CONDITIONS A - E
These pages offer explanations of pediatric medical surgical conditions including:
- what the condition is
- signs and symptoms
- how it is diagnosed
- treatment
- home care
- long-term outcomes
Use it as a reference when discussing your child’s individual condition and treatment with your doctor and medical professionals.
Achalasia
Condition: Achalasia (esophagus)
Overview (“What is it?”)
- Definition: Achalasia (from the Greek “chalasis” meaning slackening) is an abnormality that may explain problems in swallowing. The esophagus is the tube that connects the mouth to the stomach and is made up of muscle layers. The region between the esophagus and the stomach is defined by a slight tightness in the muscle called the lower esophageal sphincter. In achalasia, there are two problems: (1) the muscles of the esophagus that move food from the mouth to the stomach do not work, and (2) the lower esophageal sphincter (LES) does not relax completely. The combination of non-working esophageal muscles and a tight LES cause the food to get stuck in the esophagus.
- Etiology: Most cases of achalasia have no defined cause (idiopathic).
- Epidemiology: Achalasia occurs in 1-2 people in 200,000. It is most common in adults mostly between ages 30 to 50. About 10% of all patients with achalasia are children and teenagers
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: Patients with achalasia may present with coughing at night. When laying flat, food and spit may collect in the esophagus. Food and spit may spill in the airways and lungs. Symptoms of achalasia include problems swallowing, vomiting undigested food and chest pain behind the sternum. Because undigested food remains in the esophagus for a long time, bad breath and foul-smelling burps can be observed.
- Later signs/symptoms: If the child has continued vomiting, he or she may exhibit weight loss.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: The diagnosis of achalasia is usually diagnosed with a combination of an esophagram and measurements of esophageal manometry and motility. An esophagram is a test where the patient is made to drink barium and X-rays are taken during the swallowing process (See Figure 1). Findings of this study show a large, non-moving esophagus with a closed off (beaked) esophagus (See Figure 2). Esophageal manometry measures the pressure within the LES and esophageal motility measures movement of the esophagus. A physician places a small tube into the esophagus to measure these characteristics. In achalasia, (1) the LES pressure is high and (2) there is no effective movement of the esophagus that pushes food from the stomach. These two main problems cause food to stay in the esophagus instead of going in to the stomach. Endoscopy is when a flexible telescope is placed in the mouth and is gently pushed through the esophagus, stomach and part of the small intestine. The doctor can look at evidence of inflammation directly. This study is used to make sure that there are no other reasons for the child’s symptoms.
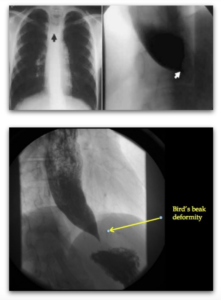 Figure 1: Chest x-ray shows an air-fluid level in the middle of the chest (arrow) in a patient with achalasia.
Figure 1: Chest x-ray shows an air-fluid level in the middle of the chest (arrow) in a patient with achalasia.
Figure 2: Upper gastrointestinal study demonstrating a “bird’s beak” deformity (arrow) in a 17 year-old patient with achalasia. (Image provided by R. Ignacio 2016)
- Conditions that mimic this condition: Because patients present with vomiting and aspiration, patients can be thought to have gastroesophageal reflux. In South America, a parasitic disease called Chagas’ disease causes injury to the nerves of the esophagus and therefore cause the similar symptoms.
- Diffuse esophageal spasm: Diffuse esophageal spasm is even less common than achalasia. Symptoms of this disorder are similar to symptoms seen with achalasia. Patients present with a long-standing history of swallowing problems, regurgitation of undigested food, bad breath and weight loss.
Treatment (“What will be done to make my child better?”)
- Medicine: Medications that decrease the pressure the LES (examples:calcium channel blockers such as nifedipine and nitrates) have unpredictable effects on symptoms.
- Endoscopy:
- Dilation: The LES can be opened forcefully by inflating a balloon within the esophagus during endoscopy. This maneuver stretches the circular fibers of the LES. It can achieve some resolution of symptoms over weeks or months. Dilation has about a 2-6% risk of perforation.
- Injection of botulinum toxin (Botox): Botox is a substance that has been used in several conditions to achieve muscle relaxation (most commonly to decrease the appearance of facial wrinkles). Botox can be injected into the esophageal sphincter muscles in achalasia to effect relaxation of the muscles. The effect lasts about three months.
- Surgery: Surgical treatment of achalasia is the only modality that results in lasting results. In this procedure, called an esophageal myotomy or Heller myotomy (Dr. Heller is the surgeon who described the procedure first), the surgeon creates an incision through the (LES) effectively releasing the circle of the sphincter and loosens up this tight region. The opening in this region allows food to pass from the esophagus to the stomach, but it also increases the likelihood of having food pass from the stomach to the esophagus (gastroesophageal reflux). In order to avoid reflux of food and acid to go from the stomach to the esophagus, surgeons create a partial fundoplication, where part of the stomach is wrapped around the lower esophagus. At the time of the operation, some surgeons may require having a specialist (gastroenterologist) put a telescope in the esophagus to make sure that the surgery is successful. The operation can be done with a large vertical cut through the middle of the upper abdomen from the bottom of the breastbone to the belly button. Another way of doing the surgery is through laparoscopy, where small incisions that allow a scope and instruments to be inserted into the belly. This second approach results in a faster recovery and smaller scars. It is important to know that the surgery opens up LES, but does not do anything to correct the abnormal movement of the esophagus. There is no surgery to help the movement of the esophagus.
- Preoperative preparation: Patients are usually asked to shower or bathe on the night before surgery. Patients are asked to stop eating or drinking for a few hours before surgery.
- Informed consent: A consent form is a legal document that states the tests, treatments or procedures that your child may need and the doctor or practitioner that will perform them. Before surgery, your doctor should tell you what the operation is, the goal of the surgery and other possible treatment options that are available. Your doctor should explain the risks and benefits of the surgery. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your child’s medical care in words you know. Before you sign the consent form, make sure all of your questions are answered. It is important to know that during surgery, there are things that can happen that your doctor may have not predicted before going in. He or she will explain these to you after the surgery.
- Emotional support: Stay with your child for comfort and support as often as possible while he or she is in the hospital. Ask another family member or someone close to the family to stay with your child when you cannot be there. Bring items from home that will comfort your child, such as a favorite blanket or toy.
- IV: An IV is a small tube placed in your child’s vein. Caregivers use the IV to give your child medicine or liquids.
- Postoperative care: After surgery, some surgeons may require the patient to have an X-ray where the patient swallows contrast to make sure that there are no small leaks in the esophagus. In addition, this study may show that contrast travels from the esophagus to the stomach, showing that the surgery was successful.
- Foley catheter: This is a tube that may be put into your child’s bladder to drain his urine into a bag. The bladder is an organ where urine is kept. The foley catheter is usually taken out shortly after the surgery.
- Nasogastric tube: The surgeon may want a nasogastric (NG) tube inserted through your child’s nose and down into his stomach. This tube keeps air and fluid out of the stomach during surgery and immediately after
- Preoperative preparation: Patients are usually asked to shower or bathe on the night before surgery. Patients are asked to stop eating or drinking for a few hours before surgery.
- Risks/Benefits: In this procedure, the surgeon makes an incision through the muscle layer only of the LES and not the inside lining of the esophagus. In about 2% of cases, the internal layer of the esophagus is opened (perforation). It is usually recognized at the time of the operation and repaired. If this were to happen, the surgeon may delay feeding the patient for some time to allow the repair to heal.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Most patients are instructed to eat a soft diet for several days after the surgery. When they are advanced to a general diet, they are to continue eat with small bites and chew thoroughly.
- Activity: If the patient had the procedure with small incisions (laparoscopic), he or she can be back to normal activity in 1-2 weeks. If the surgery is done through a big incision, then he or she can be back to normal activities in six weeks, with a weight restriction of 10 pounds up until that time.
- Wound care: The patient can shower in three days but may want to wait 5-7 days after surgery before soaking the wound.
- Medicines: Medication for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Sometimes, if the patient has heartburn symptoms, medications to decrease the acidity of the stomach (antihistamine blockers such as ranitidine and proton pump inhibitors such as omeprazole) may help. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: After discharge from surgery, problems that may indicate infection such as fevers, wound redness and discharge should be addressed. If there is a lot vomiting, chest pain or food getting stuck in the esophagus, the surgeon should be contacted.
- Follow-up care: The patient should be seen by a surgeon at least once to check the surgical wound. The patient’s gastroenterologist may require multiple visits for months to years to make sure that the patient remains symptom free.
Long-Term Outcomes (“Are there future conditions to worry about?”)
After surgery, patients may have bad heartburn symptoms. Heartburn usually means that there is acid that is going up the esophagus. When acid from the stomach contacts the esophagus for a long time, the esophagus is harmed. The esophagus can get narrow, inflamed or even have a higher risk of cancer. Patients with achalasia have a higher chance of getting esophageal cancer compared to the general population. It is important that the esophagus is examined by telescope (endoscopy) to make sure that inflammation or cancer is not happening. However, there are no guidelines as to how often or for how long these endoscopies should be performed.
Updated: 11/2016
Author: Marjorie J. Arca, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Acute (Early) Appendicitis
Condition: Acute (Early) Appendicitis
Overview (“What is it?”)
- Definition: Inflammation/Infection of the appendix. The appendix is a small extension of the intestine that is connected to the large intestine (colon). The appendix is usually located in the right lower side of the belly, and it is tubular in shape. Its length differs based on the age. The appendix has no known important function. Appendicitis is inflammation and infection of the appendix and often results from blockage of the appendix by stool (feces). Sometimes, the feces form a small stone called a fecalith. Other causes of appendicitis include swelling of lymph tissues within the appendix wall because of recent infection. Sometimes worms can also block the appendix. Once blockage of the appendix occurs, several things happen:
- The appendix cannot empty the mucus and fluid that it makes.
- The pressure in the appendix increases and it swells.
- Bacteria multiples inside the appendix.
- The swelling cuts off the blood supply to the appendix. If the infection continues, part of the appendix wall dies and a hole results. This is how ruptured or perforated appendix happens.
- Incidence: There are 70,000 appendicitis cases in kids per year in the United States. Overall, 7% of people in the United States have their appendix removed during their lifetime.
Signs and Symptoms (“What symptoms will my child have?”
- Early signs and symptoms: When inflammation in the appendix begins, there is pain around the middle of the belly near the belly button. The child may have decreased appetite and feels like vomiting. The pain never completely goes away and becomes sharper with time. Most children with appendicitis have a fever of 38°-39° C (100.5° – 102°F).
- Later signs and symptoms: More than 24 hours after the pain starts, it moves to the right lower side of the belly. Sometimes, a child complains of right lower abdominal pain while walking, or refuses to stand up or walk due to pain. Younger children (younger than five years old) have a higher chance of having ruptured appendicitis because they may not be able to talk clearly about their symptoms. If the appendix ruptures, a high fever may be seen. There may be episodes of diarrhea.
Diagnosis (“What tests are done to find out what my child has?”)
- History: The doctor will obtain a history and perform a physical exam. This is important for diagnosis of appendicitis. The surgeon will be interested in the type and location of pain: right lower side that hurts with jumping, walking or other jarring movements. The doctor will ask whether the child may have nausea, vomiting, refusal to eat, fever or diarrhea.
- Physical examination: Includes a careful abdominal examination performed by the surgeon. Other medical problems that cause belly pain will be investigated.
- Laboratory tests: Bloodwork may be sent to look at suggestion of an infection. Urine may be tested for a bladder infection or a kidney stone. Female teenagers should have a urine pregnancy test.
- Diagnostic studies: In some cases, the child’s story and the examination by the doctor may be very convincing that appendicitis is present. If the diagnosis is not clear, other tests may be ordered:
- Chest X-ray: If there is a concern for pneumonia
- Abdominal X-ray: A belly X-ray looks for clues regarding what may be causing the pain in general.
- Ultrasound: Ultrasound is very helpful to diagnose appendicitis. A probe is placed over the belly and sound waves are used to look at the appendix. Ultrasound may be useful for girls to look at the ovaries.
- Computed tomographic (CT) scan: CT is most useful when the diagnosis is not clear or if ruptured appendicitis suspected. Unlike ultrasound, CT scans use radiation to obtain images. The child may be asked to drink a liquid that outlines the stomach and intestines. Sometimes, the contrast is given through the rectum. In some cases, an IV medicine is needed to help the CT get better pictures leading to a more accurate diagnosis.
- Conditions that mimic appendicitis: Gastroenteritis (stomach flu), constipation, ovarian cyst, twisting of ovary (torsion), groin (inguinal) hernia, pneumonia, Meckel’s diverticulum, inflammatory bowel disease, kidney diseases, urinary tract infection, intestinal obstruction, pregnancy. It is important to note that:
- Children with history and physical exam findings that are convincing for appendicitis may not need any further tests.
- In children with unclear cause of belly pain, there are several possibilities.
- If the diagnosis of appendicitis is not clear, the doctor may recommend observation in the emergency room or hospital for a period of time. A doctor will examine the child every few hours to see if the pain gets better or worse.
- Ultrasound or CT may be done depending on the situation.
Treatment (“What will be done to make my child better?”)
- Since appendicitis is an infection, antibiotics are an important part of the treatment. Antibiotics are medicines that fight bacteria. It is given through the vein.
- There is some evidence that show that early appendicitis may be treated by antibiotics alone. This requires a definite diagnosis of appendicitis with CT or ultrasound. In the US, this option is only done under a study or a trial. The exact treatment (days in the hospital, how many days of antibiotics are needed) and risks of using antibiotics alone should be carefully discussed with your surgeon.
- Fluids are needed for patients with appendicitis. Since appendicitis causes loss of appetite, the patient may be dehydrated. Fluids are usually given through the vein.
- Medicine is also given to the patient to help make their belly pain better.
- Surgery: The standard way to treat appendicitis is by removing the appendix (appendectomy). This can be done the traditional way (open or larger incision) or laparoscopic.
- Open appendectomy: The appendix is removed through a transverse open incision in the right lower part of the belly.
- Laparoscopic appendectomy: In laparoscopic appendectomy, several small cuts (incisions) are made. Through one of the cuts, a video
camera is placed. The surgery itself is done using small instruments placed through the other incisions. The usual number of incisions (cuts) for laparoscopic surgery vary from one (single port umbilical) to three. Sometimes an extra cut is needed if the appendix is really ruptured and stuck. The placement of the incisions depends on the location of the appendix. - Open and laparoscopic appendectomy take the same amount of time to perform. One benefit of laparoscopy is that other abdominal structures can be examined using the video camera during surgery. Laparoscopy also has lower risks of wound infection.
- Preparation for surgery: Your child will be given fluids, antibiotics, pain medicine prior to surgery.
- Postoperative care
- Activity: Typically, the child is encouraged to walk around as soon as possible.
- Diet: In patients with early appendicitis, patients are started on liquids after their surgery then advanced to a general diet.
- Medicines: Your child may need any of the following:
- Antibiotics to help prevent or treat an infection caused by bacteria.
- Anti-nausea medicine to control vomiting (throwing up).
- Pain medicine which can include acetaminophen (Tylenol®), ibuprofen (Motrin®), or narcotics. These medicines can be given by vein or by mouth.
Home Care (“What do I need to do once my child goes home?”)
- Patients with acute appendicitis are usually discharged the same day as their surgery or the following day.
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after laparoscopic surgery, 4-6 weeks after open surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol®) or ibuprofen (Motrin® or Advil®) or something stronger like a narcotic may be
needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain. - What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, diarrhea, problems with urination, or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow-up with his or her surgeon 2-3 weeks after surgery to ensure proper post-operative healing.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Prognosis is excellent after surgery.
- Complications
- Wound infection: Happens around 3% of the time. Infections may need only antibiotics or may require opening up of the wound depending on how bad the infection is.
- Abscesses (pus pockets): Happens about 10-20% of the time with ruptured appendicitis. If the abscess is small, antibiotics may treat it. If it is big, it may need to be drained. The technique is the same as described in the section Ruptured Appendicitis with Abscess
- Small bowel obstruction: 3-5% risk after appendicitis and appendectomy.
Updated: 11/2016
Author: Joanne E. Baerg, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Adrenal Tumors
Condition: Adrenal Tumors
Overview (“What is it?”)
- Definition: The adrenal gland is an organ in the body that makes hormones. Hormones are substances in the body that helps in many different functions. A type of hormone the adrenal gland makes is adrenalin (epinephrine) and similar types of hormones. This class of hormones helps maintain blood pressure and heart rate. Adrenalin also helps us run or fight when we are threatened. The adrenal gland also makes other hormones like steroids. These steroid-like hormones that help us maintain our growth (cortisol), kidney function (aldosterone) and sexual development (estrogen and testosterone). (See Figure 1)
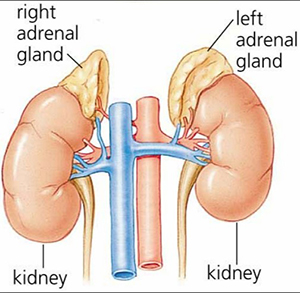
Figure 1: Adrenal glands located above each kidney.
- Tumors can come from tissue that produces either type of hormone (adrenaline family or steroid family). These tumors can be either benign (not cancerous, in terms of not being able to spread through the body) or malignant (cancerous). Another name for benign tumor is adenoma. Tumors from the part of the adrenal gland that makes adrenaline are also called pheochromocytomas. Pheochromocytomas can be benign (more common) or malignant. In babies and young children, there is a type of tumor that can also arise from the adrenal gland called a neuroblastoma.
- Epidemiology: These tumors are rare. The cancers that make steroid-type hormones account for only 0.2% of cancers in kids. Benign tumors are slightly more common than malignant tumors. Neuroblastoma is the most common tumor arising from the adrenal gland.
Signs and Symptoms (“What symptoms will my child have?”)
- Many of these patients will have high blood pressure or a fast pulse rate. In some patients, the tumor may become big enough to cause distention of the belly. Some of the patients will have problems because of effects of too much hormone. This may result in abnormal hair growth, facial hair growth, early puberty or breast development. Some patients may become fat or get bad stretch marks. Sometimes, these tumors have no symptoms. The mass is seen in an X-ray that was being done for another reason.
Diagnosis (“What tests are done to find out what my child has?”)
- Urine and blood will be collected to see if the tumor is making abnormally high levels of hormone. The hormones that can be elevated are the adrenaline family or the steroid family. There are some tumors that do not make any hormones at all.
- X-ray tests are performed which help us know how large the tumor is and whether it has spread to lymph nodes or distant sites. Ultrasounds, chest X-rays, CT scans (See Figure 2) and MRIs may all be used to help diagnose and treat your child. Sometimes, nuclear medicine scan can help to figure out what type of tumor is in the adrenal gland.
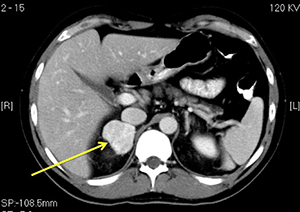
Figure 2: CT scan demonstrating a right adrenal mass (arrow). (Image provided by R. Ignacio 2016).
Treatment (“What will be done to make my child better?”)
- It is important to know if the adrenal tumor makes adrenaline. If it does, medicines to control the blood pressure and the heart rate are needed to make surgery safe.
- After the tests have been analyzed, the tumor will be removed. All adrenal tumors in kids are taken out. This helps us to determine whether the tumor is cancerous or not. It also helps determine if chemotherapy or radiation is needed so the tumor would not come back.
- Risks/Benefits: Include bleeding, infection and return of the tumor.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child’s diet should be normal after they return home.
- Activity: Recovery from surgery usually takes about a month. After the recovery period, no restrictions in activity will be needed after the surgical wounds have healed.
- Wound care: Sponge baths can be given shortly after the operation. The wounds can be washed with sponge baths. Regular baths can be given after about one week.
- Medicines: Stool softeners, laxatives and pain medications may be prescribed for your child.
- What to call the doctor for: Call the doctor or seek medical attention if your child has fever, redness around the wound, inability to stool or keep fluids down or vomiting.
- Follow-up care: Your child should be followed regularly by your endocrinologist or cancer doctor to make sure that the tumors don’t come back.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Most of the tumors that make adrenaline are benign. A few are malignant and will need to receive chemotherapy.
- Tumors that make steroid hormones are harder to assess. Sometimes, the differences between the cancerous tumors and those that are not cancer are difficult to determine, even after the tumor is examined under the microscope. Your doctor will discuss with you how your child will be monitored for tumor recurrence. If the tumor appears to be cancerous, the child may require chemotherapy.
References:
Alagille Syndrome
Condition: Alagille Syndrome (paucity of bile ducts, hyperbilirubinemia)
Overview (“What is it?”)
- Definition: A syndrome is a type of disease in which the baby has several abnormalities. In Alagille’s syndrome, one of the main problems is that there are fewer than normal number bile ducts in the liver. The liver cells make bile, a yellow liquid that the body needs to help digest food that a person eats. The bile is transferred from the liver cells into the intestine through bile ducts. The bile ducts start out small in the liver, then join together like smaller twigs that join into larger and larger branches making up the main bile ducts or channels that bring the bile from the liver into the intestine. In Alagille’s syndrome where there is few number of bile ducts, the bile gets backed up in the liver (See Figure 1). The baby’s skin and the whites of the eyes can turn yellow (jaundice).
- Children with Alagille’s may also have other abnormalities such as heart defects, abnormal vertebrae/spine bones, lung artery abnormality, characteristic facial features and an enlarged liver.
