opening. The doctor is able to see the inner lining of the colon and take pieces (biopsy) of tissue that can be looked at under the microscope. This is how diagnosis is established.
- Conditions that mimic this condition: Crohn’s disease, indeterminate colitis, infectious colitis (Clostridium difficile, Salmonella, Shigella, E.coli and Campylobacter)
Treatment (“What will be done to make my child better?”)
- Medicine: The goal of therapy is to improve symptoms and prevent flare-ups in the future.
- The most common first line therapy for treating UC is steroids, which are used to reduce inflammation. Most children treated with steroids will go into remission, however if steroids are taken for a prolonged period of time there can be significant side effects. If the ulcerative colitis is mostly affecting the rectum and last part of the colon, steroid enemas can be used with much fewer sides effects.
- Other non-steroidal medications, including sulfasalazine, 5-aminosaliciliates (5-ASA) and mesalamine can be used to achieve remission when mild to moderate symptoms are present.
- Azathioprine can be used once remission has been achieved to prevent long-term steroid use
- Infliximab, an antibody against TNF-alpha, has been used in children in both the short and long term to try to reduce the need for steroids.
- Regardless of the medications that are chosen, it is very important to continue to take them to prevent symptom recurrence.
- Surgery
- Preoperative preparation: Ulcerative colitis can be cured by removing the entire colon and rectum, therefore any child with recurrent and severe symptoms should be considered for surgery. Sometimes surgery will need to be performed urgently if there is significant bleeding or severe abdominal distension and fevers. However, usually the surgery can be planned and scheduled non-urgently. Before surgery, the family will meet with the surgeon and often an enterostomal (ostomy) therapist to discuss the best location for a stoma and to answer any questions. If the child is anemic or malnourished this may need to be corrected before surgery with a blood transfusion or additional nutritional support. Sometimes the child will need to have a “bowel prep” before surgery where a hyperosmolar solution is given to clean out the colon.
- Surgery: The goal of the surgery is to remove the diseased colon (colectomy), reconnect the small intestine with the anus (ileoanal anastomosis), and protect the intestine/anus connection from poop as it is healing (ileostomy). Once the colon is removed, there are a variety of ways to pull the small bowel through to the rectum including creating a “pouch” with the small bowel (J pouch vs. S pouch) vs. a straight pull-through. The details of each of these options will be discussed with your child’s surgeon. Most children will have a temporary ileostomy. The child’s stool will be diverted into the ileostomy (bag) to allow the pouch and the connection between the small intestine and the anus to heal.
- There are two approaches to this operation.
- Open laparotomy: The appendix is removed through a midline vertical incision.
- Laparoscopy: In laparoscopic appendectomy, several small cuts (incisions) are made. Through one of the cuts, a video camera is placed. The surgery itself is done using small instruments placed through the other incisions. The usual number of incisions (cuts) for laparoscopic surgery vary from one (single port umbilical) to several.
- Postoperative care: Most children will stay in the hospital for about a week after surgery. Diet will be slowly reintroduced, and if the child is on steroids they will be tapered over a few weeks. The family will be taught how to care for the ileostomy. Usually a second surgery is planned in 2-3 months to close the ileostomy.
Figure 2.
- Risks/Benefits
- Immediate risks: There is always a small risk of injury to the bowel, bladder or other internal organ during the surgery, although this is uncommon. If a small bowel pouch is created there is a risk of leak, but having a temporary ileostomy if thought to minimize this risk.
- Long-term risks: One of the most common problems after creation of a small bowel pouch is inflammation of the pouch or “pouchitis”. This can present with crampy abdominal pain, fever, increased bowel movements and fatigue. This can usually be treated with antibiotics. Occasionally children who have problems after surgery with pouchitis or difficulty gaining weight will be found to have Crohn’s disease or “indeterminate colitis” instead of UC. This may require that the child remain on some anti-inflammatory medications to reduce these symptoms. Other potential problems include a bowel obstruction or stricture that may require dilations or further surgery.
- One of the major benefits of surgery is that this can cure ulcerative colitis. This is especially important for children who have frequent symptoms and problems with weight gain and growth.
Home Care (“What do I need to do once my child goes home?”)
- Diet: There is no specific diet required, however some patients find that avoiding spicy or acidic foods and chocolate helps decrease the number of bowel movements after surgery. Many children have a hard time gaining weight initially after having their colon removed and therefore need a high-calorie diet with a balance of protein, carbohydrate and fat.