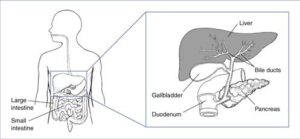
Figure 1: Structure of the liver and the bile ducts. Patients with Alagille Syndrome have fewer bile ducts to drain bile. National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
- Epidemiology: An estimated 1 in every 70,000 children born will have this disorder. This is a genetic disorder in which there is an abnormality in a gene which is passed onto the child by the parent.
Signs and Symptoms (“What symptoms will my child have?”)
- Because of the bile duct problem, the baby may have yellowing of the whites of the eyes and skin. As the baby gets older, the liver can get very big and does not work well. With poor liver function, the child can have belly pain, itching, dark (brown) urine and light (grey-colored) stool. The child may have poor appetite, feel like queasy or sick and poor growth/weight gain.
- The facial features that may be seen are shown below. The face can have a broad, prominent forehead, deep-set eyes, and a small, pointed chin. (See Figure 2 from The Childhood Liver Disease Research Network – https://childrennetwork.org/ags-p.aspx)
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: Bloodwork to measure the function of the liver and the level of bile in the blood stream. Ultrasound is a test that can look at the liver and the gallbladder to look for other reasons that can cause jaundice such as stones in the gallbladder, abnormality of the large bile ducts, or a tumor of the liver. A HIDA scan is a nuclear medicine test that looks to see if bile from the liver makes it into the intestine. Eventually, the child may need to have surgery to biopsy the liver and to inject some dye into the bile ducts to see if there is a blockage. Most children will also get a heart ultrasound and X-rays of the spine to help with the diagnosis. There are also eye abnormalities that are seen only in Alagille’s syndrome, so an eye specialist may need to look at the patient’s eyes.
- Conditions that mimic this condition: Biliary atresia, viral hepatitis, cystic fibrosis, hypothyroidism, alpha-1 antitrypsin deficiency.
Treatment (“What will be done to make my child better?”)
- Medicine:
- Correction of vitamin deficiency. Some vitamins are not absorbed when the liver is not working well (vitamin A, D, K, E)
- Medicines to treat itching (Diphenhydramine, hydroxyzine, or cholestyramine)
- Standard immunizations
- Dietary modifications (high carbohydrate and medium chain fatty acids)
- Surgery:
- Most children will undergo a liver biopsy to confirm the diagnosis. A biopsy is when a piece of liver is taken and studied to see what is wrong with it. Most children will also need a cholangiogram. A cholangiogram is a procedure where dye is injected into the gallbladder to outline the bile ducts from the liver to the intestine. Both procedures (biopsy, cholangiogram) can be done through the skin using needles or through a larger cut in the abdomen. Biliary atresia is an abnormality that may be corrected with a surgery and it is really important to rule this out.
- In children or adults with progressive failure of the liver, a liver transplant may be needed.
- Preoperative preparation:
- For liver biopsy and cholangiogram, the child will need to have an empty stomach in order to undergo anesthesia.
- In children needing a liver transplant, a transplant team will make sure that the appropriate preparations are made for the surgery. Your family will be part of this preparation.
- Postoperative care: After liver biopsy and cholangiogram, the child will be closely monitored for any type of bleeding from the liver biopsy. Feeding may be restarted shortly after the procedure.
- Risks/benefits: The biggest risk of taking a piece of liver for a biopsy is the bleeding. Other risks include infection, injury to organs near the liver or need for repeat biopsy if the specimen was not good enough. The benefit is getting an accurate diagnosis so that treatment can be started right away.
- In some patients, the liver may get so bad that it may not work anymore. When this happens, a liver transplant may be needed. After a liver transplant, the child will be in the intensive care unit (ICU). The transplant team will help with recovery process. The patient will need medicine to keep the body from rejecting the new liver (immune system blockers). Children that undergo a transplant will have to be followed closely for signs of infection, since their immune system will be blocked. They need to be monitored for possibility of rejection.
Home Care (“What do I need to do once my child goes home?”)
- Diet: The baby may need a special formula that may be better for the liver. The baby will likely need vitamins (A, D, E, K).
- Activity: Activity can return to normal when the incisions are well healed.
- Wound care: For biopsy and/or cholangiogram, leave the wound dry for about five days, then the baby can bathe. If the patient underwent liver transplant surgery, the surgical team will let you know when it is safe to given him a bath. Contact your surgeon for any redness or drainage of fluid around the incision or if your child has any fever.
- Medicines: Your child may need medicines to help with itching and to help with allowing the bile to travel from the liver to the intestine more easily. Medicines for pain may be needed including oral narcotics. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for uncontrollable itching, vomiting, abdominal pain, fevers or any problems with the incisions.
- Follow up care: You should follow up with your pediatrician to monitor growth and development. You should also follow up with the gastroenterologist (GI specialist) within a few weeks of going home from the hospital, and you should follow up with your surgeon within a few weeks after the surgery.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Children may develop worsening liver disease and eventually require a liver transplant. Growth and development are often affected, so physical and occupational therapy are helpful. Cardiac and liver disease can affect the lifespan of the child, so follow-up with a pediatric cardiologist and gastroenterologist is extremely important.
References:
- Figure 1 from National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. http://www.niddk.nih.gov/health-information/health-topics/liver-disease/Alagille-Syndrome/Pages/facts.aspx.
Updated: 11/2016
Author: Patricia Lange, MD
Editor: Marjorie J. Arca, MD
Alpha-1 Antitrypsin Deficiency
Condition: Alpha-1 Antitrypsin Deficiency
Overview (“What is it?”)
- Definition: Alpha-1 antitrypsin deficiency (AATD) may cause liver problems in children. It is passed down from parents to the child (inherited). Alpha-1 antitrypsin is a protein made by the liver that goes into the bloodstream to help protect other tissues from damage by certain chemicals. (See Figure 1) In AATD, there is abnormality of the alpha-1 antitrypsin protein, the protein builds up in the liver and causes damage to the liver. The effect of AATD is different in all patients. Only about 1 in 20 babies born with AATD will get liver disease. Sometimes the damage to the liver is bad enough that a liver transplant is needed. Because alpha-1-anti-trypsin protein protects some body parts from harm by certain chemicals, defective protein can result in
damage to organs. - Epidemiology: This condition can affect 1 person in every 3,000 to 5,000 people or about 3.4 million people in the world. White people (Caucasian) are most frequently affected. Boys and girls are affected in equal numbers.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: Newborn babies with AATD may have yellowing of the white of the eyes and the skin (jaundice), swelling of the belly, poor growth, poor appetite. Many babies and children with AATD will have NO symptoms.
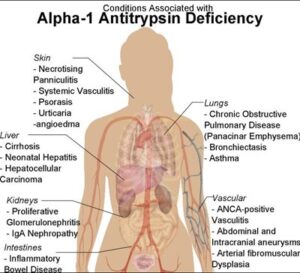
- Later signs/symptoms: Older children and adults may feel tired and weak. Older adults may begin to have difficulty breathing as smoke and chemicals in the environment begin to damage the lungs since they cannot be protected by the abnormal alpha-1 antitrypsin protein. Other body systems that can have problems include skin (itching, hives), liver, kidneys and blood vessels. (See Figure 1)
Figure 1: Possible disease associated with alpha-1 antitrypsin deficiency.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: In a baby or child with jaundice, the doctor will examine the belly to see whether the liver is big or if there is fluid in the belly. Blood tests will check the liver function and to check whether the alpha-1 antitrypsin protein is normal. A genetic test can check the genes that make the alpha-1 antitrypsin protein protein.
- Sometimes the doctor will order an ultrasound test to look at the liver and gallbladder. This test does not cause any pain and uses soundwaves to show a picture of the liver and gallbladder.
- Conditions that mimic this condition: Most babies have some jaundice during the first few days of life. Some babies with jaundice need to be under special lights to make the jaundice go away. Most babies with jaundice do not have AATD. There are other problems that cause jaundice such as biliary atresia, hepatitis, cystic fibrosis, choledochal cyst (cyst of the bile ducts), liver infections and viruses. Your doctor will rule some tests to make sure check for these conditions.
Treatment (“What will be done to make my child better?”)
- Medicine: There is no cure for AATD. The treatment is aimed at making the child’s symptoms better and to limit the damage to the liver. Your doctor might suggest a special diet and avoid medicines that may damage the liver.
- Surgery: The need for surgery in babies and children with AATD is rare. Sometimes children will undergo a liver biopsy to confirm the diagnosis. A biopsy is when a piece of liver is taken and studied to see what is wrong with it. In rare cases, the liver damage could be very serious, and the child will need a liver transplant.
- Risks/Benefits: A person needs his or her liver to work well. If the liver is severely damaged by AATD, then a liver transplant is needed. When a person gets a liver transplant, he or she will need to be on many medicines for the rest of their life to protect against infection and rejection (the body fighting against the new liver).
Home Care (“What do I need to do once my child goes home?”)
- Diet: Good nutrition is very important so the child continues to grow. You may meet with a pediatric dietician to review the best foods to give your child for adequate growth.
- Activity: Unless your child has surgery, there are no limits to activity.
- Medicines: Your child may be given medicines to help with any of the symptoms of AATD, such as medicine for fluid build-up or for itching. Your child will likely need vitamins.
- What to call the doctor for: Call your pediatrician for any bleeding, enlarging abdomen, decreased energy, decreased appetite or severe itching.
- Follow-up care: You will need to see your pediatrician for regular exams and bloodwork. It is important have shots (vaccinations) as directed by the doctor.
Long-Term Outcomes (“Are there future conditions to worry about?”)
People with AATD may develop lung problems later in life and be diagnosed with “emphysema” (chronic damage to the lungs). Children and adults with AATD should NOT smoke or be exposed to smoke and other environmental toxins. Smoke will worsen the damage to the lungs.
References:
Anal Fissure
Condition: Anal Fissure (anal tear, anal skin tags)
Overview (“What is it?”)
- Definition: An anal fissure is a tear or break in the skin at the anus. The anus is the external opening of the rectum, where stool comes out of the body.
- Epidemiology: Fissures occur most commonly in children 6-24 months of age. They are often seen in children who have problems with hard stools and constipation. When hard stools are passed, the lining of the anus can tear, causing pain and bleeding. Anal fissures are the most common cause of rectal bleeding in children.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: Streaks of blood on the stool or on toilet paper, pain/crying with bowel movement, constipation.
- Later signs/symptoms: The tear causes pain during stooling, so a child may hold his poop. Unfortunately, this leads to worsening constipation and when the child finally poops after several days, the tear can get bigger. Skin tags next to a chronic fissure as a result of repeated healing and tearing.
Diagnosis (“What tests are done to find out what my child has?”)
- History of pain with stooling and blood streaks on the stool or toilet paper suggests anal fissure. The fissures are usually located on the middle top or bottom part of the anus.
- Blood tests are not usually needed. A doctor may order X-rays of the abdomen to see if there is a back up of constipated stool.
- Conditions that mimic this condition: Anal fistula, anorectal anomalies, inflammatory bowel disease (Crohn’s disease) in older children.
Treatment (“What will be done to make my child better?”)
- Local wound care: Sitting in tub or basin (sitz baths) with warm water and mild soap cleanses the wound of stool and urine and soothes the muscle around the anus. Sitz baths decrease the pain associated with the tear. This should be done at least 2-3 times a day and after stooling.
- Medicine: Stool softeners and laxatives make the stool easier and less painful to pass. These medicines are important to make healing of the tear faster. Acetaminophen (Tylenol) and/or ibuprofen (Motrin or Advil) may help with pain.
- Diet: To prevent constipation, a diet high in fiber (fruits and vegetables) and with adequate water is recommended to prevent constipation.
- Surgery: Is rarely needed for anal fissures. Sometimes a rectal biopsy is indicated to evaluate for causes of constipation. In older children, endoscopy (colonoscopy) may be necessary to evaluate for inflammatory disorders of the colon.
- Risks/benefits of surgery: If a biopsy of the rectum is needed, it is usually not done when there is a painful fissure. Risks of biopsy include bleeding.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child’s diet should have plenty of fruits and vegetables. Prunes and raisins help soften stools. Apples and bananas can cause constipation, so limit these fruits. Adequate water intake is important.
- Activity: No restrictions in activity.
- Wound care: Sitz baths (soaking in a tub of warm water) 2-3 times a day and after bowel movements. Pat the anal area dry.
- Medicines: Stool softeners, laxatives and fiber additives may be prescribed for your child. Acetaminophen and/or ibuprofen may help with pain.
- What to call the doctor for: Call the doctor or seek medical attention if your child has redness around the anus, drainage of pus, inability to stool, swelling or the belly, vomiting or inability to eat.
- Follow-up care: Your child should be followed regularly by your pediatrician or gastroenterologist (intestine specialist) doctor to make sure the fissure is healing and that the constipation is getting better.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Most infants and children with anal fissures will have no long-term problems. Occasionally, skin tags or growth of tissue will form over the fissure which may cause some discomfort. Usually, once the constipation has resolved, these skin tags will disappear. The most concerning issue in children having anal fissures is chronic constipation that made lead to an endless cycle of pain with bowel movements, repeated trauma to the anus and worsening constipation.
Annular Pancreas
Overview (“What is it?”)
- The pancreas is an organ that sits behind the stomach. It makes chemicals (called enzymes) that help in the digestion of food. It also makes insulin, a chemical (hormone) that controls blood sugar.
- In most people, the pancreas is a flat organ deep in the belly. It is located in between the stomach and the spine just above the belly button. The right edge of the organ sits next to the small intestine, a portion called the “duodenum”. In annular pancreas, the shape of the pancreas is different. A ring of pancreatic tissue surrounds a portion of the duodenum (See Figure 2). This situation can cause narrowing of the duodenum, leading to vomiting, or it can cause no problems at all.
- In annular pancreas, the function of the pancreas is not affected. The pancreas continues to make enzymes for digestion and insulin normally.
- Why does it happen? When a baby is developing inside the mother during pregnancy, the pancreas starts as two parts (called buds). These buds are supposed to come together and fuse to the left of the duodenum. In annular pancreas, the pancreatic buds do not come together normally, and they fuse around the duodenum instead of next to it.
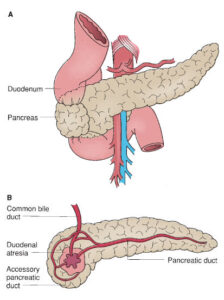 Figure 2
Figure 2
- The exact number of people affected is not clear. Most people with this condition have no problems, so they do not seek medical help. It is estimated to occur in 5-15 people per 100,000 (less than 1 percent).
- Annular pancreas is sometimes seen associated with other defects that are present at birth (congenital) such as Down’s syndrome, problems with the esophagus and duodenum, malrotation and heart defects. In some people, the abnormal shape of the pancreas can lead to narrowing or blockage of the small intestine.
Signs and Symptoms (“What symptoms will my child have?”)
- Approximately one-third of patients with annular pancreas develop symptoms. When symptoms occur depends upon the severity of the intestinal blockage. Those with severe blockage present as a baby with vomiting, inability to tolerate milk or formula. Sometimes the vomited fluid has bile (color green or yellow).
- Later signs/symptoms seen in older children include: belly pain, feeling full early during meals, vomiting, not wanting to eat.
- If a baby or child has bright green or yellow vomit (mixed with bile), he or she should be seen immediately by a doctor. Sometimes vomiting bile can be because of a very serious condition that may be life threatening (volvulus).
Diagnosis (“What tests are done to find out what my child has?”)
- Since most people with annular pancreas have no symptoms, there are usually no abnormalities on blood tests or X-rays.
- In those patients with narrowing or blockage of the duodenum because of the annular pancreas:
- On prenatal ultrasound maternal polyhydramnios may be seen. Maternal polyhydramnios is when excess fluid is present around the fetus. In addition, there may be a “double bubble sign” that suggests narrowing of the duodenum.
- X-rays taken after birth may reveal a “double-bubble sign” or evidence of an intestinal blockage.
 Figure 3. Abdominal X-ray demonstrating a double bubble sign.
Figure 3. Abdominal X-ray demonstrating a double bubble sign.
- Sometimes CT scans (Computerized Tomography—multilevel X-rays of the body) or MRIs (Magnetic Resonance Imaging—radiology study that uses magnetic energy to view the inside of the body) may be done to fully assess the anatomy and confirm the diagnosis prior to surgery.
- Conditions that resemble this condition include intestinal malrotation, duodenal (intestinal) atresia or abnormal position of a vein that goes to the liver (portal vein).
Treatment (“What will be done to make my child better?”)
- Surgery is done only for annular pancreas that leads to narrowing of the intestine.
- The goal of surgery is to make a way for the food to pass from the stomach into the intestine. Usually the part of the intestine before the blockage is sewn to the part of the intestine after the blockage. This allows the food to “bypass” the blockage. Removal of the intestine is almost never needed.
- Depending on the severity of the blockage, age of the child and other factors, the surgery can be done using a bigger incision (open procedure, laparotomy) or several small incisions (laparoscopic, minimally invasive).
- Preoperative preparation
- If your child is dehydrated from vomiting, he or she will be given intravenous (IV) fluids. In some cases, the child has malnutrition from vomiting and inability to tolerate food. The doctor will decide whether the child needs intravenous nutrition or tube feedings prior to the operation.
- If other anomalies are suspected then tests may be done prior to surgery to assess for these conditions. For example, an echocardiogram (heart ultrasound) may be ordered if heart defects are suspected.
- Postoperative care
- Your child will recover in a monitored surgical ward. He or she will not be allowed to eat right away to allow healing of the intestines. They will receive medicines for pain. Possibly intravenous nutrition will be given until feedings are started.
- The length of the hospital stay depends upon the child’s age, postoperative complications and severity of the blockage.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Once the patient starts passing gas and stool and is not vomiting any longer, he or she does not have dietary restrictions and are often allowed to resume a normal diet.
- Activity:
- Infants are under no restriction but may not be able to tolerate tummy time for the first few weeks following surgery.
- In older children, recovery depends on the approach. If the laparoscopy was used, the child can get back to normal in about two weeks. If an open or laparotomy approach is used, it will be 4-6 weeks for the incision to completely heal. During this time, children are encouraged to refrain from physical education, contact sports or strenuous activity. The exact instructions postoperatively will be discussed by your surgeon.
- Wound care: Specific wound care instructions will be given by your doctor prior to discharge. Scars will soften and fade over time but will grow with the child.
- Medicines: Medication for pain such as acetaminophen (Tylenol) or Ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: If the child has a fever greater than 101.5ºF or 38.5ºC that is not relieved by Tylenol; redness or drainage from the incision; or vomiting mandate a call to your doctor or evaluation in the Emergency Department.
- Follow-up care: Follow-up appointments for a wound check and symptoms are scheduled for the first two months. Once a full recovery is noted, then only routine follow-up with the pediatrician is needed.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Long-term results are excellent. Prognosis often depends on other associated abnormalities. Sometimes the duodenum just next tot he narrowing can get very dilated and the muscles may not work properly. If a baby or child with surgical repair of a duodenal narrowing associated with annular pancreas has vomiting that continues for weeks, then a doctor should see the patient.
References:
- Ravitch NM. The pancreas in infants and children. Surgery Clinic North America 1975; 55:377.
- Holcomb. G, and Murphy. P. Ashcraft’s Pediatric Surgery 5th Edition 2010, Elsevier.
- Hays DM, Greaney EM Jr, and Hill JT. Annular pancreas as a cause of acute neonatal duodenal obstruction. Annals of Surgery 1961; 153:103.
- Jimenez JC, Emil S, Podonos Y, Nguyen N. Annular pancreas in children: a recent decade’s experience. Journal of Pediatric Surgery 2004; 39:1654.
- Figure 1: http://pathology.jhu.edu/pc/BasicOverview1.php?area=ba.
- Figure 2: 2009-2014 The Surgical Council on Resident Education Inc; Figure 107.10.
Updated: 11/2016
Authors: Romeo C. Ignacio, Jr., MD, L. Prescher, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Anorectal Malformation
Condition: Anorectal Malformation (imperforate anus)
Overview (“What is it?”)
- Definition: This condition occurs when the rectum of the baby does not come all the way through the tissue of the bottom leaving no opening for the stool to be passed from the body. Depending on the severity of the condition, it is often classified as a low, intermediate of or a high anorectal malformation. It is also known as “imperforate anus”.
- Epidemiology: Anorectal malformations (ARM) occurs in 1 baby in every 5,000 live births. It is equally seen in boys and girls.
 Figure 1: Picture of a baby’s bottom without an anal opening. Picture courtesy of MJArca 11/2016.
Figure 1: Picture of a baby’s bottom without an anal opening. Picture courtesy of MJArca 11/2016.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: After the baby is born, an ARM is diagnosed as no opening for stool to be evacuated from the body or there is an abnormal position of the anus. Sometimes, ARM is noted when a baby does not stool within 24 hours or if a rectal thermometer cannot be inserted. If the anus is abnormally positioned, stool may come out of a different location—seen coming out of the vaginal area, or mixed in the urine.
- Later signs/symptoms: Most of the signs/symptoms occur after an attempt at surgical repair of the condition. One of the most common symptoms is constipation.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: Babies with ARM have higher risk of certain types of other abnormalities. It is important to find out if the baby has these abnormalities so nothing is missed that can impact the baby’s health moving forward. The most common abnormalities are grouped into the “VACTERL” association (named after the first letter of the most common anomalies).
- V (spine): Spine X-ray to look for abnormalities of the bones and ribs. Spine ultrasound or MRI may also be obtained.
- Anus: Baby has high imperforate anus/cloaca
-
- C (heart): An ultrasound of the heart (echocardiogram) is needed to check for problems such as abnormal holes, problems with valves, etc.
- Tracheo-Esophageal fistula (TEF): Abnormal connection between airway (trachea) and esophagus (tube that connects mouth to stomach) and a blind-ending esophagus in neck.
- Renal (kidney): Ultrasound of kidneys to look for abnormalities
- Limbs (arms and legs): Examine arms and legs for deformity. Arms most common place for abnormal bones.
- An abdominal film/X-ray, abdominal ultrasound and pelvic magnetic resonance (MRI) scan are often done to delineate the extent of the imperforate anus
- Conditions that mimic this condition: Babies can have variations in their rectal, genital and urinary anatomy. In girls, the rectum may join with the vagina and urethra to form what is known as “cloaca.”
Treatment (“What will be done to make my child better?”)
- Medicine: Medications are not helpful before surgical repair. Since air and stool in the intestine are not being emptied properly because of the anal problem, the baby’s belly can get swollen. The baby is not fed and occasionally, a tube is passed from the mouth into the stomach to remove air and fluid to keep the abdomen from becoming distended before surgery.
- Surgery: The type of surgery that the baby gets first depends on many factors including the size of the baby and other conditions that s/he may have. The designation of “low” “intermediate” or “high” ARM is given depending on the location of the abnormal opening in relation to the muscle that controls stooling or the sphincter muscle.
- Babies who have a low ARM and who are otherwise healthy may undergo a definitive repair performed soon after birth. In this repair, the end of the anus is matched with the center location of the sphincter muscle. Depending on how complicated the operation is, the baby may need a temporary colostomy to protect the surgical site from stool as the wounds are healing.
- In babies with an intermediate or high imperforate ARM, or if the baby has conditions that would make it unsafe to undergo a definitive repair (such as complex heart condition, very small size), a temporary colostomy (bringing part of the intestine out through the abdominal wall) may be performed to allow for growth which helps increase the success of the procedure. The baby’s stool comes out of this stoma.
 Figure 2. Photo of stoma and mucus fistula (encircled in purple ink). Photo courtesy of MJArca 11/2016.
Figure 2. Photo of stoma and mucus fistula (encircled in purple ink). Photo courtesy of MJArca 11/2016.
-
- Preoperative preparation: Your baby will be kept from eating until the surgery is performed. He/she will be given nutrition through an IV (intravenous catheter) until then.
- Postoperative care: Many times, babies will require a period of anal dilation to decrease the risk of developing a stricture or narrowing where the anal opening is relocated. This can be done at home for a number of months until healing has occurred and the risk of post-operative stricture has decreased.
- Risks/Benefits:
- Risks: Infection or breakdown of the wound, bleeding, damage to surrounding structures may occur during any surgery.
- Benefits: The infant requires a way to evacuate stool effectively, whether relocation of the anal canal in ARM or a colostomy.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Normal
- Activity: Normal
- Wound care: Cleaning the surgical incision after going home is important, as long periods of stool on the skin and incision can lead to wound breakdown in the immediate post-operative period. Use of barrier creams such as zinc oxide are helpful to prevent this skin breakdown.
- Medicines: Often times a medication such as senna or Mira-Lax is given to help develop good bowel habits.
- What to call the doctor for: Any fevers or redness around the incision. Also call your doctor if your child goes more than two days without having a bowel movement or has vomiting, fevers or abdominal pain.
- Follow-up care: You should plan to see your surgeon within two weeks of having the surgery performed and will likely have several visits a year for the first few years of life to make sure your child is able to pass stool without difficulties.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Patients with low ARM have excellent results in terms of continence (able to control bowel movements). They have a very high risk of having constipation for the rest of their lives. Children with intermediate and high ARM have lower success rates, as the severity of the anatomic and neurologic abnormalities are increased in these patients. These children may have more problems with soiling of stool and poor sphincter control. It may take several years to determine the final outcome of the surgical procedure.
- Specialized diets and medications may be needed to help your child have regular bowel movements and to reduce the chance of incontinence or soiling. In intermediate to high ARM, further studies and operations may be required in the future to create the best situation in terms of stool control.
Updated: 11/2016
Author: Michael B. Ishitani, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Biliary Atresia
Condition: Biliary Atresia (BA)
Overview: (“What is it?”)
- Definition: Biliary atresia (BA) is liver disease that occurs in infants only. Bile is a liquid made in the liver and is required to digest food. Once bile is made, it is stored in the gallbladder and is squeezed out by the gallbladder into the small intestine after meals. In biliary atresia, the ducts where the bile flows from the liver to the gallbladder and the gallbladder to the small intestine become inflamed and scar down. This situation results in bile becoming backed up in the liver, causing the liver to get enlarged, inflamed and scarred. If untreated, biliary atresia can cause liver failure and need for transplant.
- Epidemiology: The incidence varies between 1:5,500 for Asians and 1:19,000 for Caucasians. The cause of BA unknown, but most experts believe inflammation and scarring caused by the immune system is to blame for this problem
- It is the most frequent cause of liver-related death in children and the most frequent indication for liver transplant.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: It presents in early newborns with yellow skin (jaundice). The whites of the eyes will turn yellow (icterus). The stools become light grey when normally they should be yellow, green or brown. For the most part, babies have no symptoms. They eat and drink well. It is normal for early newborn babies in the first two weeks after birth to have jaundice, especially if they are breast fed. However, jaundice beyond 14 days is not normal and should be investigated by a doctor.
- Later signs and symptoms: Later signs include worsening of the yellow tint of the skin and eyes. Babies may have a hard time putting on weight. The urine color is dark brown. The belly gets swollen as the liver gets bigger and fluid (ascites) collect in the belly. If left untreated, biliary atresia can lead to failure of the liver, but this takes months to happen. Liver failure is life-threatening. Symptoms of liver failure include development of large blood vessels in the esophagus from back-pressure though the drainage system of the liver. These are called varices and can bleed severely. The child would vomit blood. Large veins can be seen on the skin of the belly. The belly becomes very swollen.
Diagnosis (“What tests will be done to find out what my child has?”)
- Blood studies: Blood will be collected to check the function of the liver. The bilirubin level is related to the degree of back-up of bile through the liver and indirectly the damage to the liver. In general, the worse the jaundice, the worse the bilirubin level. Other blood studies will be done to rule out other conditions that may also cause jaundice and liver damage such as infection or genetic problems.
- Ultrasound: In this test, a probe is applied on the belly directly overlying the liver and gallbladder. The probe uses sound waves to look at the gallbladder, liver and bile ducts. If the gallbladder is small or absent, it is suggestive of BA. The size of the spleen will suggest the degree of back pressure through the liver. Ultrasound may also show other problems that may cause jaundice such as gallstones.
- HIDA scan: This test is done in the nuclear medicine department. A tracer is given to the infant through the vein. Pictures are taken to see if the tracer is excreted through the liver into the bile ducts and followed into the intestine. If there is no excretion, then further investigations for BA are indicated. Often, the baby is given a medicine (phenobarbital) for five days to increase the effectiveness of the HIDA scan.
- While the previous studies can suggest that your baby may have BA, the main studies that will prove it are;
- Liver Biopsy: How the liver looks under the microscope can tell doctors what may be causing jaundice. There are changes that the liver undergoes when a patient has biliary atresia. Since the bile does not flow out of the liver, there are bile plugs that can be seen. Interestingly, the liver develops new bile ducts within it. Unfortunately, these bile ducts do not drain the bile at all. Finally, scarring of the liver can be seen.
- A piece of the liver (biopsy) can be obtained by a radiologist through a hollow needle. Another way of obtaining a liver biopsy is through an incision by a surgeon in the operating room. Your doctors will decide which is the better alternative for your baby.
- Cholangiogram: A cholangiogram is a study where dye is injected into the gallbladder to see the structure of the main bile duct draining the liver. If the bile duct is not present, then the baby has biliary atresia.
- This study can be done by a radiologist under the guidance of an ultrasound or by a surgeon in the operating room.
- Liver Biopsy: How the liver looks under the microscope can tell doctors what may be causing jaundice. There are changes that the liver undergoes when a patient has biliary atresia. Since the bile does not flow out of the liver, there are bile plugs that can be seen. Interestingly, the liver develops new bile ducts within it. Unfortunately, these bile ducts do not drain the bile at all. Finally, scarring of the liver can be seen.
- Conditions that mimic this condition: Doctors will rule out other diseases that cause jaundice such as liver infection or inflammation (hepatitis). Bacteria and viruses can cause liver damage. Another condition that needs to be checked is alpha-1 antitrypsin disorder. It is a genetic disorder that affects liver and lung. Another possibility is Alagille’s syndrome, a condition where there are fewer and normal bile ducts than in the normal person.
Treatment (“What will be done to make my child better?”)
- Medicine: No specific medical therapy is available. Surgery is needed to allow bile to drain from the liver into the small intestine.
- Doctors may change your baby’s formula to something that would be better tolerated by the liver.
- Your baby may need to take special vitamins (D, A, K, E) because these particular ones are not well absorbed when the liver is sick.
- Surgery
- The doctors may give vitamin K for three days before surgery. When there is not enough vitamin K in the body, there is a higher chance of problems with bleeding.
- Antibiotics (medicine to fight infection) will be given through the vein just before the operation to decrease risks of wound infection after surgery.
- The operation: How the surgery is started depends on how sure the surgeons are of the diagnosis of biliary atresia. If the diagnosis of biliary atresia before the surgery is not clear, then a dye is injected into the gallbladder to define the structure the bile ducts (cholangiogram) and a liver biopsy are performed. If no ducts are present, then the surgeon proceeds with the operation to drain the bile from the liver to the small intestine. This procedure is called “Kasai procedure”. It is named for the surgeon who invented the surgery. In this procedure, the surgeon finds an area in the middle of the liver where there are small tubules that may be able to drain bile from the liver. A piece of small intestine is sewn on to this area of the liver for bile drainage.
- At the time of the procedure, if the cholangiogram shows that there is a normal bile duct from the liver to the intestine, a Kasai procedure will not be needed.
- When a cholangiogram is done in the course of this procedure, the gallbladder is usually removed.
- Postoperative care: Where the infant will be cared for after the surgery depends on many factors, including the general health of the baby, amount of blood loss in the operating room, and how long the surgery took. The surgeon and the anesthesiologist will decide whether the baby needs to be in an intensive care unit or the regular ward. Sometimes, a ventilator (breathing machine) may be needed for a day or two to support breathing. The infant will receive antibiotics to prevent infection. Pain medicine will be given through the baby’s IV until he or she is able to start eating again, at which time pain medicines can be given by mouth.
- The baby will be fed once he or she passes stool and gas. The doctors may be interested to know the color of the stool. If the stool is yellow, green or brown, it is an indication that bile is being drained successfully from the liver into the small intestine.
- Risks
- Bleeding: If there is blood loss during surgery and/or if the baby started with a low blood count (anemia), the infant may need a blood transfusion
- Leak or hole in the intestine: During the surgery, the surgeons will sew the intestine to the liver or to another segment of small intestine. If the areas where the intestine are sutured do not heal properly, a hole results allowing leakage of intestinal contents into the belly. This is a serious condition that is signaled by fever, vomiting and belly pain in the first few days after surgery. Operation will be needed.
- Intestinal blockage (obstruction): Whenever anybody undergoes surgery in the abdomen, there is a chance of intestinal blockage. The most common cause is internal scarring that can kink the intestines. Intestinal obstruction can happen at any time, from a few days after surgery to years after the surgery is complete. In some cases, surgery may be needed to release the blockage
- Infection in liver (cholangitis) and /or blood: The infant will have fever, jaundice, light stools and abnormal blood studies. This is treated with antibiotics, usually given through the vein. This can be a life-threatening infection and therefore, immediate medical attention is needed.
- Benefits:
- The Kasai operation is the treatment for biliary atresia. If the surgery is successful, the infant may grow to adulthood and the liver function may remain stable, saving the liver from further damage.
- Sometimes, even after the Kasai operation, the damage to the liver is bad enough that the liver eventually fails and a liver transplant is needed. In these cases, the Kasai procedure allows the child to grow for several years. Obtaining a donor liver for transplant becomes easier because the child is bigger.
- It is important to know that the earlier the diagnosis of BA is made and the sooner the Kasai procedure is performed, then the damage to the liver is not too bad. The results are better is the baby has the surgery within six weeks of birth. If the diagnosis is BA is delayed and the Kasai procedure is done later than three months of life, there is likely damage and scarring to the liver that the baby cannot recover from. These patients will have a higher risk of eventually needing a liver transplant.
Home Care (“What do I need to do once my child goes home?”)
- Diet: The infant may be given a special formula that is better tolerated by the liver.
- Activity: There are no activity limitations.
- Wound care: No special wound care at time of discharge
- Medicines: Clarify with physicians prior to discharge. The most common medicines are:
- Medicine for pain
- Antibiotic to decrease risk of infection of the bile duct and liver
- Vitamins
- What to call the doctor for: Fever, vomiting, any redness or drainage from the surgical wound, worsening jaundice
- Follow-up care: Regular doctor visits are needed to make sure the infant is growing and gaining weight. Bloodwork is done to make sure that Kasai procedure is allowing good bile drainage from the liver and the whether the liver’s function remains satisfactory.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- In general, one-third of infants undergoing Kasai procedure avoid transplant, one-third have liver failure in the first year, and one-third progress to liver failure later in childhood.The long-term survival of BA infants with their native liver, without liver transplant, depends largely on the condition of the liver at the time of the Kasai procedure. A successful surgery restores flow of bile from the liver to the small intestine and lessens further damage to the liver.
- Infants with a shorter duration of jaundice have a better response to the Kasai procedure. This is because the longer the liver does not drain bile, the more injured and scarred it becomes, and the Kasai procedure cannot reverse the damage already done.
- After a Kasai procedure, babies can have an infection of the bile ducts, spreading up into the liver (cholangitis). This presents with fevers, chills, yellow skin, yellow eyes and light colored stools. This is a very serious infection and requires immediate medical attention. If the baby has repeated episodes of cholangitis, it can scar the liver more and may lead to overall worsening of the liver status.
References:
Updated: 11/2016
Author: Joanne E. Baerg, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Biliary Dyskinesia
Condition: Biliary Dyskinesia
Overview (“What is it?”)
- Definition: Biliary dyskinesia is a condition in which the gallbladder does not squeeze well and the bile does not drain out of the gallbladder properly. The term “dyskinesia” is a combination of two terms “dys” which means abnormal and “kinesia” which refers to movement (abnormal movement). The gallbladder is an organ located underneath the liver in the upper right part of the belly just below the ribcage. The liver makes bile and gallbladder normally stores bile. In response to a meal, the gallbladder releases bile released into the small intestine to aid in breaking down (digestion) of foods.
- Epidemiology: Biliary dyskinesia occurs mostly in older children and adults. It has become a common diagnosis in children and in some hospitals is the most common reason for gallbladder removal. It may be related to chronic inflammation of the gallbladder (cholecystitis). Usually, in biliary dyskinesia, there is no stones in the gallbladder.
Signs and Symptoms (“What symptoms will my child have?”)
- Abdominal pain (usually in the region of the right upper belly, by the place where the gallbladder is located) that typically occurs after meals, particularly fatty meals. The pain can be sudden (acute) or can be frequent, and recurrent over a long period of time (chronic). This is called “biliary colic”.
- Nausea, vomiting and not wanting to eat (poor appetite) can also be seen in children with biliary dyskinesia.
Diagnosis (“What tests are done to find out what my child has?”)
- Physical examination usually is unremarkable unless the child is having symptoms. During painful episodes, the patient may complain of right upper abdominal tenderness.
- Ultrasound: Can look for gallstones, which can cause similar symptoms. There are no stones in biliary dyskinesia. In this test, a probe is applied on the belly directly overlying the gallbladder. The probe uses sound waves to get an image of the gallbladder.
- HIDA scan (also known as cholescintigraphy or hepatobiliary scintigraphy) tests how well the gallbladder empties. In this test, a tracer is injected into the blood of the child. This tracer is taken up by the liver and is concentrated in the gallbladder (like bile). After the tracer is given, the patient is given injection of a medicine called cholecystokinin (CCK) or allowed to eat a fatty meal like a hamburger. Both CCK and a fatty meal are signals for the gallbladder to squeeze. This may cause your child pain when the CCK is injected. Normally when the gallbladder squeezes, it dumps out most of the bile. In biliary dyskinesia, the gallbladder may only squeeze out about 35-40% or less of the total gallbladder contents. Incomplete and sluggish emptying causes the gallbladder to be irritated and cause pain. This tracer for this test has a small amount of radioactivity which will NOT be harmful to your child as it is cleared from the body quickly and completely with the poop.
- Blood tests: May be ordered to check your child’s white blood cell count, bilirubin levels, liver function tests and pancreatic enzymes. In most cases, these tests are normal in biliary dyskinesia.
- Conditions that mimic this condition: Cholelithiasis (gallstones), cholecystitis (infection or inflammation of the gallbladder), hepatitis (inflammation of the liver), gastritis (inflammation of the stomach), stomach or duodenal ulcers, and pancreatitis (inflammation of the pancreas).
Treatment (“What will be done to make my child better?”)
- If a child appears to have symptoms of this condition and the ejection fraction on the HIDA scan is low, surgery to remove the gallbladder is recommended.
- Laparoscopic cholecystectomy (removal of the gallbladder) is the standard of care today. The surgery is performed through small incisions in the abdomen using a camera and special tools.
- Risks of surgery: Conversion to open surgery (larger incision in the abdomen), common bile duct injury, bile leaks, bleeding, and infection. Some of these complications can require further surgery. These complication risks are low but should be discussed by your surgeon.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Even after surgical removal of the gallbladder, there is no guarantee that symptoms will resolve. This is because the diagnosis may not be exact, and it may be difficult to tell whether the cause of symptoms is from the gallbladder or is due to another problem such as acid problems in the stomach. It is therefore important to rule out other causes of belly pain before your child undergoes removal of the gallbladder.
References:
- O’Neill: Principles of Pediatric Surgery. ©’2003, Elsevier.
- Holcomb: Ashcraft’s Pediatric Surgery, Sixth Edition. ©o2014, Elsevier Inc.
- Coran: Pediatric Surgery, Seventh Edition © 2012, 2006 by Saunders, an imprint of Elsevier Inc.
- NIH Medline, https://www.nlm.nih.gov/medlineplus/ency/article/000273.htm.
Updated: 11/2016
Authors: Romeo C. Ignacio, Jr., MD; M. Vu, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Branchial Anomalies
Condition: Branchial Anomalies (congenital fistulas, sinuses and cysts of the neck)
Overview (“What is it?”)
- Definition: Branchial anomalies occur when there is a problem in the development of face and neck tissues as a baby is being formed within the womb of the mother.
- Epidemiology: The formation of the delicate face and neck structures is complicated in the developing baby. Skin, muscles, bones and cartilage need to form around holes for the eyes, ears and mouth. If problems happen as the face and neck are forming, several things can result.
- Fistulas are abnormal communications from the inside part of the face and neck onto the skin. The inside opening may be to the ear canal or throat. It usually looks like a hole on the skin of the face and neck where fluid comes out.
- Sinuses are abnormal holes on the skin that end blindly into the skin or muscle.
- Cysts are balls of tissue and tissue that are buried underneath the skin.
- Pieces of cartilage can also be found underneath the skin.
Signs and Symptoms (“What symptoms will my child have?”)
- Fistulas present in several locations including in front of the ear or the front part of the neck. Saliva or mucous may drain from the opening. Openings in front of the ear can connect to the ear canal. Openings through the front of the neck can connect to the throat. Fistulas can be on both sides of the neck.
- Sinuses are also openings in the skin. Since there is no communication to the inside, there is no drainage usually.
- Cysts are bumps that can be felt under the skin. They may be painless or have pain with swallowing. They can get larger with time.
- Fistulas, sinuses and cysts may get infected. Less common symptoms include pain with swallowing or ear pain.
- Rarely, cysts may present as a bump or inflammation of the thyroid with neck tenderness.
Diagnosis (“What tests will be done to find out what my child has?”)
- A correct diagnosis will lead to proper management. Complete history and physical exam is usually all that is necessary for diagnosis. The classic fistula/sinus opening in the usual location, with mucous drainage, is specific for a branchial anomaly.
- Ultrasound confirms the diagnosis and can usually trace if there is an internal opening (fistula).
- CT or MRI may be needed if there is more information needed or if the diagnosis is not definite.
- Depending on how sure the doctors are of the diagnosis, other studies might be ordered.
- Conditions that mimic this condition
- Dermoid cysts: Growth from skin elements
- Thyroid nodules: Growth in the thyroid gland
- Lymph nodes: Small nodules in the neck that enlarge in response to infection.
- Skin infections such as boils or abscesses
Treatment (“What will be done to help my child?”)
- Medicine: No medications are usually needed. If the cyst, sinus or fistula is infected, medicines (antibiotics) are given to control infection.
- Surgery: Removal of the cyst, fistula or sinus is the treatment of choice.
- If the structure is infected, the infection must be treated first with antibiotics. Sometimes, control of the infection needs draining the pus from underneath the skin.
- Abnormalities on the face may connect to the ear canal. Therefore, children with these lesions on the face are usually referred to pediatric ear/nose and throat surgeons.
- Abnormalities of the neck are studied to see the entire structure along with internal openings. The sinus/ fistula or cyst is completely removed. Sometimes, a second small incision made higher in the neck is needed for complete removal. Usually the wound is closed with dissolving sutures, and there are no sutures to remove.