- Since the colon’s main function is to reabsorb water, it is important for the child to replace losses in the stool. Using sports drinks that have salt and other minerals is a good drink to keep on hand to avoid dehdydration.
- Activity: Returning to regular activities as soon as possible is encouraged and depending on the type of surgery and the child, this generally ranges from 2-4 weeks.
- Wound care: In general, there is minimal wound care required after surgery. The incisions need to be kept dry for 48 hours. If the child has an ileostomy, there will be education on how to care for the stoma prior to discharge from the hospital.
- Medicines: Most medications that were used prior to surgery will no longer be needed afterwards, but steroids will need to be slowly tapered over several weeks. Most children will be started on medications to reduce the number of bowel movements (either fiber supplements or Imodium®)
- What to call the doctor for: You should seek medical assistance if the child is having persistent fevers, increasing abdominal pain or vomiting, or seems dehydrated (not urinating very often, increased bowel movements, seems very thirsty). It is important to know that DEHYDRATION is the most common reason for readmission in these children.
- Follow-up care: A follow-up visit with the surgeon will be arranged, usually within 2-4 weeks of discharge from the hospital. Follow-up will also be arranged with the gastroenterologist to discuss long-term management and recurrence prevention.
Long Term Outcomes (“Are there future conditions to worry about?”)
Children who undergo surgery for ulcerative colitis for the most part have improved quality of life. However, most patients will have loose and more frequent stools after surgery (5-7 stools at best). Some will have urgency and a degree of incontinence (particularly at night). To get a better outcome, children often need a food diary to regulate their stooling pattern. Children will need to be screened every few years with sigmoidoscopy to ensure that the small amount of rectum that remains does not develop any evidence of cancer.
References
Articles and graphics adapted from:
- Coran: Pediatric Surgery, Seventh Edition, 2012, Elsevier Saunders
- Uptodate, Management of mild to moderate ulcerative colitis in children and adolescents, http://www.uptodate.com
- Rufo: Current therapy of inflammatory bowel disease in children. Paediatr Drugs. 2006; 8(5); 279-302
- New Health Advisor: http://www.newhealthadvisor.com
Updated: 11/2016
Author: Hannah G. Piper, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Umbilical Conditions
Condition: Umbilical Conditions (belly button or navel: hernia, infection, granuloma, drainage)
Overview (“What is it?”)
- The umbilicus (belly button or navel) is a structure in the middle part of the bely. During the development of the baby in the mother’s womb, the umbilical cord connects the baby to the mother. Through blood vessels in the umbilical cord, the mother supplies the baby with nutrients and oxygen and the baby releases waste products.
- After birth, the umbilical cord is cut. The baby takes over the functions of providing nutrition and oxygen for himself or herself, as well as getting rid of waste. In most cases, the muscles around the belly button close within days after birth.
- Definitions
- Umbilical hernia: When the muscles around of the belly button don’t fuse, there is a defect allowing inside contents (such as intestine) to pop out. This usually does not cause the baby pain.
- Umbilical granuloma: Moist tissue causing crusting of the belly button. This can get bigger without treatment. A granuloma does not cause the baby pain.
- Umbilical infection (omphalitis): Infection of the belly button. This can cause pain and discomfort. It represents a serious condition needing prompt medical therapy.
- Umbilical drainage: Fluid coming from the belly button.
- Epidemiology: About 20% of babies have umbilical hernias. About 85% of belly button hernias close on their own by the time the child is about three years of age.
- Umbilical granulomas happen in 1 out of 500 babies.
- Umbilical infections happen in 1 out of 200 babies.
Signs and Symptoms (What symptoms will my child have?”)
- Umbilical hernia: Bulge occurs in the belly button, may get bigger when the baby bears down with increasing pressure in the belly, such as when the baby is crying or bearing down. In extremely rare cases, the contents of the bulge can get stuck in the defect. In this case, the belly button becomes tender and painful. This situation requires the child to be seen immediately—either the doctor’s office or emergency room.
- Umbilical granuloma: Small, round, wet tissue that can happen after the belly button stump falls off.
- Umbilical infection: Redness and swelling around the belly button. The child may have a fever and fussiness. If the infection is uncontrolled, the area of redness may spread to a larger area or have streaks.
- Umbilical drainage: Fluid that comes out of the belly button. If the fluid is yellow and thin, may signal a communication to the bladder (urachal remnant). If the fluid is thick and smells bad, may be an infection. If green, doctors will consider abnormal connection to the intestine.