- Preoperative preparation: Patients are usually asked to shower or bathe on the night before surgery. Patients are asked to stop eating or drinking for a few hours before surgery.
- Informed consent: A consent form is a legal document that states the tests, treatments or procedures that your child may need and the doctor or practitioner that will perform them. You give your permission when you sign the consent form.
- Emotional support: Stay with your child for comfort and support as often as possible while he or she is in the hospital. Bring items from home that will comfort your child, such as a favorite blanket or toy.
- Postoperative care: Depending on the extent of the surgery, the patient goes home on the same day of the operation or stays in the hospital overnight.
- Risks/benefits
- Benefits of surgery: Confirm the diagnosis, prevent infection, decrease the risk that the lesion could become malignant.
- Risks of surgery: Bleeding, damage to nerves or neck structures, post-operative scar, risk of anesthesia, rare swelling around the airway that may interfere with breathing. The patient may be observed in hospital overnight if this is a concern.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid strenuous activity first 1-2 days.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Neck swelling or shortness of breath are serious signs that there is bleeding or swelling that is affecting breathing. The patient should go to the emergency room. Fever, redness of the incision or fluid draining from the wound can be signs of post-operative infection.
- Follow-up care: Follow-up visit with the surgeon a few weeks after operation.
Long-Term Outcomes (Are there future conditions to worry about?”)
No long-term concerns if the anomaly is completely excised. There is a small incidence of recurrence, in particular, if there is a history of infection. The recurrence rate is about 3%.
Updated: 11/2016
Author: Joanne E. Baerg, MD; John C. Bleacher, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Breast Problems
Condition: Breast Problems (breast lumps/cysts/masses, breast pain, breast abscess, gynecomastia, premature thelarche, fibroadenoma)
Overview (“What is it?”)
- Definition: There are several breast conditions that can occur in children.
- Breast mass: Abnormal mass or lump in the breast
- Fibroadenomas: Benign (non-cancer) breast lumps most often seen in teenage girls
- Mastalgia: Breast pain
- Premature thelarche: Early breast development in girls six months to nine years of age. This is not typically problematic.
- Gynecomastia: Benign breast enlargement in a male
- Fibrocystic changes: Term used to describe the normal lumpy nature of the developing breast
- Breast abscess: Infection of the breast associated with a pus pocket
- Epidemiology:
- Fibroadenomas typically occur in girls 15-17 years of age. Accounts for about 90% of solid breast masses in girls.
- Gynecomastia may occur in 50-60% of teenage boys.
- Breast abscesses typically occur in infants and in older girls 8-17 years of age. Most often the infection is due to bacteria found on the skin (Staph aureus).
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: The most common sign of a breast problem is a mass or enlargement of the breast. Pain may be present.
- Later signs/symptoms: Enlargement of the mass and increasing pain. In case of an abscess or infection, worsening redness of the skin and fever may be present.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests
- In a child or an adolescent, an ultrasound is the best study. Mammograms are not as helpful in this age group.
- For young girls that have enlargement of breast, some blood tests may be performed to assess for abnormalities in hormone balance.
- Conditions that mimic this condition: Normal breast development in young girls or self-limited breast development in adolescent boys. Breast cancer in young children and adolescents is very rare.
Treatment (“What will be done to make my child better?”)
- Breast lumps: As the breast tissue develops in young girls, the tissue can be lumpy and tender at times. Non-cancerous breast lumps are common in teenagers as their breast develops. The most common lumps are called fibroadenomas and usually do not require treatment.
- Medicine: Pain may be helped by acetaminophen (Tylenol) or ibuprofen (Motrin or Advil).
- Surgery: If lumps that get bigger (greater than 5 cm), cause a lot of pain or anxiety, or those that have worrisome signs of cancer may need to be removed. The bump can usually be removed using a cut around the nipple.
- Preoperative preparation: Your child will have to stop eating several hours before the procedure in order to have an empty stomach for anesthesia.
- Postoperative care: You will likely have to do some simple wound care following any surgical procedure. Your child will be told about any limitations to activities after the surgery.
- Breast pain: Breast pain can be felt as the breast is developing. The tenderness can be felt commonly during the few days before and days during a girl’s menstrual period.
- Medicine: Pain may be helped by acetaminophen (Tylenol) or ibuprofen (Motrin or Advil). Use of supportive bra is helpful. Decreasing caffeine and salt intake may help with the pain. Some people recommend naturopathic treatments such as vitamin E (1,200 IU per day), evening primrose oil (3,000 mg per day), or a combination of both may be helpful in breast pain associated with menstrual period.
- Breast development: Sometimes there is early development of breast tissue in young children. This can happen with one side or both sides. It can happen in girls or boys. Observation and routine follow-up examination may be needed.
- When breasts develop in pre-teen and teenage girls, the breasts are typically firm, lumpy and can be painful especially just before the menstrual period starts. This is normal. It is recommended that decreasing caffeine and salt intake makes the symptoms of breast heaviness and pain better.
- Medicine: Pain may be helped by acetaminophen (Tylenol) or ibuprofen (Motrin or Advil).
- Breast abscess
- Medicine: Breast infections or abscesses will often require antibiotic treatment along with drainage of the abscess.
- Surgery: Abscesses will sometimes require incision and drainage along with antibiotic therapy. This can be done by sucking out the pus through a needle or through a cut, depending on the size and location of the infection as well as the age of the child.
- Gynecomastia: Breast development in boys can occur on one or both sides. It can be seen commonly in obese boys. Sometimes the breast tissue can get smaller. However, if there is significant breast tissue growth, it can cause pain or anxiety and distress.
- Surgery: Removal of the breast tissue can be done usually through a cut around the nipple. Regional removal of fat (liposuction) may be required with simple mastectomy (removal of breast tissue, usually through an incision around the nipple).
- Preoperative preparation: Some bloodwork may be required before your child undergoes surgery, depending on any other medical conditions. Your child will have to stop eating several hours before the procedure in order to have an empty stomach for anesthesia.
- Postoperative care: You will likely have to do some simple wound care following any surgical procedure. Your child will be told about any limitations to activities after the surgery.
- Surgery: Removal of the breast tissue can be done usually through a cut around the nipple. Regional removal of fat (liposuction) may be required with simple mastectomy (removal of breast tissue, usually through an incision around the nipple).
- Risks/Benefits: The risk of a breast cancer in a breast mass in a child is low but regardless, children with breast masses should have regular follow-up examinations. The benefits of surgical excision of breast lumps is often relief of pain, anxiety and worry.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks as the cut is healing.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Any fevers, redness or drainage from the incision site or for increased pain/discomfort.
- Follow-up care: You should follow up with the surgeon and pediatrician for ongoing monitoring of the breast problem.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- The prognosis (expected course of the disease) is very good for children with breast masses. Most breast lumps or enlargement will go away on their own. For non-cancerous lumps that are removed, the likelihood of having the lump come back is low. The likelihood of a breast mass being or becoming cancerous is also low.
- Boys that undergo removal of enlarged breast tissue typically have resolution of their pain and psychological trauma.
Updated: 11/2016
Author: Patricia Lange, MD
Editor: Marjorie J. Arca, MD
Bronchogenic Cysts
Condition: Bronchogenic Cysts
Overview: (“What is it?”)
- Definition: A cyst is a round closed sac or pouch usually present at birth arising from the airways of the lungs. They are usually located close to the windpipe (also known as the trachea) (Figure 1) or major airways branching to the lung (known as the bronchus).
- Development
- Bronchogenic cysts form when small portions the developing trachea and lung pinch off and become separated from the airways.
- Bronchogenic cysts are usually, but not always, outside of the lung. They do not communicate with the normal airways. In addition, bronchogenic cysts do not contain air sacs (alveoli). Alveoli are the main areas of the lung where oxygen and carbon dioxide are exchanged.
Signs and Symptoms (“What symptoms will my child have?”)
- These rare cysts often have no symptoms.
- They may be seen on ultrasound of a developing baby in the uterus or as an unexpected finding on a chest X-ray.
- Bronchogenic cysts located in the area where the main windpipe branches between the right and left airways can sometimes cause pressure on the trachea resulting in breathing problems in newborns.
- Possible symptoms are wheezing, noisy breathing, turning blue in color (cyanosis), breathing problems, chronic cough or chest pain.
- Long-term complications can include coughing blood due to cyst eroding through surrounding tissues (hemoptysis), infection and the development of cancer (very rare).
- These cysts can be found at any age depending on size, location and presence of symptoms.
Diagnosis (“What tests are done to find out what my child has?”)
- They may be detected on chest X-ray, MRI or CT scan of the chest.
- Fifteen percent of bronchogenic cysts are found within the lung (intrapulmonary cysts). They appear as round or oval-shaped, fluid-filled or air-filled cysts. The size can vary widely. Usually they are single in number and approximately two-thirds are in the lower lobes. Cysts may also appear as a combination of air and fluid in the chest that may be suspicious for an infection.
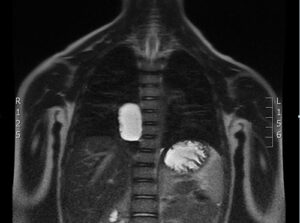 Figure 1 (Image provided by Dr. Marion Henry, Naval Medical Center San Diego, California)
Figure 1 (Image provided by Dr. Marion Henry, Naval Medical Center San Diego, California)
- 85% of bronchogenic cysts are found along the trachea or bronchus In these areas, they also appear as single, round or oval-shaped fluid- or air-filled cysts. Occasionally they can cause compression of the airways.
- A bronchoscope is a fiber-optic camera that is inserted in the airways to identify such cysts that still communicate to the airway. Using a bronchoscope usually requires anesthesia. Those cysts that compress the trachea or bronchus can also be seen on bronchoscopy.
Treatment (“What will be done to make my child better?”)
- Medicine: No medical treatment is able to remove or shrink the cyst. If the cyst is infected, medicines to treat the infection (antibiotics) may be needed.
- Surgery: Symptomatic cysts should be removed with surgery. Most bronchogenic cysts can be removed using open (called thoracotomy) versus minimally invasive (thoracoscopy) techniques. Open surgery means a larger incision between the ribs to remove the cyst. Thoracoscopy means using a camera, telescope and instruments through small incisions to perform the surgery. Thoracoscopy may be contraindicated in children with cysts under the carina. In some cases, it is extremely difficult to separate the wall of the cyst from the normal airway without causing damage to the airway. Near-complete removal and leaving the attached portion of the cyst wall on the airway is reasonable treatment and has not been associated with recurrence.
- Asymptomatic cysts should also be removed because of the risk of infection.
- Risks for surgery are low but include bleeding, infection, collapsed lung, air leakage from the airways and risks of anesthesia.
- Usually, after the surgery a tube to drain air and fluid from the chest cavity is needed for a few days. This tube will be removed prior to discharge.
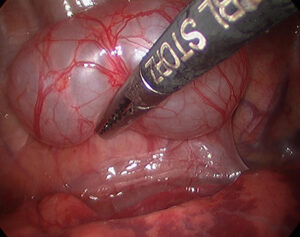 Figure 2 (Image provided by Dr. Marion Henry, Naval Medical Center San Diego, California)
Figure 2 (Image provided by Dr. Marion Henry, Naval Medical Center San Diego, California)
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after thoracoscopic surgery, 4-6 weeks after open surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening pain, fever, breathing problems or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow up with his or her surgeon 2-4 weeks after surgery to ensure proper post-operative healing.
- Complications: Wound infections may need only antibiotics or may require opening up of the wound depending on how bad the infection is.
Long-Term Outcomes (“Are there future conditions to worry about?”)
After surgical treatment, the long-term prognosis is excellent.
Updated: 11/2016
Author: Romeo C. Ignacio, Jr., MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Burns
Condition: Burns
Overview (“What is it?”)
- A burn is damage or injury that can be caused by many things. Most common causes of burn injuries to the skin or flesh include sunlight, scald (due to hot water or steam), contact (direct contact on a hot surface like a stove or iron) and electricity.
- Radiation, electricity and some chemicals can cause burns, too. Severe heat causes damage to the skin.
- How bad and how deep the injury to the skin and the deeper tissues depend on how hot the agent was and how long the time of the contact is between the cause of the burn and the child.
- The depth of burn generally describes how bad the burn is.
- Superficial or first-degree burns have damage only to the outside layer of the skin (epidermis).
- Partial or second-degree burns have injury to the inside layer of the skin (dermis), but not all the way though. In second-degree burns, the remaining dermis can recover with time. The deeper the damage, the longer it takes to heal the skin and more scarring can be seen.
- Full thickness or third-degree burns injure the entire layer of the skin; in this injury, a skin graft is almost always necessary to heal the burned skin. A skin graft is when a portion of healthy skin is taken from another part of the child’s body and placed on the burn site.
- Fourth-degree burns are those that go deeper than the skin, involving the underlying fat, muscle or even bone.
- Inhalation injury is when a child breathes in smoke and heated gases. This can cause severe damage to the lungs and can cause death.
- Certain chemicals can damage the skin and tissue. Chemicals containing strong acids or bases can be present in cleaning fluid. If contact is made with these chemicals, removing the chemical from the skin to prevent more damage is important. If the clothes are contaminated with the chemical, they should be removed. The chemicals should be washed away with running water for at least thirty minutes. All chemical burns should be evaluated by a medical professional.
- Electrical burns can be due to lightning or being in contract with electricity. Electricity gets into the body through one point, travels through the body, and exits from another part of the body in contact with the surface (ground). Patients with electrical burns can sometimes have their heart stop when they get electrocuted. Since the electricity goes through the body, damage to the muscle, bone and internal organs can be present.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs:
- First-degree burns have pink to red tinge to the skin. They tend to be painful at first. A few days later, the burnt skin peels.
- Second-degree burns form blisters. They are painful. The blisters can get big enough and may pop.
- Third-degree burns look grey or white in color. Interestingly, since the skin is completely injured, the nerves of the skin are damaged, too. Therefore, there is no pain in the area of the burn.
- Fourth-degree burns go beyond the skin. They can burn muscle or even bone. Burns due to electric burns can be fourth-degree burns.
- Inhalation injuries can range from difficulty breathing to unconsciousness.
- Later signs/symptoms:
- First-degree burns will heal without significant scarring.
- Second-degree burns will heal slower than first-degree burns, but can have some discoloration. Healed second-degree burns are easily sunburned and will therefore need to be covered by clothing or sunscreen whenever exposed to the sun.
- Third-degree burns that have been grafted can have contraction and scarring of the graft. After skin grafting, the areas may require compression garments to prevent thickening of the scar of the skin graft.
Diagnosis (“What tests are done to find out what my child has?”)
- A child with a burn should be evaluated by a medical professional who has knowledge of how to care for pediatric burns. Medicines for pain are given to help the child’s pain and also so the doctor can see how bad the burn is.
- Inhalation injury is suspected if the child has been trapped in a burning building, has been coughing up soot, or has some singeing of his or her eyebrows, eyelashes or nose hairs. Oxygen will be given to the child to help his breathing. In some cases, a blood test to see the carbon monoxide level is done. Carbon monoxide is a component of smoke. The longer one breathes in smoke, the higher the carbon monoxide level is in the blood. Carbon monoxide prevents the body from taking up oxygen. In severe cases, the child may require being placed in a special chamber where he or she would breathe in pure oxygen (hyperbaric chamber) to reverse the effects of the smoke.
Treatment (“What will be done to make my child better?”)
- Skin covers the entire body and gives a person protection from heat, cold, water loss and infection. The treatment of skin burns depends on how deep and how extensive the damage is. If your child has a burn that is greater than 10% of the entire skin surface, he or she may lose internal fluids and may need to have these fluids replaced intravenously (fluid given into a vein). If there is damage to the lungs because of breathing smoke and hot gases, a breathing tube and a ventilator machine may be necessary during the first days after the injury.
- First-degree burns only affect the topmost layer of the skin. When the red skin peels off, the underlying skin would have regenerated to make new mature skin. This type of burn can be painful, especially if the area affected is large. Cool towels may help the initial pain. Keeping a small child wrapped in lots of wet towels can result in lowering his or her temperature (hypothermia), so one should be careful. For first-degree burns, over-the-counter ointments and/or Tylenol or Motrin are usually the only things needed.
- Second-degree burns cause blisters and sloughing of the skin. These burns can vary in depth. Scald burns from hot liquid are usually less deep than oil burns. In children, sedation or anesthesia may be required for examining and cleaning the burn wounds. There are two ways of treating second-degree or partial thickness burns: 1) putting antibiotic paste such as Neosporin or Silvadene (usually twice daily) or 2) placement of a covering such as Biobrane or Mepilex. These coverings protect the skin as it heals.
- For third- and fourth-degree burns, skin grafts are needed for healing. Skin grafts are harvested from a part of the body that is not injured. Skin grafts are either split thickness or full thickness. Split thickness grafts harvest the epidermis and the topmost part of the dermis, leaving the deep dermis to reconstitute the skin of the harvested site. The harvested skin graft is placed onto the area where the burned skin has been removed. To make skin grafts cover the most area of skin, the harvested skin is sometimes cut to create a net-like effect. With time, skin cells migrate in to cover the entire area of the burn. Full-thickness skin grafts are used in areas that need a lot of movement (such as the hand or over joints) or areas requiring the best cosmetic results such as the face. Skin grafts are either sewn or stapled. Often a bulky dressing is placed over a new skin draft to encourage the graft to stick on to the burn wounds. In 5-7 days, the dressings are removed to inspect the skin graft.
- Children who have been electrocuted or with electrical burns are usually monitored in the intensive care unit. The heart is monitored to make sure that it does not have any abnormal beats or damage. Deep damage to the muscle is monitored by looking at blood levels of a substance released when muscle is injured. If muscle injury is suspected, the patient receives intravenous fluid to wash out the remains of the muscle burn and prevent damage to the kidneys.
Home Care (“What do I need to do once my child goes home?”)
- Diet: When a child has a big burn, it is important to give him food to heal his wounds. In the hospital, his doctors will make sure that he has enough nutrition to heal. At home, it is important to make sure that your child has a healthy appetite and keeps drinking water.
- Activity: What activities your child can have depends on how bad the burn was and what was done to heal it. Sometimes, if there is a fresh skin graft your doctor may want your child to take it easy during the first few days after the skin graft is placed. Your doctor should give you instructions on what your child can do.
- Wound Care: Wound care depends on how deep the wounds were and what was done to have the wounds heal. Your doctor should give you exact instructions on how to care for the wounds. Also ask your child’s doctor if your child can get the wound wet in a shower or a bath.
- Medicines:
- Burn wounds can be painful. Your child may go home with instructions to take over-the-counter medications such as Tylenol or Ibuprofen. Stronger pain medications such as narcotics can be prescribed by your child’s doctor if necessary.
- Some burn wounds are treated at home with antibiotic ointment or cream. Your child’s doctor should give you exact instructions on how to use this.
- If the burn wound gets infected, your child may need to take medicine to treat the infection (antibiotic).
- What to call the doctor for: Skin covers the entire body and gives a person protection from heat, cold, water loss and infection. When skin gets a second-degree burn or worse, infection can settle and enter the body. When your child comes home with a burn wound, he or she should be inspected for signs of possible infection such as fevers, redness around the wound, drainage or pus coming from the wound. If you suspect an infection, you should contact your child’s physician.
- Follow-up care: Your doctor will instruct you on follow up for the burn wounds.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- If the skin has a second-degree burn or worse, the scarring from burns or skin graft can get very thick over time. In some cases, the thickness can limit the motion of the part of the body where the burn was located. Once the burn or the graft is healed, parents are instructed to massage the area with lotion once or twice a day to soften the scar. In some severe cases of scarring, special garments are made to compress the skin. Your child may need to wear the garments for weeks to months to control the thickness of the scar.
- The area of the burn has a high risk of getting sunburned easily. You should instruct your child to cover the burn scars when he or she is exposed to the sun or a high SPF sunscreen (more than 50 SPF) should be used.
- Sometimes, your child’s doctor may prescribe physical therapy or occupational therapy to make sure that the movement of the area that was burned remains normal. Having your child follow up with this therapy is important because you don’t want the area to “freeze”.
Updated: 11/2016
Author: Marjorie J. Arca, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Central Venous Catheters
Condition: Venous Access/Central Venous Catheters (Broviac, Hickman, Portacath, PICC line, Mediport)
Overview (“What is it?”)
- Definition: Catheters or small tubing placed into a large vessel that goes directly to the heart that will allow fluids, medicines or nutrition to reach the bloodstream.
- Often central venous catheters are placed when longer use (weeks or months) of an intravenous catheter will be needed.
- Typically, these catheters are used for chemotherapy, intravenous nutrition, intravenous fluids, intravenous antibiotics and blood draws.
- They may sometimes be placed when a child has very small veins or in children for which it is difficult to place a peripheral intravenous (IV) catheter.
- Types:
- PICC lines (Peripherally Inserted Central venous Catheters) (Figure 1)
- Non-Tunneled Catheters (“Cook”® catheters)
- Broviac®/Hickman® tunneled catheters (Figure 2)
- Portacath/Infusaport (Figure 3)
- Umbilical catheters in newborns
 Figure 1. PICC Line (http://lymelens.com/wp-content/uploads/2013/06/PICC-line.jpg)
Figure 1. PICC Line (http://lymelens.com/wp-content/uploads/2013/06/PICC-line.jpg)

Figure 2. Broviac or Hickman catheter: The entry to the catheter is exposed on the skin.
 Figure 3. Mediport/ Infusaport/Portacath: When not in use, the chamber is completely underneath the skin. When infusion or blood draw is needed, a special needle is used to go through the skin and access the port.