Diagnosis (“What tests are done to find out what my child has?”)
The conditions that can occur with the belly button are usually pretty obvious on examination. In some cases, if there is a question regarding abnormal connection to the bladder or intestine, an ultrasound may be used. The ultrasound uses sound waves to create an image and does not use radiation.
Treatment (“What will be done to make my child better?”)
- Umbilical hernias: About 85% of belly button hernias close on their own. Since umbilical hernias do not cause pain and rarely get stuck, it is very safe to wait until the child is about three years old to repair a hernia if it has not closed yet.
- Surgery: The goal of the operation is to close the hole in the muscle underneath the belly button. A cut is made around (usually below) the belly button. Stitches are used to close the hole. The skin is usually closed using dissolvable stitches.
- Benefits: Closing the hernia decreases the chance of organs in the belly getting stuck. The hernia is not able to get bigger as the child grows.
- Risks: Bleeding, infection, fluid under the incision. Recurrence of the hernia is rare.
- Preoperative preparation: You may be asked to give the child a bath the night before or the morning of the operation. The child should have nothing solid to eat for at least eight hours before surgery.
- Postoperative care: Most patients are discharged the same day after surgery. The child should be able to tolerate liquids before leaving.
- Surgery: The goal of the operation is to close the hole in the muscle underneath the belly button. A cut is made around (usually below) the belly button. Stitches are used to close the hole. The skin is usually closed using dissolvable stitches.
- Umbilical granulomas
- Medical treatment: Most umbilical granulomas are treated with silver nitrate. Silver nitrate chemically burns the moist tissue, shrinking it and allowing the area to heal. Silver nitrate can burn normal skin as well, so one must be careful to apply the material on the granuloma only. Sometimes, petroleum jelly (Vaseline®) is applied to the normal skin around the granuloma to protect it. Repeated applications of silver nitrate may be needed
- Umbilical infections: Umbilical infections can be very serious, especially in small babies. It is very important to seek medical attention if this is a concern.
- Medical treatment: Antibiotics are medicines that fight bacteria. These can be given by mouth or through the vein depending on how severe the infection is.
- Surgical treatment: If antibiotics cannot control the infection, the child may need to have the pus drained. This can be done by putting a needle in the pus and pulling out the infected fluid, placing a drain, or cutting the skin right over the infection and allowing the pus to drain (incision and drainage). The last option may need to be done in the operating room.
- Postoperative care: If surgical drainage was done, the wound is usually packed with gauze. The packing keeps the wound open, allowing the infected material to drain outside the body. The wound heals from the bottom to the skin. The skin usually takes several days to close.
- Umbilical drainage: The doctors will try to determine the cause of the drainage. Depending on the source, the treatments are different.
- Surgical treatment: If the doctors determine that there is an abnormal connection to the bladder or the intestines, surgery will be needed to find the connection and close it. This is usually done by making a cut by the belly button.
- Benefits: The source of the drainage is found and controlled.
- Risks: Bleeding, infection, fluid under the incision
- Preoperative preparation: You may be asked to give the child a bath the night before or the morning of the operation. The child should have nothing solid to eat for at least eight hours before surgery.
- Postoperative care: Most patients are discharged the same day after surgery or a few days later depending on the extent of surgery. The child should be able to tolerate a regular diet before leaving.
- Surgical treatment: If the doctors determine that there is an abnormal connection to the bladder or the intestines, surgery will be needed to find the connection and close it. This is usually done by making a cut by the belly button.
Home Care (“What do I need to do once my child goes home?”)
- For Umbilical Hernia Repairs
- Diet: Most patients are able to eat a general diet.
- Activity: No activity limitations.
- Wound care: The patient can shower in three days but may want to wait 5-7 days after surgery before soaking the wound.
- Medicines: Medication for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Problems that may indicate infection such as fevers, wound redness and drainage should be addressed.
- Follow-up care: The patient should be seen by a surgeon or pediatrician/family practice doctor at least once to check the surgical wound.
- For Abscess Drainage
- Diet: General diet.
- Activity: No activity limitations
- Wound care: If the child was discharged the same day after the drainage, the packing gauze should be removed the following day. The child may and should shower with soap and water daily. Apply a dry gauze to the area and change as needed.
- Medicines: Medication for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: If the child has such as fevers, wound redness and drainage should be addressed.