Figure 3. Mediport/ Infusaport/Portacath: When not in use, the chamber is completely underneath the skin. When infusion or blood draw is needed, a special needle is used to go through the skin and access the port.
Diagnosis (“What tests are done before insertion of a central venous catheter?”)
- Blood tests to make sure blood is able to clot appropriately may be obtained
- Sometimes an ultrasound or Duplex study of the blood vessels may be needed to see which ones may be suitable for placement of the catheter, especially if your child has had previous central venous catheters.
Treatment (“How are the catheters inserted?”)
- Surgery
- Preoperative preparation: Your doctor will first decide what type of catheter is needed based on length of treatment and the indication for the central catheter
- PICC lines can often be inserted at the bedside with just a small amount of pain medication injected at the site of insertion.
- Most other central catheters will be placed in the operating room or radiology department with sedation or anesthesia. The blood vessels used for placement may be located either by percutaneous (needle directed through the skin into the vein) or cutdown (incision directly over the vein with isolation of the vein around sutures) techniques.
- Your child will have to have an empty stomach for several hours before the sedation/anesthesia.
- Postoperative care
- Most children do not experience much pain after the procedure but pain medications may be ordered as needed.
- The catheters can usually be used immediately after they are placed.
- A chest X-ray may be obtained after the procedure to confirm correct positioning of the catheter.
- You will be taught how to care for the incision and the catheter before you leave the hospital.
- Preoperative preparation: Your doctor will first decide what type of catheter is needed based on length of treatment and the indication for the central catheter
- Risks/Benefits
- The main risks of central venous catheter insertions are bleeding and infection but in an experienced surgeon’s hands, these risks are very low. Depending on how and where the catheter is placed, other risks include pneumothorax (air in the chest outside of the lung), injury to surrounding arteries and nerves and clotting of the blood vessels near and around the catheter.
- The primary benefits of the catheter are ease of administering fluids and medicines, ease of obtaining blood draws and avoids the need for frequent needle sticks to find a vein for a peripheral IV.
Home Care (“What do I need to do once my child goes home?”)
- Diet: There should be no restrictions on the diet from this procedure.
- Activity: Your child should avoid any direct contact or trauma to the site of the catheter. Once the wounds are healed, your child should be able to bathe normally although with exposed catheters (PICC lines and Broviacs) the skin exit site of the catheter will need to be covered with waterproof tape.
- Wound care: A dry, sterile dressing will need to be placed over exposed catheters, and you should be instructed in how to do this before leaving the hospital and how often to change the dressing.
- Medicines: Your child should not need any additional medicines for the catheter itself but he/she may be started on new medicines that were the indication for the catheter.
- What to call the doctor for: Call your doctor or go to the emergency room for any redness, pus drainage, fluid leakage or increased tenderness around the catheter. You should also notify your doctor immediately for any fevers.
- Follow-up care: Your child will need to follow up with their regular physician who requested the central line placement. You will need to see the surgeon again when it’s time for removal of the catheter. This can sometimes be done in the office for PICC lines and some Broviac/Hickman catheters. For catheters that have been in for several months and for portacaths, your child will need to be sedated or go to the operating room for removal.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Long-term complications of having central venous catheters include primarily infection and clotting of the catheter. These can sometimes be treated with administration of medication through the catheter but sometimes the catheter will have to be removed and replaced with a new one.
- The more catheters your child has to have, the greater the risk of chronic clotting of the blood vessels which may make it more difficult to place additional catheters in the future.
Updated: 11/2016
Author: Patricia Lange, MD
Editor: Marjorie J. Arca, MD
Cecal Volvulus
Condition: Cecal Volvulus
Overview (“What is it?”)
- The cecum is the first section of the large intestine or colon. It is located in the right lower region of the belly.
- Definition: Cecal volvulus is when the cecum twists upon itself. When this happens, the flow of food through the intestine is blocked and blood supply to cecum is kinked. The cecum is a segment of intestine that is normally attached to the lower right side of the belly. Normally these attachments prevent the cecum from twisting on itself. However, there are some conditions where the cecum is at increased risk for twisting on itself. These include the lack of normal attachments that can allow the cecum to move around more than it should, or several underlying medical conditions such as: neurologic impairment, Hirschsprung Disease, intestinal dysmotility or chronic constipation.
Signs and Symptoms (“What symptoms will my child have?”)
The signs and symptoms of cecal volvulus are the result of intestinal blockage and a lack of blood flow to the cecum. Symptoms include belly pain and swelling with vomiting that may be green or bright yellow bile color. As the symptoms progress, the child may feel lethargic, sleepy and tired.
Diagnosis (“What tests are done to determine what my child has?”)
The diagnosis of cecal volvulus is made with abdominal X-rays. The X-rays have characteristics of intestinal blockage, including dilated intestines. Often, a loop of large intestine is seen in the left upper abdomen. If dye is used with the X-rays, the blockage will be confirmed in that area of the intestine just in front of the cecum.
Treatment (“What will be done to make my child better?”)
- Ultimately, the treatment for cecal volvulus is an emergency operation. Some may start with a procedure called colonoscopy where a flexible scope is inserted through the rectum and into the colon. The purpose of this procedure is to attempt to untwist the cecum and decompress the blocked intestines as a temporizing measure. This procedure is only successful in a few (about 15%) of cases. Untwisting using colonoscopy is a temporary treatment because the conditions still exist for the cecum to twist again.
- Most of the time, cecal volvulus requires surgery. Surgery can be done using a moderate sized incision on the belly or using laparoscopy (small cuts in the abdomen that permit the introduction of a scope and small instruments). At surgery, the cecum is untwisted. If the cecum is dead because of lack of blood flow, it is removed. If the cecum is floppy and deemed at high risk of re-twisting, it is removed. The two cut ends of intestine are reattached. Some may fix the cecum to the inside wall of the abdomen with stitches or by placing a tube through the abdominal wall and into the cecum (cecostomy).
- The benefit of these surgery is to keep the intestines from twisting.
- The risks include bleeding, infection and that the volvulus could occur again.
Home Care (“What will I need to do when my child goes home?”)
- Diet: Your child may eat a normal diet after discharge.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after laparoscopic surgery, 4-6 weeks after open surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, diarrhea, problems with urination, or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow-up with his or her surgeon 2-3 weeks after surgery to ensure proper post-operative healing.
Long-Term Outcome (“Are there future conditions to worry about?”)
After recovery from surgery, long term outcome depends upon the underlying reason for the cecal volvulus. Ask your child’s surgeon.
Updated: 11/2016
Author: John C. Bleacher, MD; Joanne E. Baerg, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Choledochal Cyst
Condition: Choledochal Cyst
Overview (“What is it”)
- Definition: A choledochal cyst (CC) is a rare abnormality of the bile ducts. The bile ducts and its branches (hepatic ducts) are structures through which bile travels from the liver to the gallbladder and finally the intestine. Bile is a body fluid made by the liver and stored in the gallbladder. In response to a meal, the gallbladder releases bile released into the small intestine to help in breaking down (digestion) of foods.
- Normally the bile ducts and its branches are skinny channels (a few millimeters in size). Very small bile ducts start in the liver, join together within the liver (like twigs join into branches) and finally right and left hepatic ducts exit the liver and join to become the main hepatic duct. In choledochal cysts, there is enlargement or expansion of parts of the bile duct system. (Figure 1)
- The exact cause (etiology) is unknown. Some experts think that this is something that infants are born with. In 30 to 70% of CCs, there is abnormal anatomy where the bile duct enters the small intestine relative to where the pancreas enters. Experts think that when this happens, juice from the pancreas can go up the bile duct causing the bile duct to get damaged and expand.
- Epidemiology
- Western countries: 1 in 100,000 – 150,000 individuals. Japan: 1 in 13,000 individuals.
- Choledochal cyst is four times more common in females.
- Complications of choledochal cysts can happen
- Cancer can grow in the cyst over time
- Infection of the bile ducts (cholangitis)
- Inflammation of the pancreas (pancreatitis)
- Stones and sludge can form in the cyst and cause abdominal pain or inflammation of the gallbladder (cholecystitis).
- Western countries: 1 in 100,000 – 150,000 individuals. Japan: 1 in 13,000 individuals.
- Pediatric surgeons classify CCs based on what part of the biliary tree is dilated. How the CC is treated is also based on the location of the abnormality. In some cases, the expansion of the bile duct is only localized to the part outside the liver. These cysts are able to be removed completely by surgery. Some types have the abnormality within the small intestine. These cysts may be able to be removed using endoscopy. In some cases, the ducts are abnormal everywhere—inside and outside the liver.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: A choledochal cyst is usually diagnosed in during in infancy or childhood. It can also be diagnosed as an adult. These people may have belly pain, jaundice (yellow tinge to the skin and white of eyes), or swelling in the upper part of the belly.
- Later signs/symptoms: When stones and sludge form in the cyst and/or gallbladder, inflammation of these structures can cause more severe pain or fevers. Rarely, choledochal cysts can rupture resulting in a belly pain and swelling, as well as fevers.
- Infection of the bile ducts (cholangitis) and inflammation of the pancreas can happen.
- Conditions that mimic choledochal cyst: gallstones, sclerosing cholangitis (a progressive scarring liver disease), pancreatic pseudocyst (cyst of the pancreas usually resulting form inflammation or trauma), biliary hamartoma (a growth of the bile duct).
- Caroli’s disease (Type 5 CC): The risk of cancer is less than 7%. Surgery is sometimes needed for infection of the bile ducts or liver complications.
Diagnosis (“What tests are done to find out what my child has?”)
- Ultrasound: Any gallbladder or bile duct abnormality is usually first assessed with ultrasound. Using sound waves, the bile duct and its branches are imaged.
- MRCP: (Magnetic Resonance Cholangiopancreatography). This study is a type of MRI scan where magnets are used to get pictures of the organs in the belly, with detailed images of the bile ducts. It does not require radiation. Small children may need sedation (medicine to make them sleepy) or anesthesia to undergo this scan and remain still. It is painless.
Treatment (“What will be done to make my child better?”)
- The treatment of CC depends on which segment of the bile duct is affected.
- Endoscopy: In some less common types of CC, where the abnormality is localized only to the segment of the bile duct within the small intestine, endoscopy may be used to remove the abnormality. Endoscopy means placing a flexible scope into the mouth of the child and navigating the end of the scope into the small intestine where the bile duct empties. In select cases, this approach can take care of the problem.
- Surgery: In the most common types of CC, where the abnormalities are in the bile ducts outside of the liver, surgery is required. Depending on the situation, the surgery may be done with a large incision (laparotomy, open surgery) or multiple small incisions with a scope (laparoscopy, minimally invasive surgery)
- The abnormal dilated part of the bile duct must be completely removed. Often the gallbladder may need to be removed as well. If the main bile duct is removed, the flow of the bile from the liver to the intestine must be restored. This can be done by creating a connection between the intestines (either the duodenum or jejunum) and the normal bile duct.
- If there are also abnormalities in the bile ducts within the liver, the surgery becomes more complicated and may require removal of parts of the liver. This type of CC can be hard to manage.
- Benefits: Choledochal cysts can cause blockage of the flow of bile and infection of the bile ducts. If CCs are not removed, there is a risk that cancer can grow within the cyst. The risk of cancer increases with age if the CC is not removed.
- Risks: Surgery has low risks, but include:
- Bleeding: The surgeon will check the child’s blood type and have blood available for the operating room.
- Postoperative infection:The child will receive medicine to decrease infection (antibiotics) right before surgery.
- Development of internal scars (adhesions) can cause kinking or blockage of the intestine. This can happen days after surgery or months and even years later
- Risk of anesthesia: The anesthesia specialist will monitor the child carefully throughout the operation.
- All surgery has a risk of damage to internal structures and further operation may be needed to fix a problem.
- Preoperative preparation: The child will have nothing to eat for eight hours prior to operation to decreases the risk of stomach contents spilling over into the lungs (aspiration) as the child goes to sleep. The surgeon will check the child’s blood count and blood type prior to surgery. Blood will be available for transfusion in case of intraoperative bleeding. In most cases, the child can come to the hospital on the morning of surgery and does not need to be admitted prior. Most of the time, a thorough bath or shower is recommended the day prior or the day of the surgery to decrease bacteria in the skin and risk of infection.
- Postoperative Care
- Activity: Typically, the child is encouraged to walk around as soon as possible. To decrease lung complications, breathing exercises such as blowing bubbles, pinwheels or deep breathing is encouraged.
- Diet: Intestines are usually slow after surgery. Most children are not allowed to eat after surgery until there is return of intestinal function as evidenced by passing gas or having stool. Often, a tube is placed through the nose, with the tip in the stomach to suction stomach contents while the intestines are not working yet. This avoids having the child vomit and retch, which is uncomfortable especially with new incision.
- Medicines: Your child may need any of the following:
- Anti-nausea medicine: To control vomiting (throwing up).
- Pain medicine: Pain medicine is required, usually narcotics. These medicines can be given by vein right after surgery when the intestines are not working yet, or by mouth once the guts start working. Acetaminophen and pain medications in the ibuprofen family (Toradol) may be used to supplement pain control.
Home care (“What do I need to do once my child goes home?”)
- Patients with acute appendicitis are usually discharged the same day as their surgery or the following day.
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after laparoscopic surgery, 4-6 weeks after open surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, diarrhea, jaundice, if the wounds are red or draining fluid.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper post-operative healing.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Prognosis is excellent after surgery. Medical studies report excellent survival rates of over 90% and survival without need for further intervention or surgery (event-free survival). Regardless of type, appropriate surgery has good results.
- Although cancer is rare, excision of a choledochal cyst does not completely reduce the risk to zero, so long term follow-up is indicated. The physician may order periodic blood tests or ultrasound studies.
- Unique subtypes: Type 4 choledochal cysts and cysts diagnosed in infancy require more detailed follow-up by a pediatric gastroenterologist, as they have a higher incidence of complications of the liver and complications after surgery.
- Complications:
- Wound infection: Happens <5% of the time. Infections may need only antibiotics or may require opening up of the wound depending on how bad the infection is.
- Small bowel obstruction: 3-5% risk, mostly due to scar tissue or adhesions.
Updated: 11/2016
Author: Joanne E. Baerg, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Cloacal Anomalies
Condition: Cloacal Anomalies (cloaca, high imperforate anus)
Overview (“What is it?”)
- Definition: A cloacal anomaly is a result of abnormal development of the urinary, vagina and anal openings. Instead of three separate openings, there is only one hole where urine and stool comes out. This one opening connects to the urethra/bladder (urine), vagina/uterus and rectum (stool). This problem occurs only in girls. It is the most complex malformation of this area.
- Epidemiology: Occurs in 1 in 20,000 live births (rare).
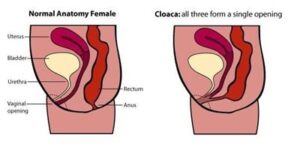 Figure 1:
Figure 1:
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs
- Abnormal appearance of the area where the vagina, urinary opening (urethra) and opening for stool (anus) looks abnormal. There is only one hole instead of three separate holes for these body functions
- Urine and stool coming from same one hole
- May have distended belly
Diagnosis (“What tests will be done to determine what my child has?”)
- Labs and tests: Babies with cloaca have higher risk of certain types of other abnormalities. It is important to find out if the baby has these abnormalities so nothing is missed that can impact the baby’s health moving forward. The most common abnormalities are grouped into the “VACTERL” association (named after the first letter of the most common anomalies).
- Vertebral (spine): Spine X-ray to look for abnormalities of the bones and ribs. Spine ultrasound or MRI may be obtained.
- Anus: Baby has high imperforate anus/cloaca.
- Cardiac (heart): An ultrasound of the heart (echocardiogram) is needed to check for problems such as abnormal holes, problems with valves, etc.
- Tracheo-Esophageal fistula (TEF): Abnormal connection between airway (trachea) and esophagus (tube that connects mouth to stomach) and a blind-ending esophagus in neck.
- Renal (kidney): Ultrasound of kidneys to look for abnormalities
- Limbs (arms and legs): Examine arms and legs for deformity. Arms most common place for abnormal bones.
- Usually need ultrasound or MRI pelvis to look at ovaries, uterus
Treatment (“What will be done to help my child?”)
- No medicine can fix cloaca, only surgery.
- Surgery: The ultimate goal is to separate the urinary tract, stool opening and vagina. These surgeries are done in stages, as they are so complicated that the best results are achieved when the baby is bigger.
- First Surgery
- Goals
- It is important to define the anatomy, as cloacal anomalies are not all the same. This is done by placing a scope in the opening and following where the channels lead—the urinary tract (bladder), the vagina and uterus, and the intestinal tract (rectum)
- Separate urine flow from stool output, since mixing of stool and urine can lead to infections of the bladder and can damage the kidneys.
- If the drainage of the bladder is not adequate, a tube may be placed through the belly to drain the bladder (vesicostomy)
- Often, adequate passage of stool is accomplished by creating a colostomy. A colostomy is when the large intestine is brought out through the belly and stool comes out of the bag. A mucus fistula is another hole where the lower portion of the intestine can drain out.
- Sometimes, the vaginal opening is so narrow that the womb (uterus) is filled with fluid, making the belly big. If so, the womb also needs to be drained of fluid to allow it to normalize in size. If the drainage of the uterus is not adequate, a tube may be placed through the belly to decompress the womb (vaginostomy)
- Postoperative care
- Once stool and gas come out of the stoma, the baby is fed
- Teach parents how to take care of stomas
- Risks
- Anesthesia: Baby will have to be completely asleep with anesthesia and breathing tube for surgery
- Bleeding
- Infection: The baby will receive medicine to prevent antibiotics (medicine to fight infection)
- Possible dislodgment of tubes if these were placed
- Benefits
- Doctor has better idea of anatomy
- The urine flow is separated from the stool, decreasing chances of urinary infection
- Drainage of all three systems is ensured
- Goals
- Second Surgery
- Goals
- Repair of the urinary, vaginal and rectal anomalies
- A separate hole is planned for each system
- Depending on how complicated the abnormalities are, the repair may be done from the bottom only or a combination of bottom and belly approaches.
- Preoperative preparation
- The timing is dependent on many factors: baby must growing and gaining weight, other abnormalities may need to be addressed first (heart, spine, etc)
- Other studies may need to be done prior to the surgery. Your surgeon will decide on this.
- Procedure
- Antibiotics will be given
- A scope will be inserted look at the channels to the bladder, vagina and anus to make sure that there are no changes.
- Create three separate openings
- Make urethral opening (urine)
- Make vaginal opening (may need to use intestine to make vagina if the vagina is not long enough to reach)
- Make opening for stool evacuation (anus)
- May need to also perform laparotomy (incision on belly)
- Postoperative care
- Usually in hospital for pain control, antibiotics, wound monitoring
- Bladder catheter in place usually while in the hospital
- Stool comes out of the colostomy so that stool does not contaminate the new incisions.
- Nothing should be placed into the newly created openings as they are healing for the first 2-3 weeks.
- Return to clinic in 2-3 weeks to start learning dilations of anal opening. Parents will then perform dilations at home to keep the hole from closing up.
- Risks
- Anesthesia: Baby will have to be completely asleep with anesthesia for surgery
- Small risk of bleeding
- Small risk of infection (that is one reason the colostomy stays in place to decrease this risk)
- Risk of damaging vagina or urethra when trying to separate and create the three holes
- Benefits
- Create three distinct holes for the child’s urinary and stool evacuation, and for eventual sexual function
- Goals
- Third surgery
- Goals: Colostomy closure—reconnect the intestine so the baby can poop out of the new anal opening and not have to use a colostomy anymore.
- Preoperative preparation
- The time when the colostomy is closed is dependent on whether the sites for the previous operation are completely healed.
- Before surgery, will need study of the intestine leading to the anus to make sure there are no areas of narrowing and the anal opening empties well.
- Bowel prep day before surgery—usually clear liquids and magnesium citrate or golytely (depends on surgeon)
- Procedure
- Exam under anesthesia to look at anus
- Takedown ostomy: reconnect colostomy and mucus fistula
- Postoperative care
- Antibiotics after surgery
- May wash incision with soap and water
- Continue anal dilations
- Diaper rash cream to buttocks since baby’s bottom has not yet seen stool. The skin is prone to breakdown.
- Risks
- Anesthesia: Baby will have to be completely asleep with anesthesia
- Small risk of bleeding
- Risk of infection: Baby will be on antibiotics after surgery
- Wound infection at incision: Baby will be on antibiotics after surgery. Will closely watch incision for signs of infection. May need dressing changes
- Risk of leak from anastomosis (connection of intestine): Go slow with removing NG/OG tube and advancing feeds
- Benefits: No more stoma. Baby’s intestine now all connected.
- First Surgery
Home Care (“What do I need to do once I take my child home?”)
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid straddling after the first two operations.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, diarrhea, problems with urination, decreased stool output or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper post-operative healing. IT IS IMPORTANT TO KEEP ALL APPOINTMENTS WITH THE SURGEON, AS HEALING IS CRITICAL IN THE FIRST FEW MONTHS AFTER SURGERY.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Bowel obstruction: Baby will have scar tissue in belly from surgeries. Scar tissue can cause kinking or blockage of intestine. If baby has yellow or green throw up, big belly, or does not pass gas/stool from stoma/anus, bring baby to pediatrician or surgeon or ER. Sometimes this can be treated with NG tube and IV fluids and stay in hospital. Sometimes this needs surgery to open up scar tissue and fix obstruction.