- Follow-up care: The patient should be seen by a surgeon or pediatrician/family practice doctor at least once to check the surgical wound.
Long term-Outcomes
Children with umbilical hernias, umbilical granulomas, umbilical infections and umbilical drainage do well. Sometimes, umbilical infections can be severe and may involve removal of skin and muscle. Severe infections can be life-threatening.
Updated: 11/2016
Author and editor: Marjorie J. Arca, MD
Undescended Testicle
Condition: Undescended Testicle (also known as cryptoorchidism)
Overview (“What is it?”)
- Before birth, a male infant’s testicles actually are located within the abdomen (belly). Under the influence of a number of different hormones, the testicles descend into the scrotum just before birth. (See Figure 1)
 Figure 1
Figure 1
- Occasionally, the testicle fails to move completely into the scrotum by the time the baby is born. The testicle remains somewhere in the belly or in the groin area. This condition is called an undescended testicle or cryptorchidism which means “hidden testicle”. (See Figure 2)
- It occurs commonly in preterm males (born before 37 week gestational age) because there is not enough time for the testicle to make its way into the scrotum before birth.
- An undescended testicle occurs in up to 3% of full-term boys and in up to 45% of premature or low birthweight (<2.5 kg) boys.
Signs and Symptoms (“What symptoms will my child have?”)
- Typically, an undescended testicle is noted at birth as an absence of the testicle within the scrotum. It can occur on one or both sides.
- The testicle may be felt in the groin area and present as a groin bulge.
Diagnosis (“What tests are done to find out what my child has?”)
- The diagnosis of this condition is usually confirmed by physical exam performed by a physician or nurse.
- Occasionally, an ultrasound is performed by physicians to evaluate for the presence of a testicle, however this is not considered necessary by most pediatric surgeons and urologists.
- Conditions that mimic an undescended testicle include an absent testicle (the testicle did not develop), ectopic testicle (the testicle is somewhere abnormal outside the normal path of descent), or retractile testicle (a testicle that is pulled above the scrotum by a hyperactive reflex). This can be usually differentiated based on physical exam with or without an ultrasound.
Treatment (“What will be done to make my child better?”)
- Observation: Occasionally, the testicle will descend on its own without any medical therapy. If it does occur, it is most likely to happen by one year of age. After that, studies have shown that the testicle is unlikely to descend without surgery.
- Surgery: The best treatment for an undescended testicle is a surgical procedure to bring the testicle into the scrotum. This is called an “orchiopexy” or “orchidopexy”. (See Figure 2)
- The timing of surgery varies between 6-12 months of age. Your surgeon will recommend the ideal time for surgery.
- If the doctor can feel the testicle in the groin, then an incision is made in the groin and the testicle is freed and brought down into the scrotum. A separate incision is often made in the scrotum in order to place “anchoring sutures” that will hold the testicle in place within the scrotum (See Figure 2).
- If the testicle cannot be felt, then a camera may be inserted through a small incision through the abdomen (called laparoscopy) in order to find its location before proceeding with the rest of the surgery. If it is difficult to get the testicle from the belly to the scrotum, it may take two surgeries to get the testicle into the right spot. The first stage is usually the laparoscopic finding of the testicle and clipping the blood vessels. It is the blood vessels that are foreshortened. The testicle is left in the body for at least six months so the testicle can establish other means of blood supply before getting the testicle into the scrotum.
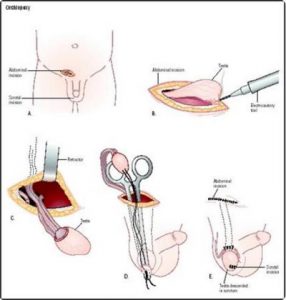 Figure 2
Figure 2
Home Care (“What do I need to do once my child goes home?”)
- Instructions after discharge can vary based on the institution or the surgeon, age of the child, and complexity of the surgery; however, some general principles remain the same.
- In general, the child should be on a normal diet after discharge.
- They should refrain from physical activity as much as possible for at least two weeks.
- The incisions should not be soaked in a tub or pool for one week.
- Your child will likely be given pain medications to home with as well; these should be administered according to the doctor’s prescription.
- Your surgeon will give you specific instructions after your operation which may slightly vary.
- Things to return to the doctor or emergency department for include:
- Fever greater than 38.5 C or 101.5F
- Pus draining from incision
- Increased redness around the incision
- Increased tenderness of the incision
- Inconsolability with food/drink/pain medications
- Decreased urination from usual
- Return of the groin bulge
Long-Term Outcomes (“Are there future conditions to worry about?”)