- Incontinence (cannot control need to pee and poop): These babies often have problems with potty training both urine and stool. Kids may not be able to feel when they have to pee or poop. They may have to see a specialist (urologist) for problems with urine. For problems with controlling stool, may need to be on bowel management or require other surgeries to try to keep the child clean.
- 20% or fewer of girls with cloacal anomalies have good continence
- Prolapse of anal mucosa (inside lining of the intestines are sticking outside the anus) may occur.
Updated: 11/2016
Author: Grace Mak, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Cloacal Exstrophy
Condition: Cloacal Exstrophy
Overview (“What is it?”)
- Definition: Cloacal exstrophy is an abnormality where the muscles, skin and bones of the lower belly do not form at all. The bones of the pelvis do not meet in the middle as they do normally. The bladder and part of the intestines are exposed to the outside. The exposed bladder is split in two halves and the intestine is in the middle of the two halves of the bladder. In boys, the penis is deformed—small, split in half or even not present. In girls, the clitoris is usually split in two, and the vagina is also usually split in two small channels instead of a single one or may not be present at all.
 Picture courtesy of MJArca 11/2016
Picture courtesy of MJArca 11/2016
- Epidemiology
- 1:200,000-400,000 live births
- Boys more commonly affected than girls
- Other abnormalities are associated with this anomaly include problems with the intestine (shorter than normal, duplicated segments, no anal opening), spine, kidney and genitals. Sometimes, there is a larger defect in the mid-abdomen with a thin covering through which one can see the inside organs. This covered defect is called omphalocele.
- Almost 50% are premature
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: Often, cloacal exstrophy is diagnosed on ultrasound while the baby is still developing inside the mother.
Diagnosis (“What tests are done to determine what my child has?”)
- Cloacal exstrophy is considered part of OEIS association, named after the four commonly seen abnormalities: Omphalocele, Exstrophy, Imperforate Anus (no anal opening), and Spina Bifida
- Omphalocele (opening of muscle and skin in center of abdomen, covered by a sac)
- Exstrophy (see above discussion)
- Imperforate anus
- Spina Bifida (defect in the skin and spine overlying the main nerves of the middle of the back)
- Labs and tests
- ECHO (heart ultrasound) looks for cardiac abnormalities
- Ultrasound of kidneys
- Blood test to determine genetic makeup of the child, check hormone levels of the blood, minerals
Treatment (“What will be done to make my child better?”)
- Cloacal exstrophy requires several operations over months and years. The timing, type of surgery, and result will depend on your child’s situation. Given possible severe deformities of the genitalia (vagina or penis), even gender assignment needs to be discussed thoughtfully and carefully.
- Medicine
- No medicine can fix cloacal exstrophy, only surgery
- Gender assignment
- Chromosome analysis—this determines what exactly is the genetic makeup of the baby
- Multi-disciplinary decision with parents, endocrinologist, psychiatrist, urologist and surgeon
- Surgery (first surgery as newborn): Several surgeons are involved with the baby’s care including general surgeons (intestine and genitals), orthopedic surgeons (bone), urology surgeons (kidney and bladder, genitals), neurosurgeons (brain and spine), cardiac surgeons (heart)
- Preoperative preparation
- Complete examination and studies to look for all possible abnormalities
- Medicine to decrease risk of infection (antibiotics) will be given
- Initial Procedure. Goals of surgery: Separate the intestinal system from the urinary system and close the belly.
- Closure of omphalocele
- Separate bladder from the intestine. The two halves of the bladder are sewed together and placed inside the belly.
- The intestine is brought out through the muscle and skin of the belly as a colostomy so the baby can eliminate stool. A bag will be placed over the colostomy to collect stool.
- Other procedures may be done at the same time. If there is an opening in the spine (spina bifida), closure of the defect may need to be done at the same time.
- Postoperative care
- Once colostomy starts to have stool come out, the baby will be allowed to eat.
- Teach parents how to take care of stomas and may need dressing changes
- Risks
- Anesthesia: Baby will have to be completely asleep with anesthesia and breathing tube for surgery
- Risk of bleeding
- Infection of the wound
- Benefits
- Closure of the abdomen
- Placement of the organs inside the belly
- Separation of urine and stool
- Pelvis procedure. Goals of surgery: Close the ring of the pelvis.
- The pelvis is an open ring in these babies. The hip bones will need to be cut and adjusted. The surgery is called “osteotomies”. The baby will need to be in traction for weeks after surgery. This operation is done usually several weeks or even months after the initial operation. The bladder may need to be repaired during this time as well. It is important to do this operation so that the pelvis can support the baby as the baby grows.
- Pull through procedure. Goals of surgery: Establish stooling out of the bottom.
- This is another separate procedure that may be necessary as your child gets bigger. In this procedure, the colon is brought out into the area of the buttocks so eventually, stool can come out of the region of the buttocks. Sometimes, this is not possible if the muscles of the rectum or the nerves controlling elimination of stool are damaged. The situation is different for individual children. If stooling through the buttock area is a possibility, your child’s surgeon will discuss it with you.
- Multiple reconstructive surgeries for bladder, genital system (penis, vagina/uterus)
- Preoperative preparation
Home Care (“What do I need to do once my child goes home?”)
- Diet: Usually normal for age. In cases where there is a shorter length of intestine, a special formula may be necessary for digestion.
- Activity: Ask doctor before allowing tummy time, but otherwise, activity is normal for age.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery
- What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, problems with urination, decreased stool output or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow-up with his or her surgeon 2-3 weeks after surgery to ensure proper post-operative healing. IT IS IMPORTANT TO KEEP ALL APPOINTMENTS WITH THE SURGEON, AS HEALING IS CRITICAL IN THE FIRST FEW MONTHS AFTER SURGERY.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Bowel obstruction: Baby will have scar tissue in belly from surgeries. Scar tissue can cause kinking or blockage of intestine. If baby has yellow or green throw up, big belly, or does not pass gas/stool from stoma/anus, bring baby to pediatrician or surgeon or ER. Sometimes this can be treated with NG tube and IV fluids and stay in hospital. Sometimes this needs surgery to open up scar tissue and fix obstruction
- Incontinence (cannot control need to pee and poop)
- These babies often have problems with potty training both urine and stool. Kids may not be able to feel when they have to pee or poop. For problems with controlling stool, may usually need to be on medicines for bowel management or require other surgeries to try to keep the child clean.
- Ideally, need several specialists as the baby grows up to achieve the best outcome possible
- Need for multiple surgeries for genital reconstruction
- Gender assignment. This is a complicated issue. Many factors go into the decision of gender for the baby. This will be discussed and resolved carefully with the involvement of all the specialists to have the best possible long-term result for the baby .
Updated: 11/2016
Author: Grace Mak, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Congenital Diaphragmatic Hernia
Condition: Congenital Diaphragmatic Hernia (CDH)
Overview (“What is it?”)
- Definition: Congenital Diaphragmatic Hernia (CDH) is a condition where baby is born with a hole in the diaphragm. The diaphragm is muscle that separates the chest from the belly. Normally, the heart and lungs are in the chest and the intestines and other organs are in the belly. When there is a hole in the diaphragm, organs from the abdomen can go through the defect into the chest cavity. As the baby grows in the womb, his lungs are compressed by these abdominal organs. The lungs are smaller because they lack the space to grow. In addition, the blood vessels of the lung are thicker, making it sometimes difficult for blood to pickup oxygen in the lungs. CDH occurs more commonly on the left. The cause of this defect is not fully known.
- Epidemiology: CDH occurs in about 1 in every 4,000 babies. The size of the hole can vary. Larger defects are associated with more problems because the lungs are usually smaller. Sometimes the lungs are so small that the babies are not able to breathe adequately after they are born, and they die. Most diaphragmatic hernias occur on the left side (80%) and will often contain stomach, spleen, small and large intestine. Those on the right side will often contain portions of the liver.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: Diaphragmatic hernias are mostly discovered during routine prenatal ultrasounds of the mother. An MRI (magnetic resonance imaging radiology test that uses magnetic waves to create images of the inside of the body) of the developing fetus can sometimes be done to predict how big the lungs are and how badly they are being compressed by the intestines and other organs. If a fetus is diagnosed with CDH, his or her birth is planned at a hospital with the capability of caring for babies with this diagnosis. The baby may have severe breathing difficulties, low oxygen levels in the blood and problems with blood pressure. These symptoms can be so serious that they can be life-threatening.
- Later signs/symptoms: Some babies with CDH that do not have symptoms right after birth may later develop problems tolerating their diet or may begin to have difficulty breathing. Some may be discovered after an X-ray is taken for respiratory symptoms such as coughing or wheezing.
Diagnosis (“What tests are done to find out what my child has?”)
- Chest X-ray usually shows intestinal loops in the chest which confirms the diagnosis of CDH.
- Blood will be obtained to check routine labs and to look for oxygen levels in the blood which show how well the lungs are working.
- Echocardiogram (“ECHO”) or ultrasound of the heart will be performed to look for any congenital heart problems and to determine if the heart is being affected by the increased pressure in the lungs from the abnormal growth of lungs. Some babies also have problems with their heart, which may occur in up to 15% of babies with a CDH. This study may also indicate how bad the blood pressure is within the lungs (pulmonary hypertension).
- An ultrasound of the head is usually obtained to make sure that there are no abnormalities or bleeding into/around the brain.
 Figure. 2: Chest Xray showing “bubbles” in the left chest indicating intestine pushing into the chest (small arrows) and heart being pushed over to the right (single large arrow).
Figure. 2: Chest Xray showing “bubbles” in the left chest indicating intestine pushing into the chest (small arrows) and heart being pushed over to the right (single large arrow).
- Conditions that mimic this condition:
- Diaphragm Eventration: An abnormal elevation of one side of the diaphragm. This may be congenital (baby is born with it) causing the diaphragm muscle to be very thin, or it may occur after an injury to the nerve that controls the diaphragm, which then weakens the muscle.
- Foramen of Morgagni Diaphragmatic Hernia: This is a defect in the center and front part of the diaphragm. These types of hernias account for less than 2% of diaphragmatic hernias and typically presents in older children and adults.
- Hiatal Hernia: When the center opening in the diaphragm enlarges, the stomach can then go through the hole into the middle part of the chest. These types of hernias make be associated with symptoms of reflux such as vomiting and heartburn.
Treatment (“What will be done to make my child better?”)
- It is important to know that in babies with CDH, replacing the intestines into the belly and repairing the hole in the diaphragm will not cure the breathing problems. The breathing problems are a result of (1) smaller lung size and (2) pulmonary hypertension.
- Pulmonary hypertension is increased pressure in the arteries of lungs. Under normal circumstances, blood goes through the vessels in the lungs. Blood picks up oxygen and gets rid of carbon dioxide in the lungs. However, if the pressure is high in these vessels, blood is shunted away from the lungs. Exchange of oxygen and carbon dioxide does not happen effectively between the blood and the lungs. Pulmonary hypertension is a life-threatening problem.
- In most cases, the blood pressure within the lungs goes down within several days after delivery. The main issue after birth is to support breathing (bringing oxygen into the body and getting rid of carbon dioxide) without causing permanent and severe damage to the lungs.
- Medical therapy
- The baby is admitted to the neonatal intensive care unit and a breathing tube is placed to help with breathing. A machine (ventilator) is used to regulate breathing, give oxygen and get rid of carbon dioxide. There are several types of machines that deliver increasing and different types of support. Which of these machines are used depend on your baby’s breathing needs.
- A tube is placed through the mouth into the stomach to drain air or fluid. A full stomach can compress the lung and contribute to more problems breath.
- Medicines are usually given intravenously for sedation and pain. These medicines can calm the baby and decrease the pressures within the lung.
- Catheters will be placed in veins (IV) or arteries to deliver medications and also to draw blood to check oxygen levels.
- Surgery
- ECMO (Extra corporeal membrane oxygenation) is a type of heart-lung bypass.
- A procedure to place cannulas (large catheters) into the blood vessels in the neck is performed at the bedside. Oxygen-poor blood is drained from the baby through the cannula in the neck and put through a machine where oxygen is infused into the blood and carbon dioxide is removed. This oxygen-rich blood is returned back into the baby and goes through the organs. Heparin, a medicine that thins the blood, is put into the blood to keep it from clotting.
- Preoperative preparation: Echocardiogram (heart ultrasound) and head ultrasound are usually required prior to ECMO.
- Benefits and risks: ECMO is used when other treatment options fail. ECMO takes on the job of the heart and lungs while pulmonary hypertension resolves. The heart and lungs are able to rest. A baby only can stay on ECMO for a brief time, up to 21 days. If the baby’s lung function does not get better at that time, then prognosis is poor. Risks of ECMO are bleeding, dislodgment of the cannula, clotting of the circuit. Placement of the cannulas can also be risky.
- If the lung function and pulmonary hypertension gets better, the baby is taken off ECMO and placed back on regular ventilator. Repair can be done either on ECMO or after the baby is taken off.
- Congenital diaphragmatic hernia repair: Timing of surgical repair is typically dependent on the baby’s stability and degree of pulmonary hypertension. Sometimes, surgery may be performed while the baby is still on ECMO. The type of surgery will be up to the surgeon and can often be performed through an incision on the abdomen or through the chest. Minimal access approaches (laparoscopy or thoracoscopy) may also be used. For large defects in the diaphragm, a patch may have to be used to close the hole.
- Postoperative care: Following the surgery, the baby will need the same monitoring and support as before the surgery. Often, the baby will need to remain on the ventilator to support the lung function and may need medications to lower lung blood vessel pressure and other medications to raise overall blood pressure.
- Risks/Benefits: The primary risks of surgery include bleeding, infection, injury to the lung, heart or abdominal organs; respiratory failure and death. Survival rates vary from 60-90%. There is also a risk of recurrence of the hernia; recurrence is greater in those that had a patch. placed at the time of surgery. Benefits of the surgery include the replacement of the abdominal organs in the abdomen, allowing the heart and lungs to reclaim the chest.
- Sometimes, if there are a lot of organs that were originally in the chest, replacing them all back in the belly may make the belly too tight. A tight belly would decrease the blood flow to the organs, creating a dangerous situation. In these cases, the abdomen is left open with the organs contained in a silastic silo or closed with a large temporary patch. The belly is then closed in stages.
- ECMO (Extra corporeal membrane oxygenation) is a type of heart-lung bypass.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child will likely be on a typical infant formula or breast milk but may require nutritional supplementation to increase calories and protein. In some cases, if the lungs continue to be weak, feeding by mouth may be too much to coordinate with breathing. The baby may require feeding by tube through the nose or a gastrostomy tube (G tube).
- Activity: Normal activity after the wounds have healed is allowed. Ask the surgeon when “tummy time” is allowed.
- Wound care: Wounds are kept dry for the first three days after surgery, then the wounds may be washed but not soaked for a week. Most of the time, if the baby was born with CDH and repair was performed, he or she should be able to be bathed normally by the time he or she gets home.
- Medicines: The baby may need to continue on some of the medicines for pulmonary hypertension if he/she continues to have difficulty with breathing.
- What to call the doctor for: Call the doctor for fevers, worsening breathing, vomiting, pain or any redness/drainage from the incisions.
- Follow-up care: You will need close follow-up with the pediatric surgeon as well as your pediatrician and possible pediatric pulmonologist.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Survival rates vary from 60-90%.
- Issues with breathing are the most common long term problem and follow-up with lung specialists may be needed.
- Some children may not have the same exercise tolerance as their peers due to the lung abnormalities.
- There is a higher incidence of developmental delay in children with CDH—motor and language problems may be evident. Hearing problems may also be present.
- A high incidence of gastroesophageal reflux is often seen in babies with CDH, some eventually needing surgery to correct.
- The hernia may come back (recur) in up to 50% in babies requiring a patch and 10% in those that did not need a patch. Therefore, regular follow-up is needed.
References
- Coran: Pediatric Surgery 2012.
- O’Neill: Pediatric Surgery, 5th Edition.
Updated: 11/2016
Author: Patricia Lange, MD
Editor: Marjorie J. Arca, MD
Crohn's Disease
Condition: Inflammatory Bowel Disease – Crohn’s Disease
Overview (“What is it?”)
- Definition: Crohn’s disease is an inflammatory condition that can affect any part of the gastrointestinal tract from the mouth all the way to the anus. It typically affects all the layers of the intestinal wall. The most commonly affected area of the intestine is the last part of the small intestine (terminal ileum), but it can affect any part of the intestine and there will often be diseased areas along the intestinal tract with normal segments in between. The intestine can be affected in several ways. Sometimes, the intestine gets so inflamed that a hole (also known as a perforation) can result. This leads to an infection inside the belly (abscess). Sometimes, the intestine can become narrowed or even blocked. Sometimes, parts of the intestine get holes and create abnormal connections from one segment of the intestine to another (intestinal fistula) or the skin around the anus (anal fistula).
- Cause: No one has really defined the real cause of Crohn’s disease. Experts believe that Crohn’s disease is because of many factors—inherited, environmental and dietary.,among others. The end result is that the body‘s immune system attacks the intestine causing the inflammation.
- Epidemiology: Crohn’s disease affects 0.5-9 per 100,000 people, with Caucasians being affected most commonly. A lower incidence is reported in Asia, the Middle East and is seen in the Southern hemisphere. Approximately one-third of people who develop Crohn’s disease are under the age of 20 years.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: The most common initial symptoms of Crohn’s disease include abdominal pain, diarrhea, decrease in appetite and weight loss. The location of the pain depends on which segment of the intestine is affected, so this can be different from one person to another.
- Sometimes Crohn’s disease can first present with perianal disease, including fissures (tears around the anus), abscesses (infections or pockets of pus) or abnormal holes drainage of with pus and stool.
- Other associated symptoms are not related to the intestines at all. This supports the theory that the patient’s immune system is attacking parts of the body without cause. Symptoms may cause include joint pain; tender, red skin nodules (erythema nodosum); red eyes with blurry vision; or inflammation of the liver.
- Children under the age of six are more likely to present with blood in the stool.
- Later signs/symptoms: As the disease progresses, children can have ongoing pain and diarrhea resulting in poor growth, low weight gain and delayed onset of puberty.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests: Often times the diagnosis of Crohn’s disease is suspected based on the symptoms the child is having, the family history and physical exam findings. A full physical exam will include measuring height and weight, looking at the child’s growth curve, a full abdominal exam, rectal exam and assessment of the eyes and skin The surgeon may perform a more thorough rectal exam under anesthesia, especially if the child has complaints of pain, drainage in the anal area or problems with stooling.
- Blood tests will look for evidence of infection, low blood count. However, there is no blood test that is currently available that confirms the diagnosis of Crohn’s disease.
- Imaging can be helpful and may include CT scan, MRI, ultrasound and/or an intestinal contrast study (upper GI with small bowel follow through). What study is done depends on the symptoms of the child. Your doctor will decide which one is best suited for the situation
- Endoscopy is when a flexible telescope is placed in the mouth and is gently pushed through the esophagus, stomach and part of the small intestine. The doctor can look at evidence of inflammation directly, but he will also obtain little pieces of tissue (biopsy) of the esophagus, stomach and first part of the small intestine. These pieces of tissue will also be sent for analysis under the microscope. Endoscopy is also done for the large intestine. The findings of these studies ultimately get to the definite diagnosis of Crohn’s disease.
- Conditions that mimic this condition: infectious enteritis (from bacterial infections), ulcerative colitis (another type of inflammatory bowel disease) or indeterminate colitis and appendicitis (inflammation of the appendix) can all have similar symptoms to Crohn’s disease.
Treatment (“What will be done to make my child better?”)
- Medicine: Most of the time, medications are given primarily to decrease inflammation and decrease the symptoms. These medicines are used to target inflammation that is out of control. The medicines are NOT for Crohn’s disease only. In fact, you may have seen some of these medications used for other diseases that are caused by inflammation.
- Steroids: Steroids can be given by mouth, intravenously or as enemas. Some steroid names are hydrocortisone, budesonide or prednisone, among others. Steroids are very powerful anti-inflammatory drugs, but they are not preferred for long-term management due to side effects with prolonged use.
- Non-steroidal anti-inflammatory drugs: There are other anti-inflammatory medications that are not steroids. Some of these are mesalamine (Asacol, Pentasa), azathioprine (AZA), methotrexate and 6-mercaptopurine (6-MP).
- Biologic agents: Another class of medications are those that decrease inflammation by lowering substances in the blood that cause inflammation. These medicines are usually given as an infusion by vein every few weeks. Infliximab (Remicade) and adalimumab (Humira) are examples of these medicines.
- Diet modification: In some patients, a drastic change in diet is tried to see if this makes Crohn’s disease better. The child stops eating regular food and receives all necessary nutrition through a feeding tube with an liquid elemental formula (where the protein and sugars are broken down into the most basic components).
- Many of these medications are used in combination and at different time points throughout the disease process. The goal is to achieve control of the disease, decrease symptoms and promote intestinal healing
- Surgery: Surgery cannot cure Crohn’s disease. The role of surgery is to take care of complications of Crohn’s disease that cannot be helped with medication. When surgery occurs, the goal is to remove the least amount of intestine length. The usual management is to cut out the intestine that is narrowed or with a hole or abnormal communication and put the two ends back together. Sometimes, if the narrowing is short enough, the affected area can be widened up without removing the bowel. In some cases, especially those where there is infection, severe malnutrition, or high doses of anti-inflammatory medicines, a stoma may need to be formed. A stoma is a surgically created opening on the surface of the belly where a piece of intestine that is brought out to allow flow of stool. A bag is placed over this intestine to control the stool.