- In general, the risk of the injury to the testicle is less than 1%.
- Other risks of surgery include bleeding, infection, pain, damage to surrounding structures, recurrent undescended testicle and side effects of anesthesia. These are rare, and the procedure is generally well tolerated.
- It is important to make sure that the testicle remains in the scrotum as the child gets bigger. This should be checked annually during the well child check.
References
- Ashcraft, K. (2010). Ashcraft’s pediatric surgery (5th ed.). Philadelphia: Saunders/Elsevier.
Updated: 11/2016
Authors: J. Prieto, MD; Romeo C. Ignacio, Jr., MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Urachal Cysts
Condition: Urachal Cyst and Sinus
Overview (“What is it?”)
- Definition: The urachus is a structure present during the development of the baby inside the mother. It connects the top of the bladder to the belly button. Normally, the urachus closes down toward the end of pregnancy. If the urachus fails to dissolve completely or partially, a urachal cyst or sinus can remain and cause symptoms.
- A urachal cyst is a leftover structure of the urachus. There is a collection of fluid located under the muscle layers of the belly, just below the belly button and above the bladder. If a connection exists between the bladder and the umbilicus where there is urine draining from the belly button, it is called a urachal sinus.
- Epidemiology: The incidence of urachal remnants is about 1.03% of the population.
Signs and Symptoms (“What symptoms will my child have?”)
- The average age of presentation is four years, but can range from infancy to adolescence.
- Early signs: A sinus can drain urine through the umbilicus without signs of infection. Belly button is noted to be wet constantly, with yellow fluid emanating from the skin fold. There may be a small red opening at the base of the umbilicus.
- Later signs/symptoms: The cyst can become infected, in which case the child has fever, lower abdominal pain, and fullness in the midline in the area below the belly button. As the infection in the urachal cyst progresses, redness may spread over the lower belly. The child may become more ill with signs of systemic infection such as tiredness, vomiting and abdominal pain.
Diagnosis (“What tests are done to find out what my child has?”)
- The pediatric surgeon will be suspicious of the diagnosis after taking a history and performing a physical exam.
- An ultrasound is used to look at the urachus. Sound waves are used to image the urachus or its remnants. Ultrasound is accurate for diagnosis in over 90% of cases.
- A cystogram uses a catheter to instill dye into the bladder to see if a urachus is present.
- Computer tomography (CT scan) or magnetic resonance imaging (MRI) may be obtained depending on the clinical situation.
- The physician may also order blood tests to look for signs of infection.
- The urine may be sent to look for bacterial infection.
- Few conditions mimic urachal cyst or sinus.
Treatment (“What will be done to make my child better?”)
- Medicine: If the urachal remnant comes into attention because of infection, antibiotics (medications to treat infection) are given to the child. Antibiotics may be given by mouth or, if the infection is severe, through the vein.
- Surgery
- A urachal sinus that is draining is removed using a small incision on the underside of the belly button. The sinus is dissected all the way to the top of the bladder and removed there. An alternative approach is to use laparoscopy, where small incisions are used on the abdomen. Through one of these incisions, a video camera is placed. Small instruments are inserted to remove the urachus.
- If an infected urachal cyst does not respond to antibiotics, the pus is usually drained under general anesthesia. Once the infection has resolved, the child may return for a definitive excision of the cyst in about 4-6 weeks. Again, either open or laparoscopic techniques can be used to remove the cyst.
- Controversy exists on whether urachal remnants found accidentally on studies for other conditions should be removed.
- Preoperative preparation: Nothing to eat or drink for eight hours prior to surgery. If the operation is a scheduled (not emergency), a bath or shower the night prior or the morning of the procedure is recommended.
- Postoperative care: Oral or intravenous pain medication may be needed. The child can play and get up after surgery.
- Risks of surgery: General risks of surgery include anesthesia, bleeding, wound infection
- Benefits: If the urachal remnant is eventually excised, it eradicates the risk of infection in the future. There is some thought that urachal remnants may be a site for future cancer, but this is really rare.
Home Care (“What do I need to do once my child goes home?”)
- Most patients may be sent home the day of surgery.
- Diet: A general diet is recommended.
- Activity: The child can be active and play normally. Normal activity will not harm the surgical site. The surgeon will give instructions for bathing. Usually the wounds are kept dry for about three days, then may shower thereafter. No bathing or swimming (activities that would soak the wound) until seven days after surgery.
- Wound care: The surgeon will give instructions.
- Medicines: Usually only oral acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) is prescribed for pain. Sometimes, narcotic pain medication is necessary. If your child is taking narcotics, he or she should take stool softeners to prevent constipation. If antibiotics are prescribed after incision and drainage of an infected urachal cyst, be sure to take all the prescribed pills.
- What to call the doctor for: Any sign of drainage, spreading redness at the surgical site
- Follow-up care: Usually your surgeon will have you make an office appointment for 2-4 weeks after surgery.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Once a urachal cyst or sinus is excised and the surgical site has healed, the problem is completely resolved. It is rare to have any long-term issues.
- There are rare reports of complete resolution of infected urachal cysts after laparoscopic drainage, without need for further operation. This should be discussed in detail with your surgeon.
Updated: 11/2016
Author: Joanne E. Baerg, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Vascular Rings
Condition: Vascular Rings
Overview (“What is it?”)
- Vascular rings are developmental anomalies that affect the aortic arch and the major blood vessels that arise from it. The aorta is the biggest artery (blood vessel) that arises from the heart. Usually these problems cause compression of the trachea (windpipe) and the esophagus or both. Sometimes these blood vessel abnormalities form a complete ring around the trachea and esophagus, and in other cases the ring may be incomplete but still be enough to cause symptoms. The various types of vascular rings may be complex.
- During normal development there are two arches to the aorta as it leaves the heart, and the right arch usually goes away. When it does not, this leaves a double aortic arch and if only parts of either of the two arches don’t regress as they are supposed to, many of the various types of ring anomalies arise.
- Other types of vascular rings include pulmonary artery slings. This occurs when the left pulmonary artery originates from the right pulmonary artery instead of the main pulmonary artery as it comes out of the heart. The abnormal left pulmonary artery passes between the trachea and esophagus and causes compression.
Signs and Symptoms (“What symptoms will my child have?”)
- Vascular rings usually cause symptoms because the abnormal blood vessels press on the trachea, esophagus or both and cause narrowing of that structure. This narrowing may cause problems breathing or swallowing. A child may stop breathing (apnea), have wheezing if the airway is compressed, or problems with vomiting or persistent spitting up if the esophagus is involved. Some infants may have recurrent respiratory infections. Other problems include difficulty feeding, failure to gain weight and grow.
- Sometimes, an infant will be fine when taking only formula and liquids and then have problems with swallowing when more solid food is introduced. Most of the time, symptoms occur sometime in the first year of life, often in the first several weeks or months. Surgical correction may needed at that time. Double aortic arches can cause symptoms early on. Some children with mild symptoms may outgrow the symptoms: however, the anatomy never becomes normal.
- Some children may never have symptoms only to become symptomatic as adults when they have hardening of the arteries (atherosclerosis) and symptoms become more apparent.
Diagnosis (“What tests are done to find out what my child has?”)
- A variety of studies may be used to make the diagnosis of a vascular ring. These may include X-ray studies called an esophagram looking at changes in the shape of the esophagus that suggested a vascular ring. An esophagram is a test where the patient is made to drink liquid contrast, and X-rays are taken during the swallowing process.
- Magnetic resonance imaging (MRI) and computed tomogram (CT) scan with contrast look at the blood vessels themselves to make the diagnosis. These studies provide excellent anatomic definition for the surgeon.
- Computed tomography (CT) scans: Detailed pictures of the chest reconstructed in different views to get a better picture of the liver mass.
- MRI (Magnetic Resonance Imaging): Uses a magnet, radiowaves and computer to obtain images of organs in the body. MRI does not use radiation
- Bronchoscopy: This study requires anesthesia. A telescope is placed through the vocal cords to look at the windpipe and the airways.
- Cardiac catheterization may be necessary in some cases. If the anatomy of the vessels are difficult to show on the other imaging modalities, then direct injection of contrast into the heart will show the flow of blood from the heart to the blood vessels.
- Breathing and swallowing problems can be caused by a wide variety of other problems most of which are more common than vascular rings. Making the diagnosis of a vascular ring requires someone to think of the problem as a potential cause of the child’s symptoms and then order the appropriate tests.
Treatment (“What will be done to make my child better?”)