- Depending on what needs to be done at surgery, the surgeon may decide whether a laparoscopic or an open (traditional) approach is the best for your child. In a laparoscopic procedure:
- Preoperative preparation: The most important part of preparing for surgery is making sure that the child has appropriate nutrition. The child will need to tolerate surgery and heal. Nutrition is really important to decrease the complications of surgery. The patient may require addition oral (tube feeding) or intravenous nutrition. Your child will be given fluids and antibiotics prior to surgery.
- Postoperative Care
- Activity: Typically, the child is encouraged to walk around as soon as possible.
- Diet: Usually the child is not allowed to eat after surgery because the intestines naturally slow down after an operation. He or she may require a tube through the nose into the stomach to drain it early after surgery. Once the child’s intestines function, as evidenced by passing gas or stool, then a diet will be started.
- Medicines: Your child may need any of the following:
- Antibiotics: To help prevent or treat an infection caused by bacteria.
- Anti-nausea medicine: To control vomiting (throwing up).
- Pain medicine: Pain medicine can include acetaminophen (Tylenol), ibuprofen (Motrin) or narcotics. These medicines can be given by vein or by mouth.
- Risks/Benefits
- Short Term Risks
- Wound infection: Happens less than 5% of the time (unless an infection is already present). Risk is increased if there is already an established infection or if the child is on high doses of anti-inflammatory drugs such as steroids. Infections may need only antibiotics or may require opening up of the wound depending on how bad the infection is.
- Abscesses (pus pockets): If the abscess is small, antibiotics may treat it. If it is big, it may need to be drained.
- Small bowel obstruction: Internal scarring can cause the intestine to kink and become narrowed. The area where the intestines are sewn together can scar.
- Damage to surrounding organs: If the child has had several previous surgeries or the inflammation is severe, there is a risk of injury to surrounding structures including other intestine, the bladder, the fallopian tubes or uterus due to scar tissue that may have formed.
- Long-term risks: Recurrence Is very common in children undergoing bowel resection for Crohn’s. IT IS VERY IMPORTANT TO FOLLOW-UP WITH THEIR GASTROENTEROLOGY SPECIALIST TO RESUME THE MAINTENANCE MEDICATIONS TO KEEP THE INFLAMMATION UNDER CONTROL. All children with Crohn’s disease are also at increased risk of developing a cancer of the colon or the small bowel later in life.
- Benefits: Surgery can resolve a problem that has been difficult to treat with medication; for example: a stricture leading to an obstruction, a fistula resulting in abnormal drainage, infection or pain. Often when symptoms improve and disease has been controlled with surgery, the child will have an improved appetite, gain weight and grow.
- Short Term Risks
- Depending on what needs to be done at surgery, the surgeon may decide whether a laparoscopic or an open (traditional) approach is the best for your child. In a laparoscopic procedure:
Home Care (“What do I need to do once my child goes home?”)
- Diet: After surgery the diet will be slowly advanced back to solids. There are options for dietary supplements that are thought to help with minimizing inflammation including omega-3 fatty acids (fish oils), short-chain fatty acids and other types of fiber. Your doctor may make suggestions as to which supplements are needed.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after laparoscopic surgery, 4-6 weeks after open surgery.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe. If a child has an ostomy there will be teaching on how to care for the stoma prior to discharge from the hospital.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain. Sometimes, if an ileostomy (portion of the small intestines is surgically connected to the abdominal wall) is needed, medicine to slow down the intestine and fiber is needed to decrease fluid loss. MEDICINES TO CONTROL CROHN’S will be resumed by the gastroenterologist.
- What to call the doctor for: Call your doctor for worsening belly pain, fever, vomiting, diarrhea, problems with urination, or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing. Follow up with the gastroenterologist to discuss long-term management and recurrence prevention.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Crohn’s is a life-long disease, and patients will have periods of remission (no symptoms) alternating with flare-ups of symptoms. It is possible that further surgery will be required if complications from the disease develop. It is important to establish long-term follow-up care with the child’s pediatrician and gastroenterologist so that symptoms can be managed effectively and minimized.
References
Articles and graphics adapted from:
- Uptodate, Overview and management of Crohn disease in children and adolescents, http://www.uptodate.com.
- Rufo: Current therapy of inflammatory bowel disease in children. Paediatr Drugs. 2006; 8(5); 279-302.
- New Health Advisor: http://www.newhealthadvisor.com.
- Johns Hopkins: http://www.hopkinsmedicine.org.
Updated: 11/2016
Author: Hannah G. Piper, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Diaphragmatic Eventration
Condition: Diaphragmatic Eventration (eventration of the diaphragm)
Overview (“What is it?”)
- Definition
- The diaphragm is a dome-shaped muscle that separates the chest or thorax (containing the heart and lungs) from the belly or the abdomen (containing liver, stomach, intestines). This large muscle aids during inspiration. (See Figure 1)
- The diaphragm is usually positioned towards the bottom of the ribcage.
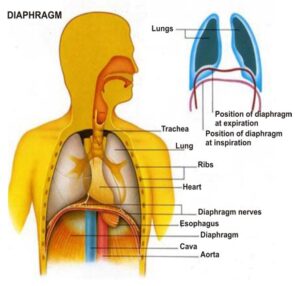 Figure 1.
Figure 1.
- In diaphragmatic eventration, the diaphragm is positioned in an abnormally high position as a result of lack of muscle or nerve function. Sometimes, the nerves or muscles are not well formed or injured. The muscle does not contract which causes its abnormal placement. If the muscle does not contract, it compresses against the lung and may make breathing difficult.
- In general, eventration happens because of two conditions
- Congenital: Situation that is present at birth. It may be due to damage of the nerve that controls the movement of the diaphragm muscle or due to a thin, abnormal diaphragm.
- Acquired: Result of phrenic nerve injury possibly from birth trauma, chest surgery and rare tumors of the chest.
- Asymptomatic congenital diaphragmatic eventrations occur in 7-35 per 100,000 persons.
Signs and Symptoms (“What symptoms will my child have?”)
- Some patients can have no problems. Eventration may be seen in X-rays obtained for other purposes.
- When problems are associated with eventration, they are usually rapid breathing, need for oxygen, inability to eat safely by mouth or poor weight gain.
- Other abnormalities may be present such as nerve injury or compression, chest wall deformities, possible missing ribs, poorly developed lungs, gastric volvulus (twist within the stomach causing vomiting), vascular abnormalities, congenital heart disease, kidney and musculoskeletal defects.
Diagnosis (“What tests will be done to determine what my child has?”)
- Chest X-ray or CT scan of the chest will show an intact diaphragm with elevation of a portion or one side (left or right) of the diaphragm muscle.
- Ultrasound can be used to visualize if the diaphragm moves in the correct direction during breathing. When one inhales, the diaphragm moves downward. However, a paralyzed diaphragm will move in the opposite (upward) direction.
Treatment (“What will be done to make my child better?”)
- Medication: No medication can help eventration.
- Surgery is done when the condition causes problems. Reasons for surgery include
- Two or more pneumonias on the side of the eventration
- One life-threatening pneumonia
- Inability to get off mechanical ventilation
- Respiratory distress related to abnormal motion of the diaphragm
- Operative treatment: Diaphragmatic plication: A procedure which takes the eventration and tightens it with sutures with the goal to flatten the diaphragm muscle. This procedure does not repair the function of the diaphragm. This can be performed with open versus minimal invasive techniques and approached through the chest or abdomen.
- Postoperative Care
- Diet: Patients are started on liquids after their surgery, then advanced to a normal diet depending on how quickly your child is recovering. If the child was on a ventilator before, oral feeding will be delayed until after the breathing tube has been removed.
- Medicines: Your child may need any of the following:
- Anti-nausea medicine: To control vomiting (throwing up).
- Pain medicine: Pain medicine can include acetaminophen (Tylenol), ibuprofen (Motrin), or narcotics. These medicines can be given by vein or by mouth.
Home Care (“What do I need to do once my child goes home?”)
- Patients with are usually discharged within 3-7 days depending on the approach.
- Diet: Your child may eat a normal diet after surgery.
- Activity: Your child should avoid strenuous activity and heavy lifting for the first 1-2 weeks after minimally invasive surgery, 4-6 weeks after open surgery. If the patient is a baby, make sure you check with the surgeon when tummy time can re-start.
- Wound care: Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Call your doctor for worsening belly pain or chest pain, fever, vomiting, problems with breathing, or if the wounds are red or draining fluid.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- After surgical treatment, the long-term prognosis is good.
- For severely symptomatic patients who were on the ventilator before surgery, diaphragmatic plication can help come off mechanical ventilator support.
Updated: 11/2016
Author: Romeo C. Ignacio, Jr., MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Duodenal Atresia
Condition: Duodenal Atresia/Stenosis
Overview (“What is it?”)
- Definition
- The duodenum is the first portion of the intestine that comes right after the stomach. The duodenum is where the bile and pancreatic juice drains.
- Atresia: A medical term used to describe a condition where an opening or passage in the body is closed or absent. Duodenal atresia means that there is a blockage between one part of the duodenum to another. There are several types of blockages. There can be an internal layer causing the blockage or two discontinuous segments. Because of the blockage, the portion of duodenum before the blockage is enlarged (dilated) while the part after the blockage is normal or smaller than normal.
- Stenosis: A medical term that describes a partial narrowing of an opening or passage. In duodenal stenosis, the narrowing causes slowing of flow of food and fluids through the duodenum.
- The duodenum is the first portion of the intestine that comes right after the stomach. The duodenum is where the bile and pancreatic juice drains.
- Epidemiology:
- Duodenal atresia is the most common cause of intrinsic duodenal obstruction in the newborn. It occurs in 1 in 2,500-5,000 live births. In 25-40% of cases, this condition is associated in someone with trisomy 21 (Down syndrome).
- Probably caused by several factors including genetic and developmental factors.
Signs and Symptoms (What symptoms will my child have?”)
- Early signs (Duodenal atresia)
- Often, duodenal atresia is seen on ultrasound performed on a pregnant mother to check on her baby. Because there is blockage of the duodenum, the fluid that the baby swallows has nowhere to go, resulting in enlargement of the stomach and the duodenum
- After delivery, the newborn will often start vomiting within a few hours of birth and not tolerate feeds.
- Most often babies will have bilious (green/yellow) emesis.
- Later signs/symptoms: Symptoms of duodenal stenosis happen later after birth.
- Early on, infants may be able to tolerate some feedings
- As the baby eats more, the food is hung up at the area of narrowing, leading to vomiting, and problems putting on weight.
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests
- Prenatal ultrasound shows dilated stomach and duodenum and too much fluid in the uterus
- Abdominal X-ray—air in dilated stomach and duodenum
- Most of the time, the plain X-ray of the abdomen is enough to make a diagnosis. However, in a patient with a narrowing (instead of complete blockage), other studies may be needed to confirm the diagnosis.
- Upper Gastrointestinal (GI) Study: Contrast is placed in stomach and duodenum to check the anatomy of these structures and the flow of food through the system.
- EGD (Esophagogastroduodenoscopy): A flexible telescope is placed in the mouth and is gently pushed through the esophagus, stomach and part of the small intestine. The doctor can see the inside of the esophagus, stomach and first part of the small intestine to look for obstruction.
- If the baby has Trisomy 21, an echocardiogram is needed prior to surgery because there is an association of heart problems in these patients.
- Conditions that mimic this condition
- Malrotation (abnormal twist of the bowel)
- Duodenal duplication
- Blockage caused by organs compressing the duodenum such as annular pancreas (pancreas is abnormally shaped and encircles the duodenum), preduodenal portal vein (where the main vein entering the liver lies in front of the duodenum).
Treatment (“What will be done to make my child better?”)
- Medicine: There is no medicine to treat the obstruction, only surgery.
- Surgery
- Preoperative preparation
- Placement of tube (orogastric or nasogastric) in stomach to remove the fluid in the obstructed stomach and duodenum.The tube decreases the risk of vomiting and aspiration (vomit fluid gets in the lungs).
- Intravenous antibiotics to decrease infection risk.
- Procedure
- Usually performed once the baby has stabilized from delivery and all the information is known to undertake safe surgery.
- Laparoscopic or open techniques may be used.
- Laparoscopy is an approach where multiple small cuts are made on the belly to insert a telescope and small instruments.
- Open technique is an approach were a larger cut is made on the belly to complete the surgery. It is either done up and down (vertical) or side to side (horizontal).
- Surgeons will make sure that there are no other areas of atresia/stenosis in small and large intestine.
- The surgeon will identify the area of blockage. The intestine before the blocked segment is sewn on to the intestine beyond the blockage, bypassing the obstruction.
- If the dilated segment is really big, then it may need to be narrowed (duodenoplasty) so it can work better
- Preoperative preparation
- Postoperative care
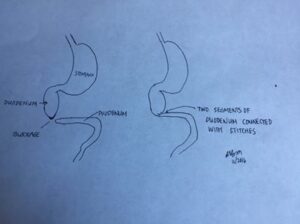
- Continue nasogastric (NG) tube to suction
- The dilated stomach and duodenum usually take days and even weeks to function normally.
- The baby usually needs IV (intravenous) nutrition (TPN) while the stomach and duodenum recover.
- Feeding orally will start when there is only a little fluid that comes from the NG tube. Increasing feeds will be done gradually.
- Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery.
- Risks
- Leak from area where the duodenum is put back together
- Narrowing of the bypass
- Wound infection
- Slow recovery of the stomach and dilated intestine
- Benefits: When the duodenum is put back together, the child is eventually able to eat.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Normal for age
- Activity: Normal for age. Ask surgeon when “tummy time” can resume
- Wound care: Can wash incision with soap and water. May not be able to submerge under water for about a week after surgery. By the time the baby is discharged, it should be fine to resume baths.
- Medicines
- Nothing specific for surgery
- By the time the baby is discharged, pain medication is likely not needed.
- What to call the doctor for
- Redness, warmth, or drainage from incision
- Vomiting
- Fever
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing. Later follow up may be needed if vomiting is a problem.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- The dilated duodenum may have abnormal function and may not move well. May require reoperation with revision of intestinal connection and/or tapering of dilated duodenum
- Reflux: Usually treated medically
- Late bowel obstruction from adhesions (scar tissue). Can be treated medically with NG tube but may need surgery to divide scar tissue
- Survival is over 90%. Deaths are usually related to associated anomalies not duodenal atresia/stenosis.
Updated: 11/2016
Author: Grace Mak, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Duplication Cysts
Condition: Duplication Cysts (intestinal duplication, enteric duplication, alimentary tract duplication)
Overview (“What is it?”)
- Definition: Duplication cysts are abnormal “extra” portions of the intestine that can occur anywhere in the intestinal tract from the esophagus to the rectum. They are called “duplications” because they are attached to the normal intestinal tract and shares its blood supply. These structures can either drain into the normal intestinal tract or not connect at all.
 Picture courtesy of MJArca 11/2016.
Picture courtesy of MJArca 11/2016.
- Epidemiology:
- Children are born with duplication cysts but symptoms usually happen before age two.
- Occurs in about 1 in 4,500 live births.
- Most commonly occurs the small intestine (ileum and jejunum)
- May have multiple duplications in 10-15% of cases.
- May be associated with other anomalies in the following locations
- Spine
- Genitals and urinary tract
Signs and Symptoms (“What symptoms will my child have?”)
- What symptoms the child has depends on the size, location and inside lining of the mass. Cysts lined with stomach tissue can cause bleeding because of the acid produced.
- Other symptoms of this condition include abdominal mass, swelling of the belly, nausea, vomiting, blood in the stool
Diagnosis (What tests will be done to find out what my child has?”)
- If the duplication cyst is located in the chest (esophageal duplication), a chest X-ray may show a mass in the posterior chest.
- Contrast studies (a radiology study where contrast is swallowed and its passage followed through the intestinal tract with several X-rays) can show a mass or cyst that narrows the bowel.
- Ultrasound, CT or MRI scans will show a mass (tubular or spherical shape) that appears to be filled with fluid and attached to the adjacent bowel. However, the findings can sometimes be nonspecific.
- If there is a history of blood in the stool, a technetium scan (radioactive tracer that is given to the child through an IV line) can detect a duplication cyst if the inside lining contains gastric tissue.
- Conditions that mimic this diagnosis: Meckel’s diverticulum, other masses in the abdomen
Treatment (“What will be done to make my child better?”)
- Medicines: No medication can make this situation better.
- Surgery is needed because duplications can cause intestinal blockage, intestinal twisting (volvulus) and bleeding. General anesthesia is required for the operation. The type of surgery and approach depends on the location and size of the duplication.
- If the duplication involves the mouth or throat region, the operation will be performed through the mouth or through a neck incision.
- Duplication cysts of the esophagus will require operation through the chest. Duplications found in the abdomen are removed by approaching the belly.
- Minimally invasive (“thoracoscopy” for chest; “laparoscopy” for abdomen) or open techniques may be used.
- Minimally invasive is an approach where multiple small cuts are made on the belly to insert a telescope and small instruments.
- Open technique is an approach were a larger cut is made on the belly to complete the surgery. It is either done up and down (vertical) or side to side (horizontal). In the chest, the cut is made in between the ribs.
- Minimally invasive (“thoracoscopy” for chest; “laparoscopy” for abdomen) or open techniques may be used.
- Preparation for surgery: Antibiotics (medicine that fights infection) will be given prior to the start of the operation to decrease infection risk.
- Risks for surgery are low but include bleeding, infection, intestinal blockage (from scar tissue of the operation), leakage from the bowel (if a portion of the normal bowel is removed) and risks of anesthesia.
- Benefit from surgery: Removal of the cyst decreases the chances of bleeding, twisting and intestinal obstruction.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Normal for age
- Activity: Normal for age. Ask surgeon when “tummy time” can resume
- Wound care: Can wash incision with soap and water. May not be able to submerge under water for about a week after surgery. By the time the baby is discharged, it should be fine to resume baths.
- Medicines
- Nothing specific for surgery
- Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain. By the time the baby is discharged, pain medication may not be needed. Ask your doctor what the best medicine, if any, is needed for pain
- What to call the doctor for
- Redness, warmth or drainage from incision
- Vomiting
- Fever
- Increasing chest or abdominal pain that is not better after taking pain medications
- Shortness of breath (for operations performed through the chest)
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing. Later follow up may be needed if vomiting is a problem.
Long-term Outcomes (“Are there future conditions to worry about?”)
- Most children with duplication cysts who undergo surgery have no long-term complications. The intestine that is removed is usually short and has no effect on overall growth and nutrition.
- Late bowel obstruction from adhesions (scar tissue). Can be treated medically with NG tube but may need surgery to divide scar tissue
Updated: 11/2016
Author: Romeo C. Ignacio, Jr., MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Empyema
Condition: Empyema (infection of the lung cavity)
Overview (“What is it?”)
- Definition: An empyema is a collection of pus in the chest cavity between the lung and the inner surface of the chest wall.
- Most common cause is pneumonia. Pneumonia is an infection of the lung.
- Other causes: trauma, cancer, injury to esophagus or complication of chest surgery.
- The pus may fill the whole chest cavity or it may be localized collection. The infection is typically caused by certain bacteria that lead to pneumonia (lung infection).
- Epidemiology: Approximately 1 in every 150 children with pneumonia will also develop empyema. Empyema risk is higher in children age 2-4 years of age. Empyemas occur twice as often in the spring and winter than they do in the fall and summer. Boys and girls are affected similarly. Children younger than two years of age have the highest risk of dying.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs: The most common signs and symptoms of empyema in children are fever, decreased appetite, lethargy, cough, chest pain and difficulty breathing.
- Later signs/symptoms: Weight loss may be noted in children with severe pneumonia and empyema because of decreased appetite.
Diagnosis (“What tests are done to find out what my child has?”)
- Physical Exam: Your doctor may notice a decrease in normal lung sounds on the side of the pneumonia and empyema. An increase in rate of breathing may also be noted.
- Labs and tests: Basic blood tests will be performed. Samples of phlegm or sputum to look for a bacterial or viral infection will be performed. A chest X-ray is needed look at the extent of pneumonia in the lungs and fluid surrounding the lung. To get a better view of the empyema, an ultrasound or computed tomography (CT) may be performed as well.
- Conditions that mimic this condition
- Pneumonia without fluid/empyema
- Cystic fibrosis
- Tumors/cancer
- Congenital Pulmonary Cysts/Sequestration
Treatment (“What will be done to make my child better?”)
- Medicine: Medicines that fight infection (antibiotics) are given to treat pneumonia. The type of antibiotic given is the one to which the bacteria causing the infection is most sensitive. Pain medications may be needed because pneumonia and empyema can be painful. Most children need breathing treatments (inhalers) to help open up their air passages.
- Surgery: If the child continues to have fevers, malaise and decreased appetite along with needing more oxygen support, then surgical drainage may be helpful. There are two main procedures for draining the empyema.
- Chest Tube Placement: The tube goes through the skin, in between the ribs and into the chest cavity where the fluid is located. The tube is placed by a surgeon, critical care doctor or interventional radiologist. If the fluid is thin, it will drain out through the tube. If the fluid is thick and semi-solid, medicine to thin out the fluid is given through the tube, allowing the thinner fluid to drain.
- Video-Assisted Thoracoscopic Surgery (VATS): Sometimes, antibiotics and tube drainage are not totally successful in draining the infected fluid. In VATS, small cuts are made on the chest wall through which a telescope and small instruments are inserted, manually removing solidified pus and tissue. This surgery allows the lung to expand fully. A tube will be left in the chest cavity to allow for additional drainage of fluid.