- Surgery is the only way to take care of a vascular ring and is indicated for any patient who has one and is symptomatic. Failure to treat the ring can lead to serious problems including inability to eat well, causing weight loss or poor weight gain. Respiratory symptoms may be as severe as apnea (not breathing for a short duration) or hypoxia (lack of adequate oxygen). Sudden death has been reported. The type of surgery needed depends on the vascular ring diagnosed and to some extent the preference and experience of the surgeon. Many of these require an open thoracotomy (incision in the chest) between the ribs. However, there are several types that are amenable to thoracoscopic repair. In thoracoscopy, several small cuts (incisions) are made. Through one of the cuts, a video camera is placed. The surgery itself is done using small instruments placed through the other incisions. The usual number of incisions (cuts) for thoracoscopic surgery vary.
- Surgery is very safe when performed by an experienced surgeon and surgical team. Some of the risks include injury to the nerves that control the vocal cords (voice box). These nerves are specifically looked for during surgery but may have to be moved a bit in order to take care of the vascular ring. This can cause a soft voice or cry in babies after surgery but this will get better in several weeks, if it happens. Another possible problem is a lymph leak in the chest after surgery. This is due to drainage of clear fluid from lymphatic ducts in the chest. While this is not common, it can be a difficult problem to take care of and involve dietary measures, medicine or even further surgery.
Home Care (“What do I need to do once my child goes home?”)
- The care at home will to some extent depend on the type of surgery that was needed and the age of the child when the surgery was done.
- For repairs done thoracoscopically, children can return to normal activity as soon as they are able.
- For open thoracotomy, activity may be more limited in older children as their wound heals and pain medicine may be needed longer.
- There is no special diet.
- The only medicine needed is pain medication for only a short period of time.
- If narcotics are used, constipation may occur. Stool softeners should be used if narcotics are being taken.
- Acetaminophen (Tylenol®) or Ibuprofen (Motrin® or Advil®) may also be used for mild to moderate pain
- What to call your doctor: Fevers, trouble breathing, redness of the wound, drainage from the wound.
- Follow-up: Your surgeon will be see you in clinic a few weeks after surgery to make sure that wound is healing well.
Long-Term outcomes (“Are there future conditions to worry about?”)
- Sometimes, respiratory symptoms take months to resolve completely because the trachea was narrowed by the vessels and, in a sense, molded to the narrowed shape. Reshaping of the trachea requires growth with time to resolve the narrowing. Sometimes even swallowing problems take some time to fully resolve.
- When corrected, vascular rings do not shorten life span, and children should make a full recovery with excellent long-term function.
Updated: 11/2016
Author: John H.T. Waldhausen, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Wilms Tumor
Condition: Wilms tumor (aka nephroblastoma)
Overview (“What is it?”)
- Definition: Wilms tumor is the most common cancer of the kidney seen in infants and children. It is made up of tissue that comes from immature cells of the kidney. Wilms tumor is named after Dr. Wilms, a pathologist who first described the tissues from which this tumor arises.
- Epidemiology: About 500 cases are diagnosed in the United States per year, representing a little more than 10% of all childhood cancers. It is the second-most common solid tumor in infants and children. The average age of the patient at presentation is three years of age, most commonly seen between six months to eight years of age.
Signs and Symptoms (“What symptoms will my child have?”)
The most common presentation is a firm, large, non-painful abdominal mass, commonly felt by a parent during a bath or a pediatrician during a well baby check. The child may also have high blood pressure or blood in his or her urine on presentation. Other findings may include weight loss, loss of appetite or decreased energy level.
Diagnosis (“What tests are done to find out what my child has?”)
- When a doctor is concerned that a child’s abdomen is distended, he or she may request several imaging studies. A belly X-ray may distinguish whether the distention is due to intestinal problems. If a mass in the abdominal organs such as the kidney is suspected, a computed tomography (CT) scan is performed. This test can definitively pinpoint the origin of the mass and may show whether the mass has extended beyond the kidney or spread into surrounding tissues such as the lymph nodes, the adjacent blood vessels. In addition, it is important to determine whether there are lesions suspicious for cancer in the other kidney. The CT will determine whether removal of the tumor is safe for your child (tumor resectability); sometimes, if the tumor is really big and surrounds organs and structures that are critical, its primary removal may not be safe for your child.
- Wilms tumors can spread to the lungs as well, so a CT of the lungs is typically performed.
- An ultrasound is a more sensitive test to see whether there is tumor in the veins next to the kidney. Knowledge of the extent of the tumor (one kidney vs both kidneys, outside tumor spread into the lymph nodes, lungs or blood vessels) is important.
- The spread of the tumor affects the type and order of treatments. For example, a tumor that is confined to one kidney only may be treated by surgery alone, but if there is spread of the tumor, chemotherapy may be the first treatment that should be done to get the best outcomes for your child.
- Labs and tests: Bloodwork will be drawn to determine the child’s general health including the blood count (red cell count) and the function of the kidney. The spread of the tumor determines the “stage” of the tumor.
- Conditions that mimic this condition: Other tumors or growths arising from the kidney and other abdominal organs such as the liver can mimic Wilms tumor. Therefore, X-rays are very important to confirm the diagnosis
Treatment (“What will be done to make my child better?”)
- Surgery: The type of operation needed for Wilms tumor depends on the extent or spread of the tumor. If the tumor is all within the kidney and no spread is seen outside of the kidney, removal of the involved kidney may be the only treatment needed. If the tumor is in both kidneys, or has spread into the vena cava (large vein next to the kidney) or the lungs, the initial treatment may not be surgery. In these cases, a biopsy of the tumor is needed to see what type of tumor (aggressive or not aggressive) exists. At the same time, a catheter is placed into the central vein of your child to allow infusion of medications that fight cancer (chemotherapy). In situations where the tumor is aggressive or it goes beyond the confines of one kidney, chemotherapy has been shown to make the overall outcome better for the child. Once the tumor shrinks, then definitive surgery to remove the main tumor is performed.
- Preoperative preparation: As already mentioned, X-rays to determine whether the tumor is resectable or whether primary removal of the tumor is the right thing for your child. Depending on the complexity of the surgery, preparation for the possibility of blood transfusion may be done.
- Postoperative care: Your child may require some days in the Intensive Care Unit, depending on the extent of the surgery.
- Important miscellaneous Issues: The prognosis of Wilms tumor depends on many factors including your child’s age, the size (weight) of the tumor, the aggressiveness of the tumor cells as determined by their properties (will be tested by the pathologists) and tumor spread. Depending on any and/or a combination of these factors, your child may need surgery alone; a combination of surgery, chemotherapy and radiation; or even stem cell transplant. Your child’s surgeon and cancer doctor (oncologist) will discuss these options with you as they become aware of the information about the tumor and its properties.
- Medicine: The medicines that will be part of your child’s chemotherapy regimen will be discussed with you by his or her oncologists. Each medicine has its side effects that can affect your child in both the short term and long term. Be sure that you are aware of these issues during the discussion.
- Risks/Benefits: Risks of surgery include bleeding (which may require transfusion), infection and damage to surrounding organs.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Usually the child can be on a regular age-appropriate diet when he or she goes home. However, during chemotherapy, the child may lose interest in eating. To keep up his strength, sometimes the child may need supplementation of nutrition using a feeding tube (tube that goes from the nose to the stomach) or a venous catheter (PICC® or central line). This issue should also be addressed by the oncologist.
- Activity: If your child had a biopsy only, regular activity can be resumed about two days after surgical procedure. If he or she had a large incision (could be up-and-down or side-to-side incision), then he/she may need to decrease vigorous activity (jumping, running, climbing, contact sports) for about 3-4 weeks while he or she is healing.
- Wound care: Dressings will be removed in 48 hours. No further dressing is required, unless you prefer a dry dressing. Usually, the wound has to be kept dry for about three days. After this, the child can shower, but he or she should not soak the wound for about one week after surgery.
- Medicines: Pain medicines will be given. If the pain medications required are in the narcotic family, then constipation is a significant side effect. Stool softeners should be given to prevent this complication.
- In patients with cancer, especially those who are on chemotherapy, acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) should be avoided as fevers due to infection may be masked.
- What to call the doctor for: A call to the surgeon should be done if there is worry about infection (unexplained fevers, redness and drainage of the wound(s), vomiting or inability to have bowel movements. Your child’s oncologist will likewise give you instructions about when to call their clinic.
- Follow-up care: A wound check is often performed in 2-3 weeks after surgery. Often, the child’s oncologist can also provide follow up of the wound as well.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Future outcomes from Wilms tumor depend on the aggressiveness and spread (stage) of the tumor. Long-term outcomes may also be affected by side effects of the chemotherapy. It is best to have these individualized discussions with your child’s oncologist and surgeon.
Updated: 11/2016
Author and Editor: Marjorie J. Arca, MD