- Thoracotomy: In some situations, the empyema is so severe that VATS cannot treat it. An incision is made in between the ribs along the side of the chest. The infected material is removed through this incision.
- Preoperative preparation: Several hours prior to surgery, your child will have to stop eating so that they can have an empty stomach in preparation for administration of anesthesia.
- Postoperative care: Depending on the status of breathing and need for oxygen, your child may be monitored in the intensive care unit following surgery. He/She will likely have a chest tube to allow for additional drainage of fluid which will be removed a few days after surgery once the drainage has decreased. Antibiotics and pain medications will continue to be given.
- Risks/Benefits of Surgery: The main risks of surgery are bleeding and infection. There is also a risk of injury to the lung. The risks of not performing the surgery include worsening respiratory status, having uncontrolled infection, spreading of the infection into the blood stream and ongoing damage to the lung.
Home Care (“What do I need to do once my child goes home?”)
- Diet: Your child may resume a regular diet.
- Activity: Depending on the incision used for the surgery, your child will likely be able to return to normal activities once the pain resolves and the pneumonia is treated.
- Wound care: The chest tube is usually removed in the hospital before discharge. You may need to use small bandages or band-aids for the chest tube wound(s) until they scab over. Surgical incisions should be kept clean and dry for a few days after surgery. Most of the time, the stitches used in children are absorbable and do not require removal. Your surgeon will give you specific guidance regarding wound care, including when your child can shower or bathe.
- Medicines: Your child may be sent home on some antibiotics for the pneumonia. Medicines for pain such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) or something stronger like a narcotic may be needed to help with pain for a few days after surgery. Stool softeners and laxatives are needed to help regular stooling after surgery, especially if narcotics are still needed for pain.
- What to call the doctor for: Fevers, increased pain, difficulty breathing or any redness/drainage around the incisions.
- Follow-up care: Your child should follow up with his or her surgeon 2-3 weeks after surgery to ensure proper postoperative healing. Follow up with the child’s pediatrician or a lung specialist may also be needed.
Long-Term Outcomes (“Are there future conditions to worry about?”)
- Overall long-term outcome is quite good in children with pneumonia and empyema.
- The chest X-ray findings return to normal in about 3-6 months
- Most children have normal lung function after 6 months to a year and can resume all normal activities.
References
- http://www.uptodate.com/contents/epidemiology-clinical-presentation-and-evaluation-of-parapneumonic-effusion-and-empyema-in-children.
- http://emedicine.medscape.com/article/1001747-overview.
- Coran: Pediatric Surgery.
Updated: 11/2016
Author: Patricia Lange, MD
Editor: Marjorie J. Arca, MD
Epididymitis/Orchitis
Condition: Epididymitis/Orchitis
Overview (“What is it?”)
- Epididymitis is inflammation of the epididymis. The epididymis is a long coiled tube that connects the testicles to the urethra in the penis. Its function is to store and transport sperm from the testicle to the penis. It is located on the top and back (posterior) portions of the testicle.
- Epididymitis is usually caused by an infection, either bacterial or viral. The most common cause of bacterial epididymitis in sexually active males is gonorrhea and chlamydia. Sometimes the inflammation can be caused by an abnormal response of the immune system (autoimmune).
- Viruses that can cause this problem include mumps, coxsackie, echovirus and adenovirus.
- Autoimmune disorders (a condition that affects the normal immune system that recognizes cells from foreign versus self tissue) such as Henoch-Scönlein purpura or Kawaski disease can also cause epididymitis.
- In males who are not sexually active, epididymitis can be caused by urinary tract infections (bladder infections) or underlying urinary tract abnormalities.
- Examples of urinary tract abnormalities include blockage of the tube where urine travels (such as posterior urethral valves) or when the bladder does not empty completely.
- Very rarely, a blood stream infection (sepsis) can become so bad that the infection spreads to the epididymis.
- Epididymitis can occur after undergoing urologic procedures or instrumentation.
- Orchitis is inflammation of the testicle. It usually occurs as an extension of epididymitis, though sometimes it occurs by itself. Mumps is a common cause of orchitis in boys who have gone through puberty.
Signs and Symptoms (“What symptoms will my child have?”)
- The most common symptom is scrotal pain. The pain usually develops over the course of a few days, increasing in intensity. In epididymitis, the pain is located on the backside of the scrotum. In orchitis, the entire testicle is painful.
- Other symptoms include swelling and redness of the scrotum. This usually only occurs on one side, but may occur on both depending on the extent of the inflammation.
- Sometimes boys experience symptoms similar to a urinary tract infection such as burning with urination, feeling like one has to urinate all the time
- Less common symptoms are fevers or vomiting, though they can occur with both epididymitis or orchitis.
Diagnosis (“What tests are done to find out what my child has?”)
- Epididymitis and orchitis can usually be diagnosed with a thorough history and physical exam.
- Your child’s physician may also order a urine test to see if there is an infection in the urinary tract.
- An ultrasound may also be performed in order to rule out other serious diseases such as testicular torsion (when the testicle twists around its blood supply) and confirm the diagnosis of epididymitis and/or orchitis.
Treatment (“What will be done to make my child better?”)
- The treatment for epididymitis and orchitis is mostly supportive.
- If there is concern for infection, antibiotics will be provided by your child’s physician.
- Pain is usually managed with over-the-counter medications such as acetaminophen (Tylenol) and ibuprofen (Advil/Motrin).
Home Care (“What do I need to do once my child goes home?”)
- Bedrest and scrotal elevation are effective at reducing pain. Scrotal elevation can be accomplished using folded sheets or a small pillow.
- Over-the-counter pain medication such as acetaminophen (Tylenol) or ibuprofen (Motrin or Advil) can be used to treat symptoms.
Long-Term Outcome (“Are there future conditions to worry about?”)
- Most cases of epididymitis resolve over the course of a few days with no lasting effects.
- If there is an anatomical issue such as an obstruction, chronic or recurrent epididymitis may develop. Your child may need surgery to correct the anatomical abnormality.
- In rare cases, orchitis can decrease the amount and quality of sperm, resulting in infertility. Most research has demonstrated that this is temporary and improves with time.
References
- Gatti J, Pettiford J. The Acute Scrotum. In: Holcomb G, Murphy P, Ostlie D, eds. Ashcraft’s Pediatric Surgery. 6th ed. Philadelphia: Saunders; 2014:702-706.
- Lewis A, Bukowski T, Jarvis P, et al. Evaulation of Acute Scrotum in the Emergency Room. Journal of Pediatric Surgery 1995;30:277-282.
- Macdonald N, Bowie W. Epididymitis, Orchitis, and Prostatitis. In: Long S, Pickering L, Prober C, eds. Principles and Practice of Pediatric Infectious Diseases. 4th ed. Philadelphia: Saunders; 2012: 367-369.
- Netter F. Atlas of Human Anatomy. 6th ed. Philadelphia: Saunders;2014.
- Santillanes G, Gausche-Hill M, Lewis R. Are Antibiotics Necessary for Pediatric Epididymitis? Pediatric Emergency Care 2011;27:174-178.
Updated: 11/2016
Authors: D. Neubauer, MD; Romeo C. Ignacio, Jr., MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Esophageal Atresia and Tracheo-Esophageal Fistula (EA and TEF)
Condition: Esophageal Atresia and Tracheo-Esophageal Fistula (EA and TEF)
Overview (“What is it?”)
- The esophagus is the muscular tube that allows food and liquid to pass from the mouth to the stomach. . In esophageal atresia (EA), the esophagus does not form normally; instead, the upper part ends blindly in the lower neck or upper chest and is therefore blocked. There are different types of EA that may be associated with a tracheo-esophageal fistula (TEF)
- Most of the time, EA is associated with a TEF, a condition where the lower part of the esophagus has an abnormal connection (fistula) to the trachea or windpipe, allowing stomach acid to enter the lungs.Other, less common forms include EA without a TEF (also known as “isolated esophageal atresia”) or “long gap esophageal atresia” or a TEF without an EA (also known as “H type fistula”).
- Epidemiology: The condition is rare, occurring in roughly one infant for every 4,000 births in the USA. More than half of infants born with EA/TEF will also have abnormalities of one or more of the following body systems: vertebral, anorectal, cardiovascular, renal (kidney) and limbs (VACTERL association, see below). For parents who have a child with EA/TEF, a subsequent child will have a higher risk than the general population of having EA/TEF. Having a parent with EA/TEF increases the likelihood of the offspring having EA/TEF.
Signs and Symptoms (“What symptoms will my child have?”)
While developing in the uterus, an infant with EA/TEF may have too much amniotic fluid (polyhydramnios) surrounding it. After the birth, the first clues are often excess saliva at the mouth (not able to handle saliva) and choking and coughing with attempts to feed.
Diagnosis (“What tests are done to find out what my child has?”)
- If EA/TEF is suspected, an attempt is made to place a tube from the nose or mouth to the stomach. If there is resistance to passage of the tube, it may mean that there is a blockage in the esophagus. Chest X-rays shows the tube coiled in the esophagus.
- It is important to find out if the baby has abnormalities commonly found in patients with TEF/EA, so nothing is missed that can impact the baby’s health moving forward. The most common abnormalities are grouped into the “VACTERL” association (named after the first letter of the most common anomalies).
- Vertebral (spine): spine X-ray to look for abnormalities of the bones and ribs. Spine ultrasound or MRI may be obtained
- Anus: Baby has high imperforate anus/cloaca
- Cardiac (heart): An ultrasound of the heart (echocardiogram) is needed to check for problems such as abnormal holes, problems with valves, etc.
- Tracheo-Esophageal fistula (TEF): Abnormal connection between airway (trachea) and esophagus (tube that connects mouth to stomach) and a blind-ending esophagus in neck.
- Renal (kidney): Ultrasound of kidneys to look for abnormalities
- Limbs (arms and legs): Examine arms and legs for deformity. Arms most common place for abnormal bones.
- Anus: Baby has high imperforate anus/cloaca
- Usually need ultrasound or MRI of the spine to look at the location of the spinal cord
- Cardiac echocardiogram: Will show whether the aorta (largest blood vessel from the heart) lies on the right or left side of the chest. Usually, the surgery is done on the side opposite to where the aorta is located.
Treatment (“What will be done to make my child better?”)
- Medicine: No medicines can make this situation better.
- Surgery: Surgery is the only option for this condition. The goal of surgery is to cut the abnormal connection (fistula) between the lower part of the esophagus and the trachea, close the hole in the trachea, and connect the upper and lower ends of the esophagus so that food can pass from the mouth to the stomach.
- The operation is done through a large incision between the ribs of the chest (thoracotomy), or thoracoscopy where a few small cuts are made in the chest. Through one of the cuts, a video camera is placed. The surgery itself is done using small instruments placed through the other incisions. The usual number of incisions (cuts) for laparoscopic surgery vary. Since the aorta is more commonly on the left side, the surgery is usually done on the right chest.
- When the two ends of the esophagus are too far to bring together in a single setting, a variety of techniques may be employed to accomplish the connection in a staged fashion and at a time when the baby is bigger. When these staged repairs are needed, a feeding tube is placed into the stomach (gastrostomy or G tube) to allow the infant to be fed directly into the stomach before the esophagus is reconnected. Rarely, attempts to connect the ends of the esophagus are abandoned and the esophagus is “replaced” by using a segment of large intestine, or the stomach is pulled up into the chest to be connected to the upper end of the esophagus. In these extreme cases, life-long difficulties with normal eating should be expected.
- In the rare cases where the esophagus is not blocked but has a connection to the trachea (“H-type” TEF), the operation is usually approached through the right side of the neck to divide the abnormal connection between the trachea and the esophagus.
- Preoperative preparation: Studies to check the heart and kidneys are performed to make sure that the baby is ready for anesthesia and surgery. Antibiotics are given prior to starting the surgery to prevent infection.
- Postoperative care: The child may need support for breathing with a breathing tube and a ventilator. S/he may have a drain (chest tube) to drain air and fluid that collect after surgery. Antibiotics may be given for a few days after surgery. A few days after surgery, the baby will undergo a swallow study, to check that the connection between the upper and lower parts of the esophagus is healed and is not leaking.
- Benefits of surgery: Surgery will establish the continuity of the esophagus, allowing the food that the baby eats by mouth go through the esophagus into the stomach. Additionally, abnormal connections between esophagus and the windpipe are cut off, protecting the airway from stomach contents and/or swallowed food.
- Risks of surgery: After the esophagus is reconnected, several later complications may occur. These include leakage at the connection or narrowing (stricture) due to scar tissue. Leakage usually will close on its own when given extra time.
Home Care (“What do I need to do once my child goes home?”)
- After an infant is discharged home, the parents need to be aware of the symptoms that occur when certain situations happen that are common in TEF/EA patients.
- Narrowing at the area where the upper esophagus is sewn to the lower esophagus happens quite a bit. The baby may have problems swallowing, coughing and sputtering as the milk or formula gets caught up in the narrowed point (structure). A few weeks after surgery, it will be stretched out to allow for easier passage of food.
- Frequently, reflux of stomach acid into the esophagus (GERD) occurs. GERD may need to be treated with medication, or in severe cases, with surgery to prevent the acid from doing damage to the esophagus or lungs.
- When a child is born with EA/TEF, the esophagus will not have the normal ability to propel food into the stomach (poor motility) making certain foods difficult to eat. This problem may become more obvious when the baby starts eating solids.
- Also, the trachea may be floppy and collapse on itself with vigorous crying (tracheomalacia). This can inhibit air from moving in and out of the lungs. In severe cases of tracheomalacia, an operation may need to be done to keep the trachea from collapsing on itself.
- In addition, the connection between the trachea and the esophagus can reopen over time (recurrent TEF) and require another operation to disconnect them again.
Updated: 11/2016
Author: John C. Bleacher, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
Esophageal Foreign Bodies, Injury and Trauma
Condition: Esophageal Foreign Bodies, Injury and Trauma
Overview (“What is it?”)
- Esophageal problems can happen when children swallow small objects that can be stuck in the esophagus. These include coins, pins or toys. Sometimes, a disc battery can be swallowed. Disc batteries are VERY DANGEROUS!!! They release acid and have electricity and can cause a hole in the esophagus in a very short period of time.
- Esophageal problems can also be called by swallowing of household chemicals that cause burn damage to the esophagus. The most commonly swallowed products include cleaning products with bleach, dishwater soap, laundry detergents, oven cleaners, toilet bowl cleaners and swimming pool products. Cosmetic products such as hair relaxer can also cause esophageal burns. The severity of injury varies with the concentration and the length of time the agent remains in contact with the mucosa. Severe exposure can lead to chronic narrowing of the esophagus or even a hole in the esophagus.
- In adolescents who have meat stuck in their esophagus, the diagnosis of eosinophilic esophagitis should be ruled out.
- Epidemiology: In 2014, 2.1 million caustic ingestions occurred in the US. 48% occurred in children younger than five years of age. In the younger age group, most swallowing incidents are accidental. The most commonly swallowed products in children five years or younger are personal care products, household cleaners, pain medications and toys. In the adolescent age group, these incidents may be part of a suicide attempt.
Signs and Symptoms (“What symptoms will my child have?”)
- Early signs:
- If the event of swallowing an object or chemical is witnessed, then intervention for removal and evaluation of possible damage to the esophagus can happen quickly.
- Objects stuck in the esophagus may block the esophagus. The child may not be able to swallow food, water or even saliva. There may neck or chest pain on swallowing. The child may make gagging, choking or coughing sounds. There may be discomfort in the neck or chest.
- Ingestion (swallowing) of dangerous products can cause damage to the esophagus. Because these products cause burns of the skin, tongue and mouth, burns can be seen in these areas. In addition, the substances can also damage the breathing organs such as the windpipe and lungs. The child may make gagging, choking and coughing sounds. Wheezing may also be present.
- Severe vomiting or retching can present with chest pain or blood in the vomit depending on the extent and depth of injury.
- Later signs/symptoms:
- Foreign body
- May present later as chest pain or fever
- Blood in the saliva or phlegm
- Ingestion of dangerous substances may have swelling of the lips and mouth. The child may develop problems swallowing if the esophagus scars.
- If there is a hole in the esophagus, the child can be very sick with a severe life-threatening infection. This will be with very high fevers and chills.
- Foreign body
Diagnosis (“What tests are done to find out what my child has?”)
- Labs and tests:

- Chest x-ray is usually the first test done. If there is a coin or other material stuck in the esophagus, it may show the location. In addition, if there is fluid in the right or left chest cavity, there may be a hole in the esophagus which is a surgical emergency. X-ray below shows a coin stuck in the esophagus.
- An esophagram is a test where the patient is made to drink barium, and X-rays are taken during the swallowing process. This may show where something is stuck or whether there is a hole in the esophagus.
- If the child had fevers or has been vomiting for a while, bloodwork may be needed.
- Conditions that mimic this condition:
- Gastroesophageal reflux/Esophagitis—when food and acid in the stomach backwash into the esophagus and cause heartburn and inflammation to the esophagus
- Esophageal webs or duplication cyst—abnormalities of the esophagus that a child has been born with. These can cause partial blockage
- Pneumonia—infection of the lug
- Eosinophilic esophagitis—inflammation of the esophagus because of allergies
Treatment (“What will be done to make my child better?”)
- Medicine
- Medicine to treat the pain may be given
- Antibiotics may be given if there is concern for a tear in the esophagus
- If there is wheezing, the child may need inhalers.
- MEDICINES TO MAKE THE CHILD VOMIT (IPECAC) ARE NOT RECOMMENDED IN THIS SITUATION.
- Non-surgical procedures for coin removal: If a coin is stuck in the esophagus for less than 24 hours, there are a couple of alternatives that can be tried in the emergency department. One option is where the doctor will pass a tube with a balloon on the end of it down past the object, inflate the balloon, and then pull the object back into the mouth. Another procedure is to have the child swallow a smooth tube to push the coin into the stomach, where it would pass through the intestine and out into the stool. An X-ray is taken afterwards to make sure that the coin is gone. If these are unsuccessful, the child will require removal of the coin under anesthesia.
- Surgery: The goals of the surgical procedure are different depending on the type of material swallowed, the length of time that has occurred since it was swallowed and how sick the child is.
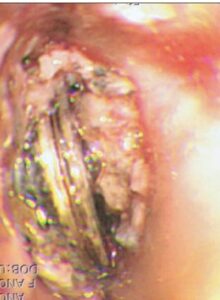 Esophagoscopy/upper endoscopy: Endoscopy is when a telescope is placed in the mouth and is gently pushed through the esophagus, stomach and part of the small intestine. The doctor can look at evidence of damage or injury directly. If there is an object stuck in the esophagus, it is removed during this procedure. The telescope used can be flexible or rigid, depending on what the child needs. The picture below shows damage in the esophagus from a disc battery stuck in the esophagus.
Esophagoscopy/upper endoscopy: Endoscopy is when a telescope is placed in the mouth and is gently pushed through the esophagus, stomach and part of the small intestine. The doctor can look at evidence of damage or injury directly. If there is an object stuck in the esophagus, it is removed during this procedure. The telescope used can be flexible or rigid, depending on what the child needs. The picture below shows damage in the esophagus from a disc battery stuck in the esophagus.- Bronchoscopy: In this procedure, a telescope is used to look at the airways—the vocal cords, voice box, windpipe and bronchus to assess for damage and possible stuck objects.
- Preoperative preparation: If there is a concern of a hole in the esophagus, antibiotics will be needed.
- Postoperative care:
- Foreign object with no damage to the esophagus: Most of the time, the child can be discharged from the hospital after the procedure, once he/she is able to swallow and eat without vomiting.
- Foreign object with damage to the esophagus: The care depends on the severity of injury. Patients with mild injuries may be discharged soon after the procedure. Patients with moderate injuries may require hospitalization for a few days with follow-up esophagram or esophagoscopy. Those with severe injuries will require hospitalization until the extent of the injury matures.
- Ingestion of hazardous materials: Depending on the findings, care may be minimal or may require hospitalization. Severe injuries may require stays in the intensive care unit.
- Esophageal injury
- Holes or perforation of the esophagus may require placement of drainage tubes or operations on the chest.
- Severe bleeding may require endoscopic procedures to or even surgical procedures to stop the bleeding.
- Scarring of the esophagus can cause blockage requiring future endoscopic or surgical procedures.
- Risks/Benefits:
- Risks: Esophagoscopy may cause injury of the esophagus. The child may aspirate saliva or contents of the stomach into the lungs.
- Benefits: Removal of a foreign body often gives immediate relief of symptoms. Endoscopy can show how bad the injury can be.
Home Care (“What do I need to do once my child goes home?”)
- Diet: After foreign body removal, children will often return to their normal diet. For deeper and more severe esophageal injuries, the child may require feeding through a tube or may only be allowed clear liquids or soft foods.
- Activity: Typically, activity can return to normal.
- Wound care: There will not be wounds for endoscopic procedures.
- Medicines: You may be given medicines for pain.
- What to call the doctor for: Call your surgeon or primary care physician for any difficulty swallowing, vomiting, fevers or for any wound problems.
- Follow-up care: Follow-up depends on the degree of damage to the esophagus. The more severe the damage, the more intense the follow-up would be.
Long-Term Outcomes (“Are there future conditions to worry about?”)
Scarring or narrowing of the esophagus is the most common long-term complication associated with moderate to severe esophageal injury. These may require dilations or in severe cases, resection or surgical replacement of the involved area.
Updated: 11/2016
Author: Michael B. Ishitani, MD
Editors: Patricia Lange, MD; Marjorie J. Arca, MD
This is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. Is a description of frequent practice and is not intended to be a definitive list of pediatric medical conditions